Abstract
Purpose
Although there are several surgical methods for treatment of sacrococcygeal pilonidal sinus, there is no widespread consensus. In this study, we aimed to compare primary closure, Limberg, and modified Limberg flap techniques, with each performed by each of 3 surgeons.
Methods
A total of 802 patients who were operated on for pilonidal sinus disease were included in this retrospective cohort study. Patients were evaluated in 3 groups: group 1 (limited excision + primary closure), group 2 (large excision + Limberg flap technique), and group 3 (large excision + modified Limberg technique). Development of early or late period complications was accepted as primary outcome.
Results
Mean patient age was 28.1 ± 6.7 years. Operation time in group 1 was 44.0 ± 14.5 minutes, and was shorter in comparison to other 2 groups (P < 0.001). One or more complications developed in 171 patients (21.3%) within study group. Highest complication rate was in group 1, with a rate of 30.7% (P < 0.001). Rate of wound dehiscence and recurrence in group 1 were differed significantly from other groups (P < 0.001 and P = 0.001, respectively).
Go to : 
Pilonidal sinus disease (PSD) is a common chronic disease that generally affects young adults below the age of 45. It is most commonly observed at the intergluteal region, though it may also affect other sites like the umbilicus and the interdigital area, particularly among in barbers. The disease was long thought to be either congenital or acquired; although in recent years it has been more widely viewed as an acquired disease [1]. The etiology of PSD is not fully understood, however, the most important cause is believed to be fallen hairs accumulating within skin folds and implanting within the skin. The skin becomes more prone to maceration, sweating and bacterial contamination, which facilitates implantation of fallen hairs, creating the necessary conditions for development of the disease. Although PSD is a benign disease, it produces symptoms such as pain and discharge, which adversely affect patient quality of life [23].
There are many approaches for treatment of the disease, including several surgical methods such as limited or large excision, primary closure, or flap techniques, and many other nonsurgical methods. However, no consensus has been reached regarding the ideal treatment method. An ideal surgical treatment reduces recurrence and complication rates, and allows for minimal hospitalization and rapid return to daily activities [4]. Among patients treated using the limited excision and primary closure method, the presence of a natal cleft is associated with higher morbidity, resulting in recurrence rates of 7%–42%. For techniques that use the flap approach, this rate decreases to 0%–3% [3]. In patients undergoing the Rhomboid excision and Limberg flap techniques, which require a larger surgical area compared to the limited excision and primary closure methods, complication rates are lower, and length of hospital-stay and time to return to work are reduced [56]. However, using the classical Limberg flap technique, maceration and scar formation due to sutures in the intergluteal sulcus, and the accumulation of hair at the midline may result in recurrence. Application of a modified Limberg technique that includes lateralization of the middle line can help reduce wound complications and recurrence rates [7]. Several publications report contradicting results regarding surgical outcomes using the same technique, which may be attributable to differences in practice between surgeons [89]. Therefore, it can be logical to explore the superiority of any type of surgical technique, each performed by a single, separate and experienced surgeon for the surgical treatment of PSD.
In this study, we compared limited excision-primary closure, Limberg, and modified Limberg flap techniques, each performed by each of the three surgeons, in terms of postoperative outcomes and recurrence rates.
Go to : 
Institutional Review Board approval was taken from Buyukcekmece State Hospital with an approval number of 2011/01-08. Written consent could not be taken from the patients due to the retrospective design of the study. The study was performed in accordance with the Declaration of Helsinki. The study was registered to the research registry with an ID number of researchregistry1,458 and to the clinicaltrials.gov with an ID number of NCT02849197.
A total of 1,082 patients who were diagnosed with PSD and who underwent surgical treatment in a governmental hospital between January 2011 and June 2015 were included in this retrospective observational study. The patients with incomplete personal and medical data and who could not be contacted by direct interview or by telephone were excluded (n = 280). Direct interview and telephone contact were performed by the medical auxiliary personnel rather than the surgeons. Therefore, the study group consisted of 802 patients.
Age, sex, and operation data (surgical technique, operation time) were recorded by retrospectively reviewing patient files in the hospital information system between January 2011 and June 2015. Early period complications (wound site infection, wound dehiscence, abscess, hematoma and seroma formation) developing within 30 days of operation was recorded from the medical files that include information regarding the postdischarge period. Those patients who did not report of a follow-up visit were contacted by phone between June 2015 and August 2015 and questioned regarding chronic pain, recurrence and possible surgical intervention.
Wound site infection was defined as erythema at the wound site; seroma and hematoma were defined as accumulation of fluid or blood at the wound site, requiring aspiration or drainage; recurrence was defined as the development of sinus openings or the presence of discharge at the wound site in the absence of wound infection; and chronic pain was defined as the presence of pain or other conditions expressed by the patient and producing discomfort at the operation area during daily activities.
For patients undergoing elective operations, 3 different surgical methods were performed by in the general surgery clinic. All of the surgeons were experienced in general surgical procedures at least more than 5 years. Patients were evaluated in 3 groups as group 1 (limited excision + primary closure), group 2 (large resection + Limberg flap technique), and group 3 (large excision + modified Limberg flap technique). The decision on the type of surgical technique was independent from the patient's condition. Each technique was performed by each of the three surgeons.
Patients were placed under spinal anesthesia and oriented in a jack-knife position. Each patient was treated with ampicillin + sulbactam (Duocid, 1 g, IM/IV vial; Pfizer, Istanbul, Turkey) as an antibiotic prophylaxis.
An elliptical incision was made, and the excision included sinus openings at the median line and extended down to the presacral fascia. One suction drain was placed in the wound cavity. Subcutaneous tissue was approximated with interrupted 2-0 absorbable suture, and skin was closed with interrupted 2-0 silk suture.
A rhomboid incision was made as to include all sinus openings, and an excision was made down to the presacral fascia. A bisector drawn in the rhombohedron was extended laterally to a length similar to that of a corner of the rhombohedron. Then, the flap was prepared by removing gluteal muscle with its fascia. One suction drain was placed at the wound cavity. The base of the flap was approximated with the presacral fascia at the excised area with interrupted 2-0 absorbable sutures. Subcutaneous tissue was approximated with interrupted 2-0 absorbable sutures, and the skin was closed with interrupted 3-0 prolene suture.
As in Limberg flap technique, a rhomboid incision was made. Upper and lower corners of the excision were lateralized 2 cm away from the midline in order to keep the suturing line at the inferior from overlapping the midline. An excision was made down to the presacral fascia. One suction drain was placed at the wound cavity, and the base of the flap was approximated with the presacral fascia at the excised area with interrupted 2-0 absorbable sutures. Subcutaneous tissue was approximated with interrupted 2-0 absorbable suture, and the skin was closed with 3-0 prolene.
Drains were kept in place until the amount of daily drainage dropped below 20 mL. Sutures were removed on postoperative day 10. All patients received oral antibiotic treatment (ampicillin + sulbactam, Duocid, 375 mg; Pfizer) for 5 days postoperatively. Oral antibiotic treatment was continued in those patients who developed wound site infection. Drainage was performed in patients who developed abscess and hematoma. Drainage or compression bandage was applied in patients who developed seroma.
Development of any complication either early or late was regarded as the main outcome. Data were analyzed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are expressed as mean ± standard deviation while noncontinuous variables are expressed as frequency and percentage. A comparison of groups regarding age, operation time and follow-up time was made with one way analysis of variance (1-way analysis of variance) test. When a difference was detected, multiple comparisons were performed with post-hoc Tukey test in order to determine the group(s) that differed significantly. A Pearson chi-square test was used in order to compare distribution of sex and complication rates across groups. Differences were accepted as significant at P < 0.05 within 95% confidence interval.
Go to : 
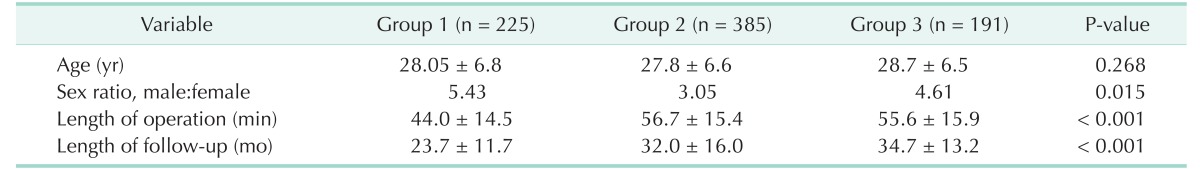
The mean age of patients was 28.1 ± 6.7 years and the male:female ratio was 3.9. The groups were similar in terms of age distribution (P = 0.268). The male/female ratio in group 2 was significantly lower compared to the other groups (P = 0.015) (Table 1). Operation time in group 1 (44.0 ± 14.5 minutes, P < 0.001) was significantly shorter than in the other 2 groups. Operation time did not differ between groups 2 and 3 (P = 0.690).
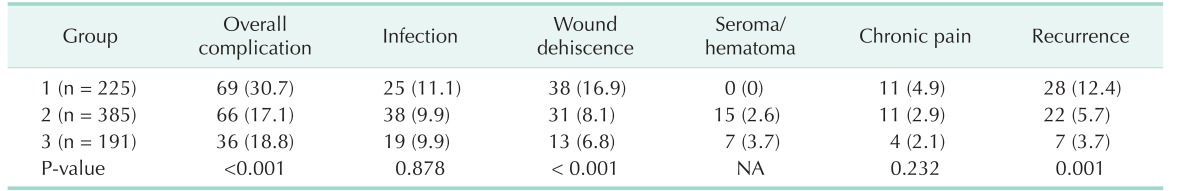
One or more complications developed in 171 patients (21.3%) within the study group. Group 1 had the highest complication rate at 30.7% (P < 0.001) (Table 2).
The rate of wound site infection was 10.2% and there was no difference between the groups (P = 0.878). In group 1, wound dehiscence and recurrence rates were 16.9% and 12.4%, respectively, and these rates were significantly higher in group 1 compared to the other groups (P < 0.001 and P = 0.001, respectively). Rates of other complications did not differ between the groups (Table 2). Mean follow-up time was 23.7 ± 11.7 months in group 1, and was significantly shorter in comparison to the other 2 groups (P < 0.001) (Table 1).
Go to : 
PSD is a commonly observed infectious entity, occurring more frequently among males and young adults. Although it is a benign disease, it is associated with significant morbidity and loss of work force [110]. The mean age (28.1 ± 6.7 years) and male:female ratio (3.9) of the patient cohort examined in the present study are consistent with the literature data. Although group 2 included significantly more female patients, it was not possible to identify the cause of this difference or identify any possible effects on the outcomes.
Some risk factors have been defined for PSD, including growing hair, driving more than 4 hours a day, family history, and bathing less than 3 times per week. While obesity does not increase the risk of PSD, it is considered a risk factor for recurrence and development of postoperative complications [1112]. Genetic susceptibility is described as a risk factor for early onset of disease and early development of symptoms, and additionally for recurrence risk [1113]. The number of sinuses is not associated with disease course [11]. Although knowledge of clinicopathologic variables including body mass index, American Society of Anesthesiologist physical status classification and other parameters with regard to PSD may help surgeons to reproduce their performance in relation with safety of patients, it was not possible to evaluate these variables due to the absence of accurate data in all patients in this retrospective study.
The continuing presence of a median line (natal cleft) after simple closure of the PSD is associated with high rates of adverse outcomes such as wound site infection and recurrence [14]. Muzi et al. [15] reported a high rate of wound site infection with primary closure, whereas rates of recurrence and wound dehiscence did not differ significantly in comparison to the Limberg flap technique. However, Dass et al. [16] found high rates of wound dehiscence, infection and recurrence with primary closure, whereas rates of seroma and hematoma were higher with the rhomboid flap technique. A meta-analysis by McCallum et al. [12] reported a recurrence rate with primary closure of 11%. In this study, the recurrence rate with primary closure was 12.4%. Some studies have reported recurrence rates of up to 21% using the primary closure technique [81718]. Studies using the Limberg flap technique report recurrence rates of about from 0% to 5%, however these studies differ substantially in the amount of follow-up time [13]. In the study of Zorlu et al. [19], there was only one recurrence among 40 patients (2.4%) with Limberg flap at the sixth month control. In our study, the recurrence rate with Limberg flap technique was 5.7% at the end of follow-up (mean, 32 months). Although this rate is close to upper ranges reported in previous studies, we believe long-term follow-up in our study group impacted the results. In a study including 94 patients, Kaya et al. [18] reported the recurrence rate using a modified Limberg technique as 4.2%, whereas another study by Shabbir et al. [14] reported a recurrence rate of 3.3%. In this study, we found a recurrence rate of 3.7% over a mean follow-up time of 34.7 months, which is consistent with the literature data. Considering these rates, it could be concluded that the outcomes of the surgical techniques performed in this study are consistent with the literature data, particularly with regard to recurrence.
Following surgical treatment of pilonidal sinus, wound problems, complications and recurrence are more likely to develop along the median line and at the lower end of the incision. Higher morbidity observed after primary closure is due to the continuing presence of median line and the vacuum effect on this area, which creates conditions that promote recurrence [20]. In the Limberg flap method, wound problems and recurrence are more likely to develop at the lower end. For this reason, lateralization of the lower end in the modified Limberg method is associated with lower recurrence rates [21]. We believe the modified Limberg technique, which yielded a lower recurrence rate in our study, reduces complications such as wound site infection and wound dehiscence by eliminating the median line and lateralization of the lower end, and thus aids in increasing patient comfort. Although not statistically significant, the recurrence rate was lowest in the modified Limberg method, which could be regarded as another advantage to this technique.
Previous studies have compared open and primary closure techniques to other closure methods in terms of wound site infection, and these techniques have been associated with markedly increased wound site infection rates [5810]. While wound site infection rates vary between 1.93%–11.45% after primary closure technique, lower rates have been reported when using flap techniques, and it is thought that recurrence is correlated with wound site infection [89]. However, in this study, although the wound site infection rate was higher with primary closure compared to other groups, the difference was not statistically significant.
Some studies have found no difference between flap techniques and primary closure in terms of complications such as hematoma, seroma, wound site infection, and recurrence [6]. However, we found higher rates of complication and recurrence among patients who underwent surgery using the primary closure technique. It is difficult to control all the variables associated with surgical technique, patient, and disease, and therefore similar studies may reach different conclusions.
Some studies have reported that the placement of a drain does not have any effect on the risk of hematoma, infection or wound healing [22]. However, placement of a drain, especially when using the flap techniques, reduces the rate of wound dehiscence, wound site infection and hematoma development [23]. Since drain was placed in all patients in our study, we could not evaluate the effect of drain utilization in pilonidal sinus surgery. There is no scoring system defined for preoperative and postoperative periods in pilonidal sinus surgery; therefore it is difficult to compare the results of different studies in a standard fashion. Nevertheless, there is a generally accepted opinion that surgical methods that involve closure of the wound should be preferred over the techniques that involve leaving the wound open [6]. The ideal treatment method for PSD should be the simplest method with the lowest rate of recurrence and lowest complication rate, shortest hospital stay, and lowest cost [1]. Flap techniques are associated with low recurrence, fewer wound problems and complications, and rapid healing and may therefore be regarded as the preferred surgical option. However, it should be noted that flap techniques have some additional risks including surgical scarring and anesthesiarelated complications [9]. Postoperative numbness causing patient dissatisfaction may be regarded as an important issue for selecting flap techniques including Limberg and modified Limberg methods [2425]. It has been reported that 19% of the patients with primary PSD treated with Limberg transposition flap reported numbness at the operation site and more than half of them (63%) were not pleased with cosmetic appearance of the scars [25]. Therefore, superiority of flap techniques may be regarded as questionable if such complications are considered for the evaluation of surgical methods of PSD.
Studies that involve different surgical techniques for treatment of PSD have reported contradicting results in terms of recurrence rates. Likewise, it is not always possible to confirm the results obtained in comparative studies. The inability to control variables related to surgical technique, patients, and disease often contributes to a high level of variation between studies. Factors related to surgical technique, patients, and disease may have a strong effect on recurrence rates following surgical treatment of PSD. In this study, each surgical method was performed by each of the 3 surgeons; we believe that it would have eliminated the confounding effects of the surgical technique to a great extent. It has been thought that the expertise on one type of surgery improves the outcome of that surgery i.e., inguinal hernia. Additionally, higher volume of that specific type of surgery which is performed by experienced surgeons is another important issue. Therefore, the single surgeon experience gathered by performing one type of surgery on a specific disease may have a positive impact for diminishing confounding variables. In addition, controlling for other variables associated with patient and disease status may be necessary to clarify discrepancies between studies and to improve the outcome of the technique.
Retrospective design was the main limitation of the study. For the formation of the groups, no application of any randomization or another approach was another limitation. In conclusion, it was found that Limberg and modified Limberg methods, each performed by a single, separate and experienced surgeon are superior to the primary closure method in pilonidal sinus surgery in terms of the rates of general complications, wound dehiscence, and recurrence.
Go to : 
References
1. Tavassoli A, Noorshafiee S, Nazarzadeh R. Comparison of excision with primary repair versus Limberg flap. Int J Surg. 2011; 9:343–346. PMID: 21354343.

2. Osmanoglu G, Yetisir F. Limberg flap is better for the surgical treatment of pilonidal sinus. Results of a 767 patients series with an at least five years follow-up period. Chirurgia (Bucur). 2011; 106:491–494. PMID: 21991875.
3. Akca T, Colak T, Ustunsoy B, Kanik A, Aydin S. Randomized clinical trial comparing primary closure with the Limberg flap in the treatment of primary sacrococcygeal pilonidal disease. Br J Surg. 2005; 92:1081–1084. PMID: 16078300.

4. Akin M, Leventoglu S, Mentes BB, Bostanci H, Gokbayir H, Kilic K, et al. Comparison of the classic Limberg flap and modified Limberg flap in the treatment of pilonidal sinus disease: a retrospective analysis of 416 patients. Surg Today. 2010; 40:757–762. PMID: 20676861.

5. Khan PS, Hayat H, Hayat G. Limberg flap versus primary closure in the treatment of primary sacrococcygeal pilonidal disease; a randomized clinical trial. Indian J Surg. 2013; 75:192–194.

6. Horwood J, Hanratty D, Chandran P, Billings P. Primary closure or rhomboid excision and Limberg flap for the management of primary sacrococcygeal pilonidal disease? A meta-analysis of randomized controlled trials. Colorectal Dis. 2012; 14:143–151. PMID: 20969718.

7. Akin M, Gokbayir H, Kilic K, Topgul K, Ozdemir E, Ferahkose Z. Rhomboid excision and Limberg flap for managing pilonidal sinus: long-term results in 411 patients. Colorectal Dis. 2008; 10:945–948. PMID: 18462233.
8. Ozer S, Karaca T, Bilgin BC, Demir A, Ozer H, Ertas E. Comparison of recurrence between marsupialization, primary repair, limberg flap methods for pilonidal sinus disease. Turk J Colorectal Dis. 2012; 22:10–16.
9. Mentes O, Bagci M, Bilgin T, Coskun I, Ozgul O, Ozdemir M. Management of pilonidal sinus disease with oblique excision and primary closure: results of 493 patients. Dis Colon Rectum. 2006; 49:104–108. PMID: 16283563.

10. Enshaei A, Motearefi S. Comparison of two surgical methods, primary closure and rotational flap, in patients with chronic pilonidal sinus. Glob J Health Sci. 2014; 6(7 Spec No):18–22. PMID: 25363174.

11. Hosseini SV, Bananzadeh AM, Rivaz M, Sabet B, Mosallae M, Pourahmad S, et al. The comparison between drainage, delayed excision and primary closure with excision and secondary healing in management of pilonidal abscess. Int J Surg. 2006; 4:228–231. PMID: 17462356.

12. McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ. 2008; 336:868–871. PMID: 18390914.

13. Karaca AS, Ali R, Capar M, Karaca S. Comparison of Limberg flap and excision and primary closure of pilonidal sinus disease, in terms of quality of life and complications. J Korean Surg Soc. 2013; 85:236–239. PMID: 24266015.

14. Shabbir F, Ayyaz M, Farooka MW, Toor AA, Sarwar H, Malik AA. Modified Limberg's flap versus primary closure for treatment of pilonidal sinus disease: a comparative study. J Pak Med Assoc. 2014; 64:1270–1273. PMID: 25831644.
15. Muzi MG, Milito G, Cadeddu F, Nigro C, Andreoli F, Amabile D, et al. Randomized comparison of Limberg flap versus modified primary closure for the treatment of pilonidal disease. Am J Surg. 2010; 200:9–14. PMID: 20637332.

16. Dass TA, Zaz M, Rather A, Bari S. Elliptical excision with midline primary closure versus rhomboid excision with limberg flap reconstruction in sacrococcygeal pilonidal disease: a prospective, randomized study. Indian J Surg. 2012; 74:305–308. PMID: 23904719.

17. Ersoy OF, Karaca S, Kayaoglu HA, Ozkan N, Celik A, Ozum T. Comparison of different surgical options in the treatment of pilonidal disease: retrospective analysis of 175 patients. Kaohsiung J Med Sci. 2007; 23:67–70. PMID: 17339168.

18. Kaya B, Eris C, Atalay S, Bat O, Bulut NE, Mantoglu B, et al. Modified Limberg transposition flap in the treatment of pilonidal sinus disease. Tech Coloproctol. 2012; 16:55–59. PMID: 22170253.

19. Zorlu M, Sahiner IT, Zobaci E, Kocak C, Yasti AC, Dolapci M. Early results with the Mutaf technique: a novel off-midline approach in pilonidal sinus surgery. Ann Surg Treat Res. 2016; 90:265–271. PMID: 27186571.

20. Colak T, Turkmenoglu O, Dag A, Akca T, Aydin S. A randomized clinical study evaluating the need for drainage after Limberg flap for pilonidal sinus. J Surg Res. 2010; 158:127–131. PMID: 19394643.

21. Mentes BB, Leventoglu S, Cihan A, Tatlicioglu E, Akin M, Oguz M. Modified Limberg transposition flap for sacrococcygeal pilonidal sinus. Surg Today. 2004; 34:419–423. PMID: 15108080.

22. Erdem E, Sungurtekin U, Nessar M. Are postoperative drains necessary with the Limberg flap for treatment of pilonidal sinus? Dis Colon Rectum. 1998; 41:1427–1431. PMID: 9823811.

23. Tocchi A, Mazzoni G, Bononi M, Fornasari V, Miccini M, Drumo A, et al. Outcome of chronic pilonidal disease treatment after ambulatory plain midline excision and primary suture. Am J Surg. 2008; 196:28–33. PMID: 18565338.

24. el-Khadrawy O, Hashish M, Ismail K, Shalaby H. Outcome of the rhomboid flap for recurrent pilonidal disease. World J Surg. 2009; 33:1064–1068. PMID: 19198934.

25. Eryilmaz R, Sahin M, Alimoglu O, Dasiran F. Surgical treatment of sacrococcygeal pilonidal sinus with the Limberg transposition flap. Surgery. 2003; 134:745–749. PMID: 14639351.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download