Abstract
Purpose
Partially absorbable mesh has been introduced and used for inguinal hernia repair for the purpose of minimizing pain and improving abdominal wall compliance. In this study, we evaluate the efficacy and safety of ProFlex mesh, a partially absorbed mesh with new structural architecture.
Methods
We retrospectively reviewed 64 cases of totally extraperitoneal herniorrhapy (TEP) from January 2013 to December 2014 for their clinical features, including operation time, pain, postoperative complications, and recurrence.
Results
There were no significant differences in operation time, hospital stay, postoperative pain, or complications between the 28 patients who received the ProFlex mesh and the 36 who received nonabsorbable lightweight mesh, although one patient who received the nonabsorbable had a recurrence during follow-up. There were differences in operation time, complications, and hospital stay according to the surgeon's previous operation volume.
Approximately 35,000 inguinal or groin hernia repair operations are performed annually in Korea, as reported by the Organisation for Economic and Co-operative Development. With the introduction of mesh material for patients with inguinal hernias in the 1930s, low recurrence rates of 2%–4% were observed, and now the use of mesh has become standard practice [123]. Although mesh placement prevents recurrences, the mesh itself might be a source of mechanical impairment of the patients' movement or generate a phenomenon called foreign body feeling; when totally extraperitoneal herniorrhaphy (TEP), was introduced in the 1990s, the rates of nerve injury and wound scarring after operation decreased significantly.
Subsequent inflammatory reactions after placement may cause chronic pain [1,4,5,6]; in one study, the incidence of such complications after inguinal hernia varied [6]. A number of recent studies showed that such differences in incidence were affected by type of mesh material (lightweight vs. heavyweight) and that the use of lightweight mesh showed significantly fewer postoperative complications during both open [78910111213] and laparoscopic surgery [141516171819]. Theoretically, ultralight mesh could be considered the ideal mesh material, but it has problems such as difficult intraoperative control and potential risk of early recurrence.
UltraPro (Ethicon, Somerville, NJ, USA), a partially absorbable mesh that overcomes the disadvantages of both heavyweight and ultralight mesh, consists of an entanglement of absorbable and nonabsorbable fibers; it offers feasibility during surgery, strength in the early postoperative period, and fewer foreign body materials left behind. ProFlex (Samyang Bio farm, Seoul, Korea), another partially absorbable mesh with a novel different architecture, is composed of single filaments designed to contain both absorbable and nonabsorbable portions all together in each filaments. Although ProFlex has been used for many years, no studies have reported on its use.
In this study, we retrospectively reviewed our cases of hernia repair with ProFlex mesh and Optilene (B. Braun, Melsungen, Germany), typically used nonabsorbable lightweight mesh, to compare their efficacy and safety in TEP.
We performed a retrospective study at a single tertiary referral hospital in Korea of all inguinal hernia patients who underwent endoscopic TEP repair of inguinal hernia. Our center began using partially absorbable mesh in January 2013. Of approximately 90 hernia repairs annually, 20 used partially absorbable mesh; we planned to include 30 cases of hernia using partially absorbable mesh. This study was approved by the Institutional Review Board of Korea University Guro Hospital (KUGH15047-001), Korea. We reviewed all cases of TEP from January 2013 to December 2014 for clinical data. We included patients over 19 years old who had unilateral inguinal hernias and who had 1 year of followup. The patients recruited from January 2013 to December 2013 were grouped as early period group and the patients recruited from January 2014 to December 2014 were grouped as late period group to determine whether there was bias according to time flow. We divided the patients by type of mesh, partially absorbable and nonabsorbable mesh group. There was no specific predetermined indication of what mesh to use and was used according to the surgeon's preference. Due to similarity of the texture of Optilene and Proflex, the surgeon had no subjective difference in manipulation of mesh during surgery. We reviewed medical data such as clinical information (sex, age, duration of symptoms, body mass index) and operation time to compare the comfort of the surgical techniques and the incidence of postoperative complications. To evaluate postoperative complications, we checked the occurrence of seroma by physical examination and voiding difficulty as an immediate complication on the day of surgery. The patients were discharged on day 1 after the operation as standard when there were no early complications, but with complaints of discomfort or fear after discharge, the patients were discharged on day 2. At the outpatient clinic, patients were checked on postoperative day 7 for occurrence of seroma, infection, and foreign body sensation. The patients were instructed to revisit the outpatient clinic for any feelings of discomfort or pain during one year of follow-up. Patients were subsequently followed up by phone at three months, 6 months, and 1 year to check for late complications such as foreign body sensation and recurrence. Since both of the meshes to be compared in this study were not heavyweight meshes, the presence of recurrence rather than foreign body sensation was the main question as long term complication. At 3 months, patients were asked about pain continued for more than 2 weeks after surgery. At 6 months and 1 year, patients were asked about presence of the symptom of recurrence.
Two highly experienced surgeons in the general colorectal surgery department performed all of the operations; Surgeon A had performed more than 200 hernia repairs, and surgeon B had performed 50 before the study period. In brief, the operation methods were as follows: All patients were subjected to general anesthesia in the supine position. Preperitoneal access was achieved through one infraumbilical transverse 12-mm incision. After dissection between the rectus muscle and the posterior rectus sheath using the posterior tip of a long forceps, we inserted space makers into the preperitoneal space to advance to the pubic symphysis and then inflated the balloon, thereby creating an optical cavity. We inserted the 12-mm trochar and maintained the optical cavity by carbon dioxide insufflation; we inserted an additional two 5-mm trochars as work ports. In cases of indirect hernia, we disunited the hernia sac from the cord and applied the mesh after complete reduction without sac ligation. We laid over the mesh to cover the whole hernia site completely without additional fixation and carbon dioxide was out.
We performed the statistical analyses using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA), and we used chisquare and Student t-test to calculate significance, which we considered a P-value < 0.05. The descriptive data are expressed as mean ± standard deviation.
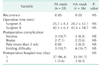
During our period of interest, a total of 64 patients received TEP for unilateral inguinla hernias and were included in the study; 28 had received partially absorbable mesh, and 36 had received nonabsorbable mesh. Sixty patients were men and 4 were women, and there was no difference in sex ratio. The group that received partially absorbable mesh was younger than the patients who received the nonabsorbable mesh (56.7 ± 14.8 vs. 61.6 ± 13.3), but there were no statistically significant differences between the 2 groups. In fact, by mesh type, there were no statistically significant differences in age, sex, herniation side, herniation type, operator, or period of herniation (Table 1). There were no conversions to either open or transabdominal preperitoneal (TAPP) repair.
Table 2 shows the operation results and postoperative complications by mesh type. Surgeon A's mean operation time with the partially absorbable mesh was 25.7 ± 8.2 minutes and 28.2 ± 12.1 minutes with the nonabsorbable mesh. Surgeon B's mean operation time was 42.3 ± 6.3 minutes with the partially absorbable mesh and 45.6 ± 18.7 minutes for the nonabsorbable patients; there were no intrasurgeon differences in operation time by mesh type. At 1-year followup, there was no recurrence in either group. In the partially absorbable mesh group, seven patients had postoperative complications (25%), seroma in 3 cases (10.7%), bruising in 2 (7.1%), and voiding difficulty in 3 (10.7%); no patients suffered from pain in the partially absorbable mesh group. A total of 14 patients had postoperative complications (35%) in the nonabsorbable mesh group, 3 cases (8.3%) of seroma, 2 (5.6%) of bruising, 3 (8.3%) of postoperative pain, and 6 cases (16.7%) of voiding difficulty; the incidences of each complication were not statistically significantly different between the 2 groups, and the outcome measure differences in postoperative hospital stay were also not statistically significant. None of the complications was life-threatening, and all were relieved with conservative treatment.
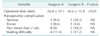
We compared the 2 surgeons' operation times and incidence of postoperative complications to improve reliability. The mean operation times for surgeons A and B were 26.8 ± 10.1 and 44.6 ± 15.8, respectively, which was statistically significant, but incidence of postoperative complications was not (Table 3).
Once mesh material was developed, recurrence rates and postoperation complications from hernia surgery decreased significantly. Nonabsorbable mesh types such as polypropylene, polytetrafluorethylene, and polyester were initially used for hernia repair. Among these, heavy polypropylene mesh was most commonly used because it had many benefits such as being flexible, strong, easily cut, readily integrated by surrounding tissues, and resistant to infection. However, postoperative pain and foreign body feeling continuously bothered patients, and thus lightweight and ultralightweight meshes were developed. However, although the use of the lightweight mesh resulted in much less postoperative pain and foreign body feeling than the use of the heavyweight nonabsorbable mesh, decreased intraoperative control and increased recurrence rates were more common. To maximize both intraoperative control and postoperative comfort and also minimizing recurrence rates, partially absorbable prostheses were recently developed that combined nonabsorbable materials such as polypropylene as standard with absorbable materials such as polyglactin that had the benefit of leaving behind less foreign material in the recipient without compromising mechanical resistance.
Optilene (polypropylene) and ProFlex (glycolide–co-caprolactone + polypropylene) meshes were used in this study. Optilene mesh is made using nonabsorbable fibers, whereas the ProFlex fibers are a combination of absorbable and nonabsorbable fibers (Table 4). ULTRAPRO, a typical partially absorbable mesh that compensates for the disadvantages of both heavyweight and ultralight mesh, is an entanglement of absorbable and nonabsorbable fibers that offers feasibility during surgery and strength in the early postoperative period; its use also results in less foreign body material remaining in the patient. ProFlex, is also a partially absorbable mesh but with a novel different architecture: it is composed of single filaments designed to contain both absorbable and nonabsorbable portions. The noteworthy aspect of this composition is that the pore size remains unchanged even when a single filament changes to multifilament fibers and its total weight decreases gradually with time (Fig. 1).
Despite numerous studies, there are still conflicts regarding the optimal mesh type for endoscopic hernia repair considering postoperative complications and patients' feelings. A limited number of randomized studies have been published recently that assessed the outcomes after implantation of lightweight and heavyweight mesh in endoscopic TEP hernia repair [192021]. Two studies showed slight benefits with lightweight meshes during the early postoperative period compared with heavyweight mesh in terms of chronic pain and impairment of physical activities [1920].
However, one systematic review of eight trials and 1,667 cases that compared the outcomes of inguinal hernia repair using new lightweight mesh and transitional heavyweight mesh showed that both mesh repairs had similar outcomes with regard to postoperative pain, seroma development, and time to return to work [22].
Seromas are known to be the most common postoperative complication after TEP inguinal hernia repair, and they also occurred most often in this study. In one previous study, the median rate of posthernia repair seromas was 8.79%. Similarly, in the present study, the rate of postoperation seroma was 10.7% with the partially absorbable mesh and 8.3% in the nonabsorbable mesh group [23].
One recent large, double-blind, randomized control trial analyzed 950 patients with unilateral primary inguinal hernias who underwent endoscopic TEP using either ULTRAPRO (partially absorbable) or Prolene (Ethicon, Somerville, NJ, USA) mesh and found no significant differences in incidence or intensity of pain, foreign body feeling, or any other end point 3 months after TEP repair. In addition, no differences were found at other time points throughout 3 months of early postoperative follow-up [2124].
There could be surgeon biases that can affect surgical time and mesh handling techniques. In our study, one surgeon took a mean 26.8 minutes for the TEP operation, whereas the other took a mean 44.6 minutes. Although this was a significant difference in median operation time between the 2 surgeons, the type of mesh used did not affect either surgeon's operation time (25.7 minutes vs. 28.2 minutes, 42.3 minutes vs. 45.6 minutes). There might be individual differences in TEP skill and ability, but type of mesh does not matter for operation quality. These results suggest the feasibility of using ProFlex for inguinal hernia repair.
In a previous study, the median recurrence rate after hernia was 2.1% (8 of 388); by subgroups, the rate was 1.0% with absorbable mesh and 5.3% with the nonabsorbable mesh (P < 0.05), and the average time from surgery to recurrence was 432.4 days [25]. In the present study, no recurrence was found in either groups, but our median follow-up period was 1 year, so additional observations are needed based on the previously known recurrence period.
The mesh was not fixed in all cases in this study. The long-standing standard practice for TAPP hernia repair was to use mesh fixation with tackers to prevent recurrence [26], but atraumatic mesh fixation fibrin sealants are being increasingly employed to prevent chronic pain following traumatic fixation procedures [27]. Additionally, numerous studies have showed that both fixation and nonfixation of the mesh were associated with equally low recurrence rates in both TAPP and TEP [28]. As more evidence of these results, the data presented here also reveal no recurrences without fixation in any cases regardless of type of mesh.
As noted above, we found no differences in recurrence rates or postoperative complications such as seromas, bruising, pain, or voiding difficulty between the partially absorbable Proflex mesh and the nonabsorbable mesh, and these findings suggest that Proflex is not inferior to classic nonabsorbable mesh. There are some limitations to our study. It was a retrospective study based on the data of a relatively small number of patients in a single institution, and we evaluated postoperative pain solely on a yes-or-no basis rather than using detailed pain scores. However, our study is the first to compare the recurrence rates and chronic pain outcomes of ProFlex and Optilene.
In the present study, ProFlex, a partially absorbable mesh with new architecture, showed feasible and safe results in TEP. However, more large prospective studies are needed to give more reliability to these results.
Figures and Tables
 | Fig. 1Composition of and changes in ProFlex (Samyang Bio farm, Seoul, Korea) partially absorbable mesh. PP, polypropylene, PGA-PCL, poly (glycolide-co-caprolactone). |
References
1. Bay-Nielsen M, Kehlet H, Strand L, Malmstrom J, Andersen FH, Wara P, et al. Quality assessment of 26,304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet. 2001; 358:1124–1128.
2. EU Hernia Trialists Collaboration. Repair of groin hernia with synthetic mesh: meta-analysis of randomized controlled trials. Ann Surg. 2002; 235:322–332.
3. van Veen RN, Wijsmuller AR, Vrijland WW, Hop WC, Lange JF, Jeekel J. Long-term follow-up of a randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg. 2007; 94:506–510.
4. Klinge U, Klosterhalfen B, Müller M, Schumpelick V. Foreign body reaction to meshes used for the repair of abdominal wall hernias. Eur J Surg. 1999; 165:665–673.
5. Cunningham J, Temple WJ, Mitchell P, Nixon JA, Preshaw RM, Hagen NA. Cooperative hernia study. Pain in the postrepair patient. Ann Surg. 1996; 224:598–602.
6. Poobalan AS, Bruce J, King PM, Chambers WA, Krukowski ZH, Smith WC. Chronic pain and quality of life following open inguinal hernia repair. Br J Surg. 2001; 88:1122–1126.
7. Post S, Weiss B, Willer M, Neufang T, Lorenz D. Randomized clinical trial of lightweight composite mesh for Lichtenstein inguinal hernia repair. Br J Surg. 2004; 91:44–48.
8. O'Dwyer PJ, Kingsnorth AN, Molloy RG, Small PK, Lammers B, Horeyseck G. Randomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repair. Br J Surg. 2005; 92:166–170.
9. Bringman S, Wollert S, Osterberg J, Smedberg S, Granlund H, Heikkinen TJ. Three-year results of a randomized clinical trial of lightweight or standard polypropylene mesh in Lichtenstein repair of primary inguinal hernia. Br J Surg. 2006; 93:1056–1059.
10. Paajanen H. A single-surgeon randomized trial comparing three composite meshes on chronic pain after Lichtenstein hernia repair in local anesthesia. Hernia. 2007; 11:335–339.
11. Koch A, Bringman S, Myrelid P, Smeds S, Kald A. Randomized clinical trial of groin hernia repair with titanium-coated lightweight mesh compared with standard polypropylene mesh. Br J Surg. 2008; 95:1226–1231.
12. Polish Hernia Study Group. smietanski M. Randomized clinical trial comparing a polypropylene with a poliglecaprone and polypropylene composite mesh for inguinal hernioplasty. Br J Surg. 2008; 95:1462–1468.
13. Nikkolo C, Lepner U, Murruste M, Vaasna T, Seepter H, Tikk T. Randomised clinical trial comparing lightweight mesh with heavyweight mesh for inguinal hernioplasty. Hernia. 2010; 14:253–258.
14. Bringman S, Wol lert S, Osterberg J, Heikkinen T. Early results of a randomized multicenter trial comparing Prolene and VyproII mesh in bilateral endoscopic extraperitoneal hernioplasty (TEP). Surg Endosc. 2005; 19:536–540.
15. Heikkinen T, Wollert S, Osterberg J, Smedberg S, Bringman S. Early results of a randomised tr ial compar ing Prolene and VyproII-mesh in endoscopic extraperitoneal inguinal hernia repair (TEP) of recurrent unilateral hernias. Hernia. 2006; 10:34–40.
16. Langenbach MR, Schmidt J, Zirngibl H. Comparison of biomaterials: three meshes and TAPP for inguinal hernia. Surg Endosc. 2006; 20:1511–1517.
17. Agarwal BB, Agarwal KA, Mahajan KC. Prospective doubleblind randomized controlled study comparing heavy- and lightweight polypropylene mesh in totally extraperitoneal repair of inguinal hernia: early results. Surg Endosc. 2009; 23:242–247.
18. Chui LB, Ng WT, Sze YS, Yuen KS, Wong YT, Kong CK. Prospective, randomized, controlled trial comparing lightweight versus heavyweight mesh in chronic pain incidence after TEP repair of bilateral inguinal hernia. Surg Endosc. 2010; 24:2735–2738.
19. Chowbey PK, Garg N, Sharma A, Khullar R, Soni V, Baijal M, et al. Prospective randomized clinical trial comparing lightweight mesh and heavyweight polypropylene mesh in endoscopic totally extraperitoneal groin hernia repair. Surg Endosc. 2010; 24:3073–3079.
20. Bittner R, Schmedt CG, Leibl BJ, Schwarz J. Early postoperative and one year results of a randomized controlled trial comparing the impact of extralight titanized polypropylene mesh and traditional heavyweight polypropylene mesh on pain and seroma production in laparoscopic hernia repair (TAPP). World J Surg. 2011; 35:1791–1797.
21. Cristaudo A, Nayak A, Martin S, Adib R, Martin I. A prospective randomised trial comparing mesh types and fixation in totally extraperitoneal inguinal hernia repairs. Int J Surg. 2015; 17:79–82.
22. Currie A, Andrew H, Tonsi A, Hurley PR, Taribagil S. Lightweight versus heavyweight mesh in laparoscopic inguinal hernia repair: a metaanalysis. Surg Endosc. 2012; 26:2126–2133.
23. Gao D, Wei S, Zhai C, Chen J, Li M, Gu C, et al. Clinical research of preperitoneal drainage af ter endoscopic total ly extraperitoneal inguinal hernia repair. Hernia. 2015; 19:789–794.
24. Burgmans JP, Voorbrood CE, Schouten N, Smakman N, Elias S, Clevers GJ, et al. Threemonth results of the effect of Ultrapro or Prolene mesh on post-operative pain and well-being following endoscopic totally extraperitoneal hernia repair (TULP trial). Surg Endosc. 2015; 29:3171–3178.
25. Ujiki MB, Gitelis ME, Carbray J, Lapin B, Linn J, Haggerty S, et al. Patient-centered outcomes following laparoscopic inguinal hernia repair. Surg Endosc. 2015; 29:2512–2519.
26. Bittner R, Leibl BJ, Jäger C, Kraft B, Ulrich M, Schwarz J. TAPP Stuttgart technique and result of a large single center series. J Minim Access Surg. 2006; 2:155–159.
27. Bittner R, Gmähle E, Gmähle B, Schwarz J, Aasvang E, Kehlet H. Lightweight mesh and noninvasive fixation: an effective concept for prevention of chronic pain with laparoscopic hernia repair (TAPP). Surg Endosc. 2010; 24:2958–2964.
28. Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc. 2011; 25:2773–2843.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download