Abstract
Purpose
There is no consensus regarding the difference in outcomes of HCV in patients who receive living donor liver transplantation (LDLT) or compared to deceased donor liver transplantation (DDLT). The aims of this study were to compare characteristics between LDLT and DDLT groups and to identify risk factors affecting patient survival.
Methods
We retrospectively reviewed the multicenter records of 192 HCV RNA-positive patients who underwent liver transplantation.
Results
Thirty-five patients underwent DDLT, and 146 underwent LDLT. The 1-, 3-, and 5-year patient survival rates were 66.7%, 63.0%, and 63.0% in the DDLT group and 86.1%, 82.3%, and 79.5% in the LDLT group (P = 0.024), respectively. After propensity matching, the patient survival curve of the LDLT group was higher than that of the DDLT group. However, there was no statistically significant difference in patient survival between the 2 groups (P = 0.061). Recipient age ≥ 60 years, LDLT, and use of tacrolimus were positively associated with patient survival in multivariate analyses.
HCV infection is the most common underlying disease among Western patients requiring liver transplantation (LT). In Korea, 1%–2% of the population is infected with HCV, and 15%–20% of these infected individuals have chronic liver disease related to HCV infection [1]. As HCV prevalence has increased, HCV-related cirrhosis and HCV-related hepatocellular carcinoma (HCC) will gradually become more common indications for LT in Korea [2].
Recurrent HCV infection after LT is associated with reduced graft and patient survival [3]. Several studies have demonstrated worse survival outcomes in HCV-positive LT patients compared to HCV-negative patients [4]. Recipient, donor, and transplant-related factors are associated with a high risk of severe and progressive HCV disease. Poor donor liver quality, older donor age, prolonged warm and cold ischemia times, donation after cardiac death, and a high donor risk index are associated with lower graft survival and higher rates of advanced fibrosis [5].
Living donor LT (LDLT) is an important advancement that has expanded the donor pool and decreased wait-list mortality rates [67]. Early data have suggested that HCV patients who underwent LDLT had worse outcomes, including increased rates of cholestatic HCV, compared to DDLT recipients [8]. However, recent studies suggest there are no significant differences in outcomes between patients who receive LDLT versus DDLT for HCV-related disease, including graft and patient survival [91011]. The lack of consensus within the field emphasizes the importance of a better understanding of the optimal mode of LT for HCV-positive patients.
Herein, we compared patient characteristics and survival data of HCV-positive patients who underwent either LDLT or DDLT and identified factors associated with patient survival.
This study was conducted in 3 liver transplantation centers in Korea: Samsung Medical Center (SMC), Asan Medical Center (AMC), and Seoul National University Hospital (SUNH). Because this was a retrospective study, we were not able to request patient consent for the use of clinical records. However, each center's Institutional Review Board (IRB) approved our protocols (Samsung Medical Center IRB No. 2014-07-031, Asan Medical Center IRB No. S2015-1341-0003, Seoul National University Hospital IRB No. 1407-139-597). Present study was exempt from written informed consent at each IRB. We retrospectively evaluated the medical records of patients who underwent their first LT between 1999 and 2012. Data from all consecutive 192 HCV RNA-positive cases during this period were reviewed using the same questionnaire. However, immunosuppression protocols, treatment for organ rejection, and treatment for recurrent HCV infection were not standardized across centers. The laboratory-based model of end-stage liver disease (MELD) score was calculated at the time of transplantation. Information on and/or records of all patients were deidentified prior to analysis. Cases of hospital mortality (n = 11) were excluded from our analysis of risk factor identification. We ultimately investigated risk factors associated with patient survival in 181 patients.
The following variables were obtained from our medical record review in response to the survey: patient age, sex, HCV genotype, MELD score, co-occurrence with HCC, coinfection with HBV or HIV, antiviral treatments received after transplantation, type of calcineurin inhibitor received, use of mycophenolate mofetil (MMF), steroid withdrawal, biopsy-proven acute rejection, HCV recurrence, and other outcomes. Additionally, donor age and ischemic time were included as variables. Finally, we recorded information on patient survival and calculated the time to death. However, we did not incorporate any other incomplete variables that might have been associated with patient survival, such as IL-28 gene polymorphisms, histological findings, biliary complications, or infectious episodes. Diagnosis of acute rejection was based on internationally accepted histologic criteria (Banff guidelines) using liver biopsies [12]. HCV recurrence was diagnosed based on histology, biochemistry, and/or detection of HCV RNA in the serum.
To avoid confounding differences between DDLT and LDLT due to baseline differences between DDLT and LDLT recipients, we performed our analyses with all patients and after propensity score matching. Patients in the DDLT and LDLT groups were matched using propensity scores in IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). The propensity score of an individual was calculated given the covariates of recipient age, donor age, MELD score, and use of calcineurin inhibitors using a logistic regression model. We applied 1:1 nearest neighbor matching without replacement in order to ensure that conditional bias was minimized. Each patient in the DDLT group was matched to a patient in the LDLT group with the mini mum difference in propensity score.
Continuous data are reported as the median and range and were compared using the Mann-Whitney U-test. Categorical variables are reported as numeric proportions. Comparisons of categorical data between groups were performed using the chi-square test or Fisher exact test as appropriate. Patient survival rates were evaluated using the Kaplan-Meier method and compared using the log-rank test. Clinical variables found to have prognostic significance by univariate analysis were entered into a Cox multivariate proportional hazards model to determine which factors independently predicted patient survival. The cutoff values for continuous variables were set according to each receiver operating characteristic (ROC) curve. Statistical significance was set at a P-value less than 0.05. Statistical analyses were performed using IBM SPSS Statistics ver. 21.0.
Patient characteristics are shown in Table 1. There were 35 DDLT patients and 146 LDLT patients. Median ages of the DDLT and LDLT recipients were 53 years (range, 34–69) and 57 years (range, 34–72), respectively (P = 0.418); however, the median donor age of the DDLT group was significantly older than that of the LDLT group (41 years vs. 31 years, P < 0.001). Thus, the proportion of donors in the DDLT group who were older than 30 was 80%, compared to 53.4% in the LDLT group. No significant differences in gender, HCV genotype, HCV RNA, HBV coinfection, or HCC co-occurrence were observed between the 2 groups. The median MELD score of the DDLT group was significantly higher than that of the LDLT group (21 vs. 15, P < 0.001).
Most of the DDLT patients received a whole liver graft (97.1%), while LDLT patients largely received right lobe grafts (91.8%) (P < 0.001). The median graft-to-recipient weight ratio in the LDLT group was 1.08 (range, 0.68–1.20). Warm ischemic time in the DDLT group was not significantly different from that in the LDLT group (44 minutes vs. 38 minutes, P = 0.124), but cold ischemic time was significantly longer in the DDLT group than in the LDLT group (228 minutes vs. 77 minutes, P < 0.001).
The median follow-up durations in the DDLT and LDLT groups were 19 months (range, 2–157 months) and 38 months (range, 2–151 months), respectively. There were no statistically significant differences in the use of induction agent, used cyclosporine, used tacrolimus, used MMF, or steroid use for longer than six months, HCV recurrence or biopsy-proven acute rejection between the 2 groups. Most patients in the LDLT group received universal prophylaxis, while most DDLT patients received preemptive treatment.
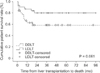
The 1-, 3-, and 5-year patient survival rates were 66.7%, 63.0%, and 63.0%, respectively, in the DDLT group and 86.1%, 82.3%, and 79.5% in the LDLT group (P = 0.024) (Fig. 1). The causes of mortality are summarized in Table 2. Twelve patients in the DDLT group and 28 patients in the LDLT group died during the observation period. The most common cause of death in both groups was sepsis. Univariate analyses revealed that recipient age ≥60 years, LDLT, use of tacrolimus, and biopsy-proven acute rejection were closely associated with increased patient survival. Recipient age ≥60 years, LDLT, and use of tacrolimus were determined to be independent factors associated with patient survival in multivariate analyses (Table 3).
Propensity score matching analysis created 31 pairs of patients. Baseline, perioperative, and post-transplant char acteristics except cold ischemic time and graft type were similar between the two matched groups (Table 4). The cold ischemic time in the DDLT group was longer than that in the LDLT group (P < 0.001). After propensity matching, the patient survival curve of the LDLT group was higher than that of the DDLT group. The 1-year patient survival rates of the DDLT and LDLT groups were 62.7% and 87.1%, respectively (P = 0.024). However, there was no statistically significant difference in patient survival curve between the 2 groups (P = 0.061) (Fig. 2).
In this multicenter study, we found that HCV RNA-positive patients who underwent LDLT had significantly higher survival rates than patients who underwent DDLT. However, DDLT recipients had worse prognostic factors, such as older donor age, higher MELD score, and longer cold ischemic time, compared with LDLT recipients.
A previous study reported a worse graft outcome and more aggressive recurrent hepatitis C after LDLT compared with DDLT because of genetic similarity between the donor and recipient and enhanced HCV replication by intense hepatocyte proliferation in partial liver grafts [8]. The worse outcomes reported after LDLT might have been due to an increased rate of biliary complications or other problems experienced during the learning-curve years of LDLT [1314]. Among the 3 centers that participated in this study, more than 100 LDLTs are performed annually.
More recent studies have reported improved results in LDLT recipients compared with DDLT because of the young age of the living donor and shorter ischemic time of LDLT [15]. Generally, DDLT recipients have a higher MELD score than LDLT recipients. High MELD score is considered an independent prognostic factor for severe recurrent HCV and worse patient or graft outcome; therefore, the above data should be evaluated with caution [16]. Similar outcomes were observed for LDLT and DDLT in a recent study using adjusted MELD scores and donor age [15].
Patient enrolled in the present study had similar baseline characteristics compared with those in previous studies. Donor age was younger and cold ischemic time was shorter in the LDLT group than in the DDLT group. However, donor age was not significantly associated with recipient survival in our study, most likely because the median donor age in the present study was young (32 years old) due to the higher proportion of LDLT cases. However, the Adult-to-Adult Living Donor Liver Transplantation Cohort Study (A2ALL) found no statistical difference in the 5-year cumulative risk of advanced fibrosis between LDLT and DDLT patients (44% in LDLT patients vs. 37% in DDLT patients, P = 0.16) [13]. In addition, they reported that the 5-year unadjusted patient and graft survival probability were 79% and 78% in LDLT and 77% and 75% in DDLT, respectively [13]. The present study showed that the 5-year unadjusted patient survival rate was 63% in DDLT and 79.5% in LDLT. In the A2ALL study, the median MELD score in the DDLT group was 19 points (range, 14–25), whereas that in the present study was 20 points (range, 8–38). Median MELD score was similar between present study and A2ALL study, but the range of MELD scores in the present study was wider than in the A2ALL study.
LDLT offers a survival advantage for wait-listed patients compared to DDLT [17]. With an increasing number of patients in need of organs, LDLT is an important means of expanding the donor pool. LDLT has several advantages over DDLT, including a shorter waiting time, lower dropout rate, reduced cold ischemia time, and a more thorough pretransplant evaluation for both the donors and recipients. However, most single-center studies have suggested that HCV disease severity among LDLT recipients is either similar or worse than that among DDLT patients [9]. We compared LDLT and DDLT patients using propensity score matching because of differences in baseline characteristics such as recipient age, donor age, MELD score, and calcineurin inhibitors. Cold ischemic time was not matched, however, due to the large difference between the DDLT and LDLT groups. After matching, the patient survival curve of the LDLT group was better than that of the DDLT group. However, the survival difference between the 2 groups was not statistically significant; only the 1-year patient survival rate in the LDLT group was higher than that in the DDLT group (87.1% vs. 62.7%; P = 0.024). Long ischemic time is related to ischemic-reperfusion injury, which contributes to increased morbidity and mortality after LT [18]. The present study showed that long cold ischemic time in DDLT recipients resulted in worse patient survival than LDLT recipients despite matching of important variables.
In our study, HCV-infected patients were treated with a combination of interferon and ribavirin. Since the introduction of direct-acting antivirals (DAA) in 2011, sustained viral response 12 weeks after treatment can be achieved in 70% of recurrent HCV liver recipients [19]. Sofosbuvir-based therapy is recommended in the pre- and posttransplant periods [20]. In this era of DAA, there are not likely to be differences in the outcomes of DDLT and LDLT HCV-infected recipients.
There are several limitations inherent to the study design, including variability in documentation, differences in selection criteria and data collection, and missing data. The present study was also seriously weakened by the imbalance in the number of subjects between the 2 groups. To minimize variability, we sent a standardized collection form containing 56 questions to each participating transplant center. Answers were either multiple-choice or involved providing a name or a specific value. However, the quality of the pretransplant interviews from which the baseline data were derived and the quality of the posttransplant follow-up data across the three centers were variable. In addition, the present study did not have a uniform policy for antiviral therapy in HCV recurrence after LT because of its multicenter nature. Furthermore, subjects had varying follow-up durations. We also did not have data on the onset of biopsy-proven acute rejection or the date of graft failure. Additionally, a lack of data regarding the interleukin-28B genotype of donors and recipients and the presence of fibrosis on biopsy are important limitations of this study. We used propensity score matching to minimize the influence of differences in baseline characteristics; however, given the small number of cases evaluated in the present study, the results should be interpreted with caution. To address these limitations, a well-designed prospective study is needed.
In conclusion, we showed that the survival of patients who underwent LDLT was higher than that of patients who underwent DDLT when the DDLT recipients had poor prognostic factors. Survival rates of LDLT recipients were similar to those of DDLT recipients after propensity score matching. Thus, LDLT appears to be suitable for HCV-infected patients if an appropriate living donor is available in this era of DAA.
Figures and Tables
Fig. 1
Survival curves of all LDLT and DDLT patients. LDLT, living donor liver transplantation; DDLT, deceased donor liver transplantation.

Fig. 2
Survival curves of propensity-matched LDLT and DDLT patients. LDLT, living donor liver transplantation; DDLT, deceased donor liver transplantation.
References
1. Shon HS, Choi HY, Kim JR, Ryu SY, Lee YJ, Lee MJ, et al. Comparison and analysis of the prevalence of hepatitis C virus infection by region in the Republic of Korea during 2005-2012. Clin Mol Hepatol. 2015; 21:249–256.
2. Kim JM, Lee KW, Song GW, Jung BH, Lee HW, Yi NJ, et al. Outcomes for patients with HCV after liver transplantation in Korea: a multicenter study. Ann Surg Treat Res. 2016; 90:36–42.
3. Howell J, Angus P, Gow P. Hepatitis C recurrence: the Achilles heel of liver transplantation. Transpl Infect Dis. 2014; 16:1–16.
4. Lake JR, Shorr JS, Steffen BJ, Chu AH, Gordon RD, Wiesner RH. Differential effects of donor age in liver transplant recipients infected with hepatitis B, hepatitis C and without viral hepatitis. Am J Transplant. 2005; 5:549–557.
5. Berenguer M, Schuppan D. Progression of liver fibrosis in post-transplant hepatitis C: mechanisms, assessment and treatment. J Hepatol. 2013; 58:1028–1041.
6. Lee SG. A complete treatment of adult living donor liver transplantation: a review of surgical technique and current challenges to expand indication of patients. Am J Transplant. 2015; 15:17–38.
7. Olthoff KM, Smith AR, Abecassis M, Baker T, Emond JC, Berg CL, et al. Defining long-term outcomes with living donor liver transplantation in North America. Ann Surg. 2015; 262:465–475.
8. Garcia-Retortillo M, Forns X, Llovet JM, Navasa M, Feliu A, Massaguer A, et al. Hepatitis C recurrence is more severe after living donor compared to cadaveric liver transplantation. Hepatology. 2004; 40:699–707.
9. Hu A, Liang W, Zheng Z, Guo Z, He X. Living donor vs. deceased donor liver transplantation for patients with hepatitis C virus-related diseases. J Hepatol. 2012; 57:1228–1243.
10. Mitchell O, Gurakar A. Management of hepatitis C post-liver transplantation: a comprehensive review. J Clin Transl Hepatol. 2015; 3:140–148.
11. Terrault NA, Shiffman ML, Lok AS, Saab S, Tong L, Brown RS Jr, et al. Outcomes in hepatitis C virus-infected recipients of living donor vs. deceased donor liver transplantation. Liver Transpl. 2007; 13:122–129.
12. Banff Working Group on Liver Allograft Pathology. Importance of liver biopsy findings in immunosuppression management: biopsy monitoring and working criteria for patients with operational tolerance. Liver Transpl. 2012; 18:1154–1170.
13. Terrault NA, Stravitz RT, Lok AS, Everson GT, Brown RS Jr, Kulik LM, et al. Hepatitis C disease severity in living versus deceased donor liver transplant recipients: an extended observation study. Hepatology. 2014; 59:1311–1319.
14. Brown RS Jr. Living donor liver transplantation for HCV: will the true outcomes stand up? J Hepatol. 2012; 57:1166–1167.
15. Jain A, Singhal A, Kashyap R, Safadjou S, Ryan CK, Orloff MS. Comparative analysis of hepatitis C recurrence and fibrosis progression between deceased-donor and living-donor liver transplantation: 8-year longitudinal follow-up. Transplantation. 2011; 92:453–460.
16. Akamatsu N, Sugawara Y. Liver transplantation and hepatitis C. Int J Hepatol. 2012; 2012:686135.
17. Berg CL, Merion RM, Shearon TH, Olthoff KM, Brown RS Jr, Baker TB, et al. Liver transplant recipient survival benefit with living donation in the model for endstage liver disease allocation era. Hepatology. 2011; 54:1313–1321.
18. Grassi A, Ballardini G. Post-liver transplant hepatitis C virus recurrence: an unresolved thorny problem. World J Gastroenterol. 2014; 20:11095–11115.
19. Charlton M, Gane E, Manns MP, Brown RS Jr, Curry MP, Kwo PY, et al. Sofosbuvir and ribavirin for treatment of compensated recurrent hepatitis C virus infection after liver transplantation. Gastroenterology. 2015; 148:108–117.
20. Korean Association for the Study of the Liver. KASL clinical practice guidelines: management of chronic hepatitis B. Clin Mol Hepatol. 2016; 22:18–75.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download