Abstract
Purpose
Recently, transoral endoscopic thyroidectomy (TOET) is receiving attention because it is regarded as a true minimally invasive surgery in that it does not leave scars on any part of the body and the area of flap dissection is similar to that of open surgery. In this study, we present the surgical procedures and initial outcomes of TOET in the treatment of papillary thyroid microcarcinoma (PTMC) patients.
Methods
The medical records of patients who underwent TOET for PTMC between July 2016 and February 2017 were retrospectively reviewed. Indication of TOET was PTMC without capsular invasion or lymph node metastasis on preoperative imaging studies.
Results
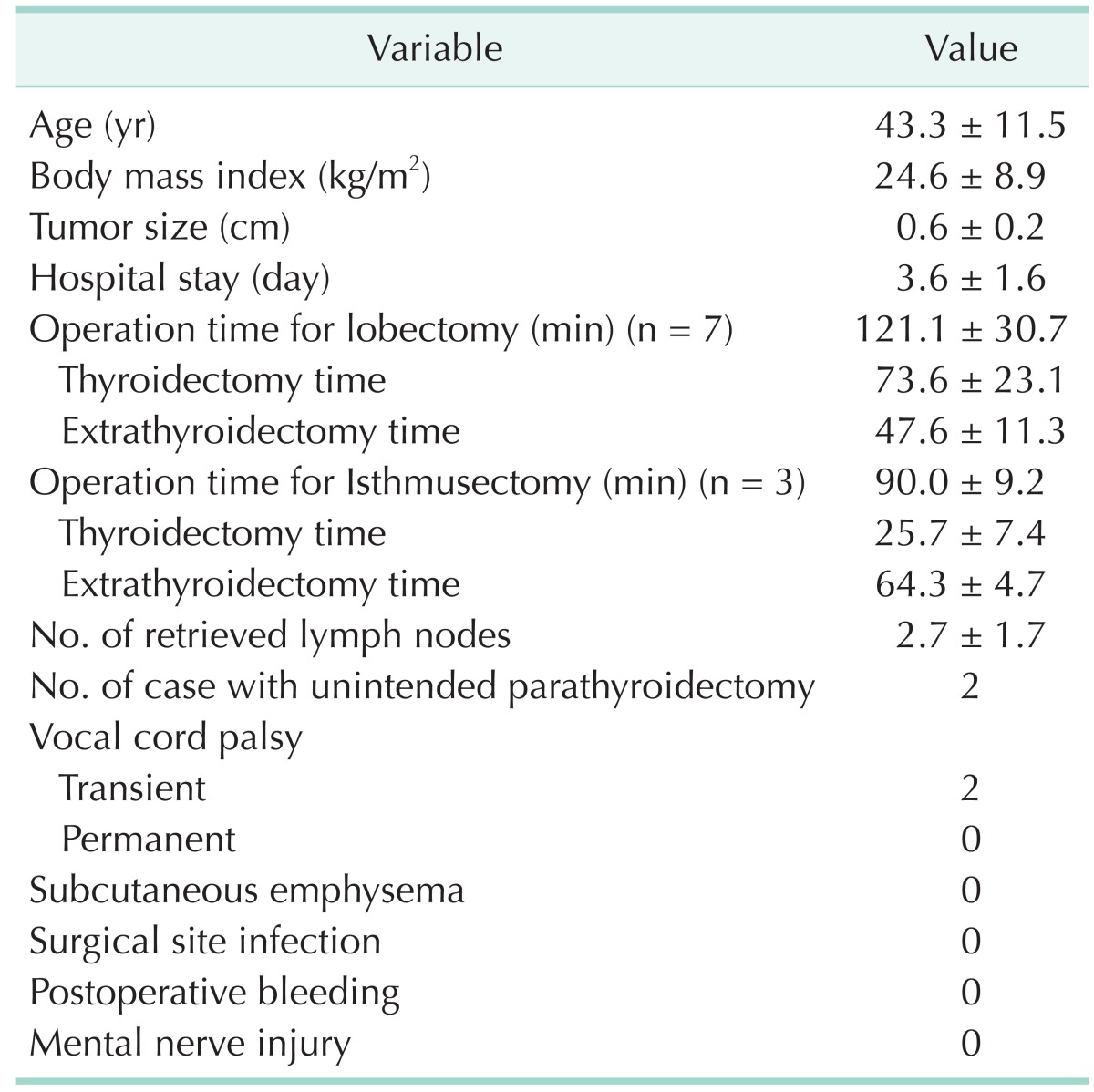
Ten female patients were enrolled. Seven patients underwent thyroid lobectomy and three patients underwent isthmusectomy. The mean age and tumor size was 43.3 ± 11.5 years and 0.6 ± 0.2 cm, respectively. Operation time for lobectomy and isthmusectomy was 121.1 ± 30.7 (range, 65–148) and 90.0 ± 9.2 minutes (range, 82–100 minutes), respectively. The mean number of retrieved lymph nodes was 2.7 ± 1.7. Two patients had transient vocal cord palsy, which recovered in three months. There was no case with subcutaneous emphysema, surgical site infection, postoperative bleeding, or mental nerve injury.
Various remote-access approaches for thyroid surgery such as transaxillary, axillo-breast, subclavian, and retro-auricular approaches have been developed to avoid a neck scar caused by the conventional Kocher incision [1234]. However, remote-access approaches leave significant scarring and require extensive flap dissection to access the thyroid gland. On the contrary, the transoral approach to thyroid surgery is receiving attention as it is regarded as truly minimally invasive because it does not leave scars on any part of the body and the area of flap dissection is similar to that of open surgery.
In 2008, the first transoral approach for thyroid surgery was performed successfully via the mouth floor in living pigs in Germany [5], and this approach has since been applied in human patients [67]. However, the transoral approach through the mouth floor did not become popular and was even prohibited by German authorities due to its high complication and conversion rates [67]. The most severe complication related to this approach was mental nerve injury, which was due to the excessive tissue dissection in the mouth floor. To overcome the complications related to mouth floor dissection, a transvestibular approach was developed in 2009 [8]. In general, the transvestibular approach uses 3 vestibular ports without a mouth floor port [9]. A camera is introduced through the midline port, and the lateral 2 ports are used for an energy-based device or endoscopic instruments. Recently, the transvestibular approach has gained popularity worldwide since a study reported successful outcomes in 60 patients undergoing endoscopic thyroidectomy using the transvestibular approach [10].
In this study, we present the step-by-step procedures and initial outcomes of transoral endoscopic thyroidectomy (TOET) in the treatment of papillary thyroid microcarcinoma (PTMC, papillary thyroid carcinoma ≤ 1.0 cm) patients.
The medical records of patients who underwent TOET for the treatment of PTMC between July 2016 and February 2017 at Seoul Metropolitan Government - Seoul National University Boramae Medical Center were retrospectively reviewed. The operation was performed by a single surgeon (YJC). Indication of TOET was PTMC requiring lobectomy or isthmusectomy. PTMC with suspicious capsular invasion or lymph node metastasis on the preoperative imaging studies were not indicated for TOET. Eligible patients were counselled on the advantages and disadvantages of TOET in detail before electing TOET. The institutional review board at Seoul Metropolitan Government - Seoul National University Boramae Medical Center approved this study (approval number: H-16-2017-25).
Preoperative ultrasound and CT scan were performed routinely for the evaluation of tumor and lymph node status. Patients were admitted to the ward the day before surgery and underwent indirect laryngoscopic examination for vocal cord evaluation. Prophylactic antibiotics were administered 30 minutes before surgery (Cefotetan 1 g).
Patients were placed in a supine position with slight neck extension, such as in open thyroidectomy. EMG endotracheal tube (Medtronic, Jacksonville, FL, USA) was intubated transorally for intraoperative neural monitoring (IONM) and fixed at the midline (Fig. 1). After draping, the oral cavity was cleansed and irrigated with a chlorhexidine solution. Three linear incisions (midline, 2 cm; lateral, 5 mm) were made in the lower lip. A midline incision was made at 1 cm above frenulum of the lower lip and lateral incisions were made at 1 cm medial to the mouth angle (Fig. 1B). Through the incisions, a total of 30 mL of dilute epinephrine-saline solution (1:200,000) were injected into the subplatysmal space using Veress needle. Then, we inserted an 8-mm-sized vascular tunneler through the midline incision and dissected the subplatysmal to create working space. One 10-mm and two 5-mm trocars were inserted through the midline and lateral incisions, and CO2 gas was insufflated at 6 mmHg pressure with high flow. We inserted a 10-mm 30° 4K camera (Synergy UHD4, Arthrex Inc., Naples, FL, USA) through the midline trocar, and laparoscopic instruments through lateral incisions for further flap dissection.
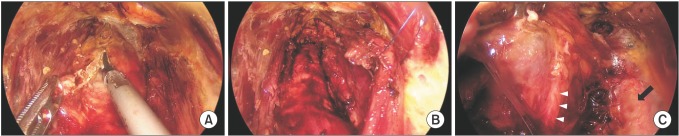
After creating working space from the thyroid cartilage to the sternal notch and to the medial border of bilateral sternocleidomastoid muscles, the midline of the strap muscles was divided. Then, we divided the isthmus (Fig. 2A). In the isthmusectomy cases, we excised the isthmus with a margin of surrounding normal thyroid tissue to as much as 120 degrees of the anterior trachea. To obtain wider space at the lateral aspect of the thyroid gland, we placed a stitch around the strap muscles and retracted from the outside using 3/0 Nylon (Fig. 2B). We lifted the superior pole of the thyroid gland and ligated superior thyroidal vessels with a Harmonic ACE +7 (Ethicon, Cincinnati, OH, USA). Then, we dissected adjacent soft tissues preserving the superior parathyroid gland, and reflected the thyroid to identify the recurrent laryngeal nerve (RLN). IONM was routinely performed either to identify or confirm RLN. After identifying RLN at its entry point (Fig. 2C), we dissected the thyroid gland from the trachea preserving the inferior parathyroid gland. Ipsilateral prophylactic central neck dissection was performed routinely.
The resected specimen was placed into an endoplastic bag and extracted through the midline port. The muscle layer of the midline incision was sutured tightly with interrupted 4/0 absorbable suture. Oral mucosa was closed gently with interrupted 4/0 absorbable suture. We did not insert a drain for thyroid lobectomy as in open thyroidectomy.
The patients were discharged on the second or third postoperative day and intravenous antibiotics were maintained for an additional 2 or 3 days after the operation. Patients started water intake 4 hours after operation and normal regular diet on the first postoperative day. Patients visited the outpatient clinic 2 weeks after discharge for immediate postsurgical care and stitch removal. Follow-up examinations were performed at 3 and 6 months thereafter.
Operation videos were reviewed and the operation time was divided into thyroidectomy time and extrathyroidectomy time. Thyroidectomy time was the time from midline division of strap muscle to trocar removal, and extrathyroidectomy time was the remaining thyroidectomy time, which included the time spent for incision, tunneling, flap dissection, and closure.
Mental nerve was evaluated in ward and outpatient clinic. Patients were asked whether they had numbness around the chin or the lower lip. We also applied alcohol swab around the chin to check for sensory deficit. A routine indirect laryngoscopic examination was performed preoperatively and at the first outpatient clinic visit. Laryngoscopic examinations were repeated in patients with vocal cord palsy until the vocal cord movement normalized. Vocal cord palsy lasting less than 6 months was defined as transient.
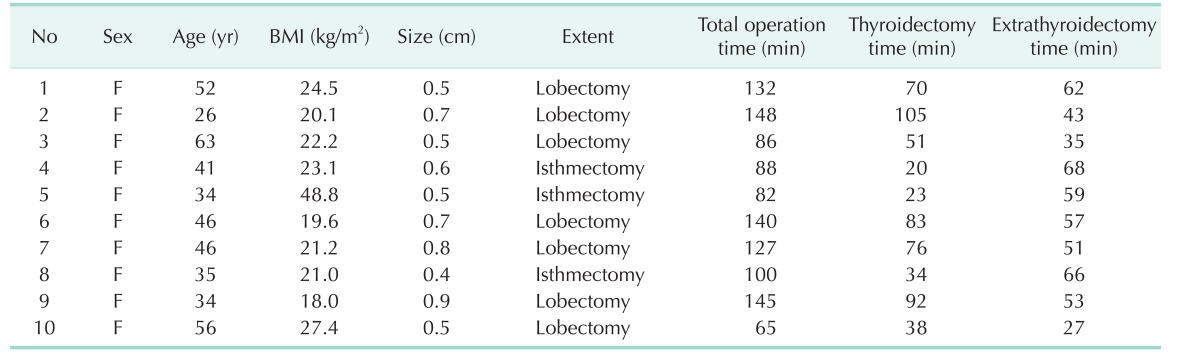
A total of 10 female patients were enrolled (Table 1). The mean age was 43.3 ± 11.5 years and the mean body mass index was 24.6 ± 8.9 kg/m2. Seven patients underwent thyroid lobectomy and 3 patients underwent isthmusectomy. Mean tumor size was 0.6 ± 0.2 cm. Total operation time ranged 65 to 148 minutes.
Table 2 demonstrates surgical outcomes of the study patients. Operation time for lobectomy and isthmusectomy was 121.1 ± 30.7 and 90.0 ± 9.2 minutes, respectively. The mean thyroidectomy time of lobectomy and isthmusectomy was 73.6 ± 23.1 and 25.7 ± 7.4 minutes, respectively. The mean extrathyroidectomy time of lobectomy and isthmusectomy was 47.6 ± 11.3 and 64.3 ± 4.7 minutes, respectively. The mean number of retrieved lymph nodes was 2.7 ± 1.7. Two patients had transient vocal cord palsy, and vocal cord movement recovered within 3 months after the operation. There was no case with subcutaneous emphysema, surgical site infection, or postoperative bleeding. No patient had mental nerve injury. There was also no complication related to the transoral approach such as flap perforation or lip tearing.
This study is the largest case series of TOET for thyroid carcinoma patients after a study of Wang et al. that also reported 10 cases of papillary thyroid carcinoma patients [11]. We have set strict indications for TOET as it was in the initial cases. We selected female patients who had PTMC without capsular invasion or lymph node metastasis which required lobectomy or isthmusectomy. We did not include male patients because the prominent thyroid cartilage may hamper instrument manipulation. We also limited the application of TOET to the PTMC patients without capsular invasion or lymph node metastasis because small tumors are easy to manipulate and achieve oncological safety. As there are studies in which PTMC patients without invasion or lymph node metastasis may not require thyroidectomy [1213], we discussed the pros and cons of observation versus TOET or open thyroidectomy with the patients before surgery. In cases of PTMC in the isthmus, we performed wide isthmusectomy based on the evidences from previous studies [1415]. We had applied TOET selectively to lobectomy or isthmusectomy cases in order not to cause serious complications such as bilateral RLN injury or permanent hypoparathyroidism. When more experience is gained, the indication may be extended to total thyroidectomy. Indeed, TOET has been performed safely in Graves' disease and secondary hyperparathyroidism by experienced hands [1617].
The operation time shown in this study (range, 65–148 minutes) was not significantly long compared to conventional open thyroid surgery considering that this was a totally new experience. The operator was an experienced surgeon in the bilateral axillo-breast approach and visited Dr. Anuwong in Thailand twice to observe more than 10 cases. Therefore, it might take a longer operation time for surgeons without experience in remote-access surgery using CO2 insufflation. However, the operation time is likely to be reduced in both extrathyroidectomy and thyroidectomy times as surgeons accumulate experience. To reduce the extrathyroidectomy time, proper subplatysmal injection and tunneling is important. Subplatysmal flap dissection could be tricky and bleeding from the flap or anterior jugular vein significantly extends the operation time. In this study, the flap was easily dissected without bleeding in most of the cases with short extrathyroidectomy time. In the thyroidectomy time, one of the most difficult problems was collision between instruments. In particular, collision between the camera and the laparoscopic instruments made the dissection of the upper pole difficult. To avoid this, we made a midline incision 1 cm distal to the frenulum of the lower lip and inserted the lateral trocars close to the mouth angle so as to locate the midline trocar on the different plane from the lateral trocars.
There is a concern for surgical site infection because this approach converts clean wound into clean-contaminated wound. Initially, we used intravenous antibiotics for 3 days after the operation and prescribed oral antibiotics for an additional 3 days. However, we had no case of deep site or wound infection until the 7th case, and changed the protocol not to use additional antibiotics after a single dose of prophylactic antibiotics. To our knowledge, there has been no case of infection since one patient was reported to have a local infection at the incision site in 2011 [6]. The rare occurrence of infection might be because the connection between the wound at the lower lip and the oral cavity can be minimized during the operation if the lower lip is kept lifted upward in a transvestibular approach.
The endotracheal tube in TOET can be nasotracheally intubated to obtain enough space for instrument manipulation [10], and EMG endotracheal tubes can also be nasotracheally intubated [18]. However, the nasal cavity of Asian patients are relatively narrow compared to Western patients, and likely to bleed during the intubation and extubation procedure. Therefore, we inserted EMG endotracheal tubes transorally and fixed them tightly at the midline. For the tube position, we fixed EMG endotracheal tubes at the mouth angle for the first case as shown in the literature [11], but the range of movement of the instrument on the tube side was limited. To avoid this, we changed the tube position to the midline, and the operation no longer suffered interference.
The operation time of TOET was relatively long, which can increase cost and anesthesia time for patients. However, transoral thyroidectomy is actively performed world-wide including the USA, Italy, and South Korea [192021], and the operation time will soon be reduced as experience accumulates with technical refinement. In summary, TOET was a feasible procedure and can be performed safely. Although the oncological safety should be evaluated in a large number of patients with longer follow-up, TOET may be an optional operative procedure for selective patients with PTMC.
ACKNOWLEDGEMENTS
This research was supported by a clinical research grant-inaid from the Seoul Metropolitan Government - Seoul National University Boramae Medical Center (03-2017-11). We would like to thank Han Mo Sung for data collection.
References
1. Kang SW, Lee SC, Lee SH, Lee KY, Jeong JJ, Lee YS, et al. Robotic thyroid surgery using a gasless, transaxillary approach and the da Vinci S system: the operative outcomes of 338 consecutive patients. Surgery. 2009; 146:1048–1055. PMID: 19879615.

2. Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, et al. Endoscopic thyroidectomy using a new bilateral axillobreast approach. World J Surg. 2007; 31:601–606. PMID: 17308853.

3. Inukai M, Usui Y. Clinical evaluation of gasless endoscopic thyroid surgery. Surg Today. 2005; 35:199–204. PMID: 15772789.

4. Terris DJ, Singer MC, Seybt MW. Robotic facelift thyroidectomy: II. Clinical feasibility and safety. Laryngoscope. 2011; 121:1636–1641. PMID: 21721012.

5. Witzel K, von Rahden BH, Kaminski C, Stein HJ. Transoral access for endoscopic thyroid resection. Surg Endosc. 2008; 22:1871–1875. PMID: 18163167.

6. Wilhelm T, Metzig A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World J Surg. 2011; 35:543–551. PMID: 21088839.

7. Karakas E, Steinfeldt T, Gockel A, Mangalo A, Sesterhenn A, Bartsch DK. Transoral parathyroid surgery-- a new alternative or nonsense? Langenbecks Arch Surg. 2014; 399:741–745. PMID: 24728604.
8. Nakajo A, Arima H, Hirata M, Mizoguchi T, Kijima Y, Mori S, et al. Trans-oral video-assisted neck surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc. 2013; 27:1105–1110. PMID: 23179070.

9. Wang C, Zhai H, Liu W, Li J, Yang J, Hu Y, et al. Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery. 2014; 155:33–38. PMID: 23890962.

10. Anuwong A. Transoral endoscopic thyroidectomy vestibular approach: a series of the first 60 human cases. World J Surg. 2016; 40:491–497. PMID: 26546193.

11. Wang Y, Yu X, Wang P, Miao C, Xie Q, Yan H, et al. Implementation of intraoperative neuromonitoring for transoral endoscopic thyroid surgery: a preliminary report. J Laparoendosc Adv Surg Tech A. 2016; 26:965–971. PMID: 27585396.

12. Ito Y, Miyauchi A, Kihara M, Higashiyama T, Kobayashi K, Miya A. Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid. 2014; 24:27–34. PMID: 24001104.

13. Ito Y, Miyauchi A, Inoue H, Fukushima M, Kihara M, Higashiyama T, et al. An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg. 2010; 34:28–35. PMID: 20020290.

14. Maser C, Donovan P, Udelsman R. Thyroid isthmusectomy: a rarely used but simple, safe, and efficacious operation. J Am Coll Surg. 2007; 204:512–514. PMID: 17324791.

15. Nixon IJ, Palmer FL, Whitcher MM, Shaha AR, Shah JP, Patel SG, et al. Thyroid isthmusectomy for well-differentiated thyroid cancer. Ann Surg Oncol. 2011; 18:767–770. PMID: 20882418.

16. Jitpratoom P, Ketwong K, Sasanakietkul T, Anuwong A. Transoral endoscopic thyroidectomy vestibular approach (TOETVA) for Graves' disease: a comparison of surgical results with open thyroidectomy. Gland Surg. 2016; 5:546–552. PMID: 28149798.

17. Sasanakietkul T, Jitpratoom P, Anuwong A. Transoral endoscopic parathyroidectomy vestibular approach: a novel scarless parathyroid surgery. Surg Endosc. 2016; 12. 28. DOI: 10.1007/s00464-016-5397-5. [Epub].

18. Inabnet WB 3rd, Suh H, Fernandez-Ranvier G. Transoral endoscopic thyroidectomy vestibular approach with intraoperative nerve monitoring. Surg Endosc. 2017; 31:3030. PMID: 27834022.

19. Udelsman R, Anuwong A, Oprea AD, Rhodes A, Prasad M, Sansone M, et al. Trans-oral vestibular endocrine surgery: a new technique in the United States. Ann Surg. 2016; 264:e13–e16. PMID: 27649533.
20. Dionigi G, Bacuzzi A, Lavazza M, Inversini D, Pappalardo V, Boni L, et al. Transoral endoscopic thyroidectomy via vestibular approach: operative steps and video. Gland Surg. 2016; 5:625–627. PMID: 28149809.

21. Park JO, Kim MR, Kim DH, Lee DK. Transoral endoscopic thyroidectomy via the trivestibular route. Ann Surg Treat Res. 2016; 91:269–272. PMID: 27847801.

Fig. 1
Patient position and incisions of transoral endoscopic thyroidectomy. (A) Patients were placed in supine position with slight neck extension and (B) incisions were made at midline (2-cm length) and 1 cm medial to mouth angle (5-mm length).
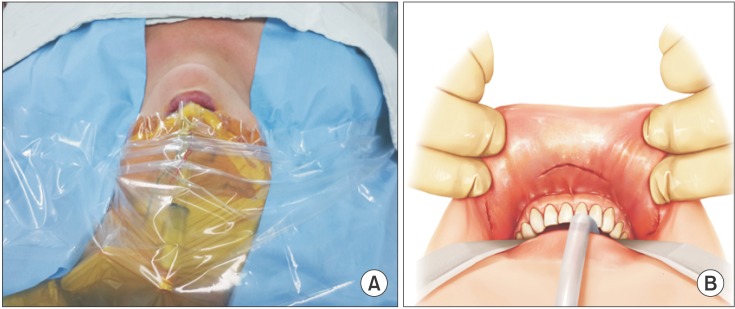
Fig. 2
Procedures of transoral endoscopic thyroidectomy. (A) Isthmus was divided at the midline. (B) Strap muscles were retracted using external hanging suture. (C) Identification of the right recurrent laryngeal nerve (white arrowheads). Common carotid artery is demonstrated (black arrow).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download