Abstract
Purpose
Predicting the need for surgical intervention among patients with intestinal obstruction is challenging. The delta neutrophil index (DNI) has been suggested as a useful marker of immature granulocytes, which indicate an infection or sepsis. In this study, we evaluated the impact of the DNI as an early predictor of operation among patients with intestinal obstruction.
Methods
A total of 171 patients who were diagnosed with postoperative intestinal obstruction were enrolled in this study. Medical records, including data for the initial CRP level, WBC count, and DNI were reviewed. Receiver operating characteristic (ROC) curves were generated to clarify the optimal DNI cutoff values for predicting an operation.
Results
Among the 171 patients, 38 (22.2%) needed surgical intervention. The areas under the initial CRP, WBC, and DNI ROC curves were 0.460, 0.449, and 0.543, respectively. The optimal cutoff value for predicting further surgical intervention according to the initial DNI level was 4.3%. The accuracy of the cutoff value was 74.9%, the sensitivity was 23.7%, and the specificity was 89.5% (positive predictive value, 23.7%; negative predictive value, 89.5%). In the multivariate analysis, initial DNI levels ≥ 4.3% were significantly associated with surgical intervention (odd ratio, 3.092; 95% confidence interval, 1.072–8.918; P = 0.037).
The proper management of intestinal obstruction has been a clinical challenge for surgeons for decades [12]. Once ischemic change develops, the mortality rate increases 2 to 10 times [3]. For this reason, various trials have examined ischemic change in the bowel among patients with intestinal obstruction to determine the most important predictive factors as well as proper management. For example, a recent study has suggested a multivariate prediction model that includes patient symptoms and findings from abdominopelvic CT [4]. Other researchers have proposed that the CRP levels increase with the severity of bacterial translocation during acute intestinal obstruction [5]. Nonetheless, even with these efforts, predicting the need for surgical intervention in patients with intestinal obstruction remains difficult.
However, the delta neutrophil index (DNI) was recently introduced as a new indicator of immature granulocytes [6], which indicate an infection or sepsis. Furthermore, the DNI has shown significant associations with disease severity and mortality among various diseases such as septic shock [678]. Therefore, given this strong correlation with infectious status, we evaluated the impact of the DNI as an early predictor of surgical intervention in patients with intestinal obstruction.
The medical records of 171 patients who were diagnosed with postoperative intestinal obstruction from January 2009 to December 2013 were extracted from our database and reviewed. All patients had a previous history of laparotomy and were initially treated using a conservative strategy. Patients who required immediate surgery for strangulated bowel at the time of diagnosis or those with intestinal obstruction such as gastrointestinal malignancy, inflammatory bowel disease, or incarcerated hernia were excluded.
Symptoms of intestinal obstruction include nausea, vomiting, abdominal distension, and intermittent abdominal pain. Plain abdominal X-ray radiographs showed definite air-fluid levels in the small bowel but no evidence of gas within the colon. Blood chemistry and laboratory tests, including the CRP level, WBC count, and DNI, were performed for all 171 patients upon admission.
The DNI was analyzed by an automatic cell analyzer (ADIVA 2120 Hematology system, Siemens Healthcare, Erlangen, Germany). DNI was calculated using the following formula:
DNI = [neutrophil and eosinophil subfraction measured in the myeloperoxidase (MPO) channel by cytochemical MPO reaction] – [polymorphonuclear (PMN) subfraction measured in the nuclear lobularity channel by the reflected light beam]
Because there were no signs of strangulation, conservative management was the first choice of treatment for all 171 patients. Decompression with a nasogastric tube and intravenous fluid resuscitation was performed. The patients were encouraged to start ambulation to recover bowel movement. If gas passage was confirmed with improvement on radiologic findings, the nasogastric tube was removed and the diet was built up.
Indications for surgical intervention were based on close monitoring of clinical symptoms and serial radiologic findings. The final decision for surgical intervention was made by each patient's surgeon.
IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA) was used for all statistical analyses. Categorical variables were analyzed using chi-square tests or Fisher exact tests, and continuous variables were analyzed using Mann-Whitney U-tests. Univariate and multivariate analyses were performed using logistic regression analysis. P < 0.05 was considered statistically significant.
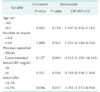
Receiver operating characteristic (ROC) curves were generated to clarify the optimal DNI cutoff level for predicting surgical intervention. The role of the DNI in predicting surgical intervention was evaluated by the area under the ROC curve (AUC). The optimal cutoff level was determined by drawing a line connecting the points nearest to the left-upper corner. This method for determining the optimal cutoff level accounts for the trade-off between sensitivity and specificity over a continuous range [9].
The clinical characteristics of enrolled patients are described in Table 1. The median age of the patients was 60 years old and gastrointestinal surgery was the most common type of previous operation. The median initial DNI value was 0.8% (range, 0.0%–22.4%). Surgical intervention was performed on 38 patients (22.2%) (Table 1). Of the 38 patients, 23 patients had operations due to adhesion band without bowel ischemia. Thirteen patients underwent bowel resections due to bowel ischemia, and the other 2 patients underwent bypass surgeries for intestinal obstruction caused by recurrent cancer. The median initial DNI value was not significantly different between patients with and patients without surgical intervention (0.9% vs. 1.0%, respectively, P = 0.929) (Fig. 1).
The ROC curve demonstrated that the optimal DNI cutoff level for predicting surgical intervention in patients with postoperative intestinal obstruction was 4.3%. This cutoff level had a sensitivity of 23.7%, a specificity of 89.5%, and an accuracy of 74.9% (Fig. 2). The AUC was 0.543 (≥0.5), which suggests that the DNI has a role in predicting surgical intervention. The initial CRP and WBC count values failed to demonstrate a role as a predictor of surgical intervention.
When we compared the surgical intervention rate with the DNI cutoff level, we found that patients with an initial DNI ≥ 4.3% underwent surgical intervention more frequently (DNI ≥ 4.3% = 39.1% vs. DNI < 4.3% = 19.6%); results were statistically significant (P = 0.036). In addition, patients with an initial DNI ≥ 4.3% showed higher CRP levels compared to patients with an initial DNI < 4.3% (DNI ≥ 4.3% = 51.0 mg/L vs. DNI < 4.3% = 2.7 mg/L, P = 0.001) (Table 2). In the multivariate risk factor analysis including other clinically related factors, an initial DNI ≥ 4.3% was the only significant predictor of surgical intervention (Table 3).
In this study, we found that surgical intervention was needed more often among patients with an initial DNI ≥ 4.3% than among patients with an initial DNI < 4.3%. Moreover, having a DNI ≥ 4.3% at admission was the sole factor in predicting the need for surgical intervention among patients with postoperative intestinal obstruction.
Many studies have attempted to define the optimal prediction model for determining the need for surgical intervention among patients with intestinal obstruction. For example, Zielinski et al. [10] recently proposed and validated a multivariate small-bowel obstruction model to predict the necessity of surgical intervention based on 4 risk factors including vomiting, small bowel feces sign, free intraperitoneal fluid, and mesenteric edema [4]. On the other hand, another study has suggested a simple model using age, the presence of ascites, and drainage volume through a decompression tube [11]. However, a consensus regarding the proper time for surgical intervention in cases of intestinal obstruction has not been reached.
In light of this, the DNI, which corresponds to the fraction of immature granulocytes in the circulating blood, has been introduced as a prognostic marker for various diseases [121314], especially sepsis [6781516] and bacteremia [171819]. Since the DNI can be easily calculated from the peripheral circulating blood by subtracting the fraction of mature PMN leukocytes from the sum of MPO-reactive cells, its correlation with patient prognosis has been well established.
However, an experimental model of intestinal obstruction demonstrated that the mucosal barrier was disrupted after 24 hours in all intestinal obstruction cases [20]. This then allows bacteria to migrate through this disrupted mucosa to the systemic circulation and can cause sepsis [2122]. A subsequent elevation of the immature/total granulocyte ratio or the banded neutrophil count, i.e., left-shift, can then occur [23]. Therefore, the mechanism of bowel ischemia must be considered in cases of intestinal obstruction. Thus, we hypothesized that the DNI might help detect the moment when bacterial translocation causes sepsis and thus signals a need for surgical intervention among patients with intestinal obstruction.
This study has some limitations. For example, we were not able to standardize the treatment for all patients as the treatment depended on the individual surgeon's preference. Furthermore, because of the retrospective nature of this analysis, the evaluation tool for disease progress and improvement could not be scheduled in a regular format. Most importantly, the optimal cutoff value of the DNI (≥4.3%) showed a low discriminatory power (sensitivity of 23.7%) and detected only 9 of 38 patients who underwent surgery. However, given that the mean interval between admission and operation was 5.3 days, this might be because some surgeons decided to intervene surgically even in patients without evidence of septic condition. Finally, even though our hypothesis was based on the organic relationship between bacterial location, the DNI, and septic condition in patients with postoperative intestinal obstruction, further prospective studies using strict standardization of the treatment methods are needed to help clarify the results.
In conclusion, even though postoperative intestinal obstruction is usually managed based on clinical symptoms and the preference of the surgeon, our results indicate that the initial DNI level in patients with intestinal obstruction can be a useful predictor for determining surgical intervention.
Figures and Tables
Fig. 1
Initial level of delta neutrophil index (DNI) in patients with or without surgical intervention.

Fig. 2
Receiver operating characteristic (ROC) curve of delta neutrophil index (DNI) in enrolled patients. AUC, area under the ROC curve.
References
1. Mucha P Jr. Small intestinal obstruction. Surg Clin North Am. 1987; 67:597–620.
2. Bizer LS, Liebling RW, Delany HM, Gliedman ML. Small bowel obstruction: the role of nonoperative treatment in simple intestinal obstruction and predictive criteria for strangulation obstruction. Surgery. 1981; 89:407–413.
3. Cheadle WG, Garr EE, Richardson JD. The importance of early diagnosis of small bowel obstruction. Am Surg. 1988; 54:565–569.
4. Schein M, Assalia A. Small bowel obstruction-who needs an operation. World J Surg. 2010; 34:920–922.
5. Cevikel MH, Ozgun H, Boylu S, Demirkiran AE, Aydin N, Sari C, et al. C-reactive protein may be a marker of bacterial translocation in experimental intestinal obstruction. ANZ J Surg. 2004; 74:900–904.
6. Nahm CH, Choi JW, Lee J. Delta neutrophil index in automated immature granulocyte counts for assessing disease severity of patients with sepsis. Ann Clin Lab Sci. 2008; 38:241–246.
7. Seok Y, Choi JR, Kim J, Kim YK, Lee J, Song J, et al. Delta neutrophil index: a promising diagnostic and prognostic marker for sepsis. Shock. 2012; 37:242–246.
8. Park BH, Kang YA, Park MS, Jung WJ, Lee SH, Lee SK, et al. Delta neutrophil index as an early marker of disease severity in critically ill patients with sepsis. BMC Infect Dis. 2011; 11:299.
9. Soreide K, Korner H, Soreide JA. Diagnostic accuracy and receiver-operating characteristics curve analysis in surgical research and decision making. Ann Surg. 2011; 253:27–34.
10. Zielinski MD, Eiken PW, Heller SF, Lohse CM, Huebner M, Sarr MG, et al. Prospective, observational validation of a multivariate small-bowel obstruction model to predict the need for operative intervention. J Am Coll Surg. 2011; 212:1068–1076.
11. Komatsu I, Tokuda Y, Shimada G, Jacobs JL, Onodera H. Development of a simple model for predicting need for surgery in patients who initially undergo conservative management for adhesive small bowel obstruction. Am J Surg. 2010; 200:215–223.
12. Park HJ, Ha YJ, Pyo JY, Park YB, Lee SK, Lee SW. Delta neutrophil index as an early marker for differential diagnosis of adult-onset Still's disease and sepsis. Yonsei Med J. 2014; 55:753–759.
13. Pyo JY, Park JS, Park YB, Lee SK, Ha YJ, Lee SW. Delta neutrophil index as a marker for differential diagnosis between flare and infection in febrile systemic lupus erythematosus patients. Lupus. 2013; 22:1102–1109.
14. Lim TS, Kim BK, Lee JW, Lee YK, Chang S, Kim SU, et al. Use of the delta neutrophil index as a prognostic factor of mortality in patients with spontaneous bacterial peritonitis: implications of a simple and useful marker. PLoS One. 2014; 9:e86884.
15. Zanaty OM, Megahed M, Demerdash H, Swelem R. Delta neutrophil index versus lactate clearance: early markers for outcome prediction in septic shock patients. Alexandria J Med. 2012; 48:327–333.
16. Hwang YJ, Chung SP, Park YS, Chung HS, Lee HS, Park JW, et al. Newly designed delta neutrophil index-to-serum albumin ratio prognosis of early mortality in severe sepsis. Am J Emerg Med. 2015; 33:1577–1582.
17. Kim HW, Ku S, Jeong SJ, Jin SJ, Han SH, Choi JY, et al. Delta neutrophil index: could it predict mortality in patients with bacteraemia. Scand J Infect Dis. 2012; 44:475–480.
18. Lee CH, Kim J, Park Y, Park YC, Kim Y, Yoon KJ, et al. Delta neutrophil index discriminates true bacteremia from blood culture contamination. Clin Chim Acta. 2014; 427:11–14.
19. Kim HW, Yoon JH, Jin SJ, Kim SB, Ku NS, Jeong SJ, et al. Delta neutrophil index as a prognostic marker of early mortality in gram negative bacteremia. Infect Chemother. 2014; 46:94–102.
20. Antequera R, Bretana A, Cirac A, Brito A, Romera MA, Zapata R. Disruption of the intestinal barrier and bacterial translocation in an experimental model of intestinal obstruction. Acta Cient Venez. 2000; 51:18–26.
21. Liolios A, Oropello JM, Benjamin E. Gastrointestinal complications in the intensive care unit. Clin Chest Med. 1999; 20:329–345. viii.
22. Akyildiz M, Ersin S, Oymaci E, Dayangac M, Kapkac M, Alkanat M. Effects of somatostatin analogues and vitamin C on bacterial translocation in an experimental intestinal obstruction model of rats. J Invest Surg. 2000; 13:169–173.
23. Cornbleet PJ. Clinical utility of the band count. Clin Lab Med. 2002; 22:101–136.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download