To the Editor,
In Japan, the standard treatment approach for women with early-stage cervical cancer includes a radical hysterectomy with bilateral pelvic lymphadenectomy for stage IB–IIB disease [
1]. A benefit of surgery is that exploration allows surgeons to have an opportunity to assess the para-aortic lymph nodes (PANs) for metastasis. A recent survey study has shown that nearly 60% of Japanese Gynecologic Oncology Group (JGOG) institutions perform para-aortic lymphadenectomy for early-stage cervical cancer but there is a lack of universal indications for this procedure across their institutions [
2].
Given the relatively rare incidence of PAN metastasis in early-stage cervical cancer (3%–8%) [
34], identifying the predictors for PAN metastasis is crucial in the management of clinical stage IB–IIB cervical cancer. The objective of this study was to identify predictors of PAN metastasis at the time of surgical treatment for stage IB–IIB cervical cancer.
This is a retrospective study using data from a surgical tumor registry and includes consecutive cases of clinical stage IB–IIB cervical cancer who underwent radical hysterectomy at Tokai University School of Medicine between January 1976 and December 2014. Inclusion criteria were as follows: 1) histology types including squamous cell carcinoma, adenocarcinoma, and adenosquamous; and 2) lymphadenectomy sites including both pelvic and para-aortic chains. Exclusion criteria were cases that received neoadjuvant chemotherapy prior to radical hysterectomy, rare histology types, or if lymphadenectomy was only performed in the pelvic chain. Institutional Review Board approval was obtained at Tokai University, and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were used to outline the study [
5].
Among the eligible cases, clinico-pathological characteristics were abstracted from the medical record. In addition to pelvic lymph node (PLN) and PAN status, the following surgical-pathological factors were assessed: cervical stromal invasion (inner half vs. outer half), lympho-vascular space invasion (LVSI, yes vs. no), tumor size (>4 vs. ≤4 cm), uterine corpus invasion (yes vs. no), adnexal metastasis (yes vs. no), vaginal involvement (yes vs. no), and parametrial involvement (yes vs. no). In this study, we also assessed the pathological findings of surgical specimens from the parametrial tissue located at the origin of the internal iliac vessels.
Lymph node status included the number of sampled lymph nodes and the number of these that contained tumor cells. The lymph node ratio (LNR) was then determined as a percent proportion of tumor-involving lymph node per the total sampled lymph node for each case. Detailed qualities of PLN metastasis were further assessed for: common iliac node metastasis, bilateral PLN metastases, size of any metastasized PLN determined intraoperatively (cut-off, 1 cm), the presence of multiple PLN metastases, and high LNR (cut-off, 6.6%) [
6].
The primary focus of this analysis was to identify surgical-pathological factors for PAN metastasis. Secondary interest of analysis was surgical-pathological factors for parametrial tumor metastasis at the origin of internal iliac vessels. Chi-square or Fisher exact tests were used to assess statistical significance of categorical variables. A binary logistic regression model with conditional backward method was used to determine the independent predictors for PAN metastasis, and the magnitude of statistical significance was expressed with adjusted odds ratio (aOR) and 95% confidence interval (CI). Variance inflation factor was determined among the covariates entered in the model, and a value of ≥2 was interpreted as a presence of multicollinearity in this study. The Hosmer-Lemeshow test was used to assess the goodness of fit in the final model. All hypotheses were 2-tailed and a p<0.05 was defined as statistically significant. Statistical Package for Social Sciences (SPSS, version 24.0; IBM Corp., Armonk, NY, USA) was used for the analysis.
There were 555 cases identified from the surgical tumor registry, 498 of which were stage IB–IIB. Cases that underwent neoadjuvant chemotherapy were then excluded (n=51), leaving 447 cases of stage IB–IIB disease with primary surgical treatment. Among those, 19 cases of rare histology types and 316 cases with only pelvic lymphadenectomy without para-aortic lymphadenectomy were excluded. We then analyzed the remaining 112 case of surgically-treated stage IB–IIB cervical cancer without neoadjuvant chemotherapy and included both pelvic and para-aortic lymphadenectomy.
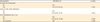
Patient demographics are shown in
Table 1. The median age was 53 years, and clinical stage II disease comprised nearly half of the study population (n=51, 45.5%). The median number of sampled PLN and PAN were 39.5 (interquartile range, 21) and 30 (interquartile range, 21), respectively. PAN metastasis was seen in 27 (24.1%; 95% CI=16.2–32.0) cases in this study.
On univariate analysis, negative PLN metastasis (proportion of PAN metastasis, yes vs. no, 31.8% vs. 0%, p<0.001) had a negative predictive value for PAN metastasis of 100%. LVSI (yes vs. no, 29.0% vs. 0%, p=0.026) and parametrial tumor involvement at the origin of internal iliac vessels (yes vs. no, 53.8% vs. 36.4%, p=0.004) were significantly associated with PAN metastasis. We were not able to perform multivariate analysis due to the absence of PAN metastasis in PLN-negative cases and LVSI-negative cases.
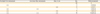
Quality and quantity metrics of PLN status were assessed for PAN metastasis. On univariate analysis, the presence of common iliac node metastasis (proportion of PAN metastasis, yes vs. no, 66.7% vs. 10.6%), bilateral PLN metastasis (52.2% vs. 4.5%), metastasized PLN size of ≥1 cm (54.8% vs. 10.3%), the presence of multiple PLN metastases (52.1% vs. 3.1%), and a LNR of ≥6.6% (63.2% vs. 4.1%) were statistically significantly associated with PAN metastasis (all p<0.001). In a multivariate model (
Table 2), the presence of common iliac lymph node metastasis (aOR=4.03; 95% CI=1.04–15.7; p=0.044), multiple PLN metastasis (aOR=7.35; 95% CI=1.27–42.6, p=0.026), and metastasized PLN size of ≥1 cm (aOR=8.92; 95% CI=2.30–34.6; p=0.002) remained independent predictors for PAN metastasis. There was no multicollinearity amongst these 3 covariates.
By utilizing these intraoperatively assessable PLN characteristics, the incidences of PAN metastasis were determined (
Table 3). When no risk factor was present, there was no case of PAN metastasis. With metastasized lymph nodes of ≥1 cm or multiple PLN metastases, the incidences of PAN were 16.7% and 18.2%, respectively. When 2 lymph node factors were present, the incidences of PAN ranged 28.6%–45.5%. When all 3 nodal factors were present, the incidence of PAN metastasis exceeded 80.0% (84.2%) (p<0.001).
As parametrial tumor involvement at the origin of the internal iliac vessels was significantly associated with increased risk of PAN metastasis, we examined the risk factors for parametrial tumor involvement at the origin of internal iliac vessels. On univariate analysis, only bilateral PLN metastasis was significantly associated with parametrial tumor involvement at the origin of internal iliac vessels (50.0% vs. 9.1%; odds ratio [OR]=10.0; 95% CI=1.10–90.8; p=0.027). With tumor involvement in parametrial tissue of the hysterectomy specimen, there was an increased risk of parametrial tumor involvement at the origin of internal iliac vessels although it did not reach statistical significance (57.1% vs. 23.8%; OR=4.27; 95% CI=0.99–18.4; p=0.075).
Identification of PAN metastasis impacts not only patient counseling for prognosis but also for postoperative treatment. As para-aortic lymphadenectomy during radical hysterectomy can increase both surgical and post-operative morbidity related to the procedure, selective rather than universal para-aortic lymphadenectomy in women at increased risk for para-aortic metastasis is an ideal approach to reduce procedure-related complications.
PLN metastasis is a well-known factor for PAN metastasis. In this study, we not only validate the location, size, and quantity of PLN metastasis as predictors of PAN metastasis, we but also provided combined quality and quantity metrics of PLN metastasis to assess the incidence of PAN metastasis. All these parameters are assessable during the surgery (
Table 3), making the utility of this study useful in daily practice.
In this study, we found that more than half of the cases with parametrial tumor involvement in the hysterectomy specimen had tumor involvement in the parametrial tissue near the internal iliac origin (57.1%). Tumor involvement in this anatomical location was also associated with PLN and PAN metastasis. This association not only supports a hypothesis of lymphatic tumor spread via parametrial, pelvic, and PANs but also determines the treatment intervention in stage IIB disease. Given the comparable effectiveness on survival [
7], if chemotherapy rather than radiotherapy is considered for adjuvant treatment in high-risk patients, 1) assessment of tumor involvement in the lateral parametrium at the origin of internal iliac vessels and 2) complete resection in necessary case would be paramount because chemotherapy alone may not have adequate local control in the pelvis in high-risk group [
7]. In this setting, laterally-extended parametrectomy (LEP) procedure may be an option for surgical treatment in node-positive early-stage cervical cancer [
89]. Morbidity related to this extended surgical procedure was not available in our study, and further study is warranted to assess the risks and benefits related to LEP.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download