Abstract
Purpose
Central pancreatectomy (CP) may be indicated for the treatment of benign or low-grade malignant tumor in the neck and proximal body of the pancreas. Pancreatic fistula is one of the most common complications after CP. In this study, we suggested an inverted mattress pancreaticojejunostomy (IM-PJ) technique to decrease the risk of pancreatic fistula.
Methods
Between 2010 and 2015, CP was performed with IM-PJ for 10 consecutive patients with a benign or low-grade malignant tumor in the neck and proximal body of the pancreas. All clinical and pathological data were analyzed retrospectively.
Results
Median age was 56.4 years (range, 17–75 years). Median surgery duration was 286 minutes (range, 205–410 minutes). In all cases, the distal stump was reconstructed using the IM-PJ method. Median duration of hospital stay was 23.8 days (range, 9–53 days). No patient mortality occurred. Pancreatic fistula developed in 9 cases (90%); however, all fistulas were grade A and resolved without surgical or radiological intervention. Nine patients remain well with no recurrence or new endocrine or exocrine dysfunction.
Central pancreatectomy (CP) is a pancreas parenchyma sparing surgical procedure. This procedure was first suggested in the 1950s as a treatment for chronic pancreatitis and in the treatment of a traumatic pancreatic injury [1]. Recently, CP has been used in the removal of benign and low-grade malignant lesions located in the neck and proximal body of the pancreas. Unlike conventional pancreatic resections, CP has the advantages of avoiding extended resection of the pancreas and preserving pancreatic endocrine and exocrine function [2].
While CP is typically considered to be a ‘safe and reason able’ procedure, it is associated with a high incidence of post operative pancreatic fistula (POPF) because surgeons must manage 2 cut surfaces (proximal and distal) after segmental resection of the pancreas. Following the closure of the proximal remnant with hand-sewn or staple sutures and reconstruction of distal pancreaticoenteric anastomosis, resected cephalic end and anastomosis are at risk of leakage. For this reason, various studies have compared the incidence of pancreatic fistula after CP with conventional procedures, and various techniques for the reconstruction of the distal pancreatic remnant that aim to reduce POPF have been proposed [34].
In a previous study, we introduced an ‘inverted mattress pancreaticojejunostomy (IM-PJ)’ technique for decreasing the risk of pancreatic fistula and subsequent serious complications after pancreaticoduodenectomy (PD) [5]. IM-PJ effectively decreased the incidence of pancreatic fistula and related complications in our data series.
In this study, we present our experiences of CP with IM-PJ reconstruction of the distal end, focusing in particular on POPFs as defined by the International Study Group for Pancreatic Fistula (ISGPF).
Between March 2010 and June 2015, 10 patients who underwent CP were identified from medical records at Kyungpook National University Chilgok Hospital. Hospital charts, radiographic images and pathological reports were reviewed retrospectively. Demographic variables, preoperative symptoms, preoperative workup, intraoperative factors, and postoperative course, and pathological findings were obtained from medical records retrospectively. Preoperative diagnosis was based on CT scanning. For those patients in whom CT scan was not sufficient to make a diagnosis, other imaging studies, including MRI and endoscopic ultrasound (EUS) were undertaken at the discretion of the surgeon or referring physician. Follow-up data with clinical, radiologic, and laboratory outcomes were assessed via outpatient medical records every 6 or 12 months. Tumors were classified according to the World Health Organization Classification of exocrine and endocrine pancreatic neoplasm.
The study protocol was approved by Kyungpook National University Medical Center Institutional Review Board (approval number: KNUMC 2016-10-016).
An upper midline incision was employed in all patients to access to the peritoneal cavity. Dissection began with the division of the gastrocolic ligament to enter into the lesser sac. Pancreatic dissection was initiated inferiorly along the superior mesenteric vein. A tunnel formed at the pancreatic neck in order to separate the parenchyma from the posterior superior mesenteric vein, portal vein confluence. Nylon tape was placed behind the pancreas to protect the vascular structures before dividing the pancreas. The splenic artery was subsequently dissected from the superior border of the pancreas. The pancreas was transected using a linear stapler and the pancreatic tail was dissected free from the splenic vein. The distal pancreatic stump was reconstructed using an IM-PJ technique, which was based on our IM-PJ technique [5] (Fig. 1). Before abdominal closure, a closed suction drain was placed around the proximal resection stump and/or IM-PJ anastomosis to monitor for pancreatic leakage and amylase content in the effluent.
(1) Antimesenteric border of the proximal jejunum measuring the same size as the pancreatic cut surface was longitudinally opened.
(2) A p-duct stent was placed on the p-duct and proximal jejunum before IM technique procedure start. Three-to-four U-shaped mattress sutures (4-0 Prolene) were placed starting at the serosa of the posterior jejunal wall and going out-in through the full thickness of the jejunum. Then, inverted seromuscular stitches were placed going in-out (Fig. 1A).
(3) These sutures penetrated the pancreatic remnant in a straight manner (Fig. 1B).
(4) The seromuscular layer of the anterior jejunal wall was inverted by the transpancreatic U-shaped sutures going out-in followed by a full thickness stitch in the anterior jejunal wall going in-out, thereby invaginating the pancreatic remnant into the lumen of the jejunum (Fig. 1C).
(5) A U-shaped suture was placed in a corner of the jejunum starting at the serosa of the jejunal wall and going out-in through the full thickness of the jejunum. Then, an inverted seromuscular stitch was placed going in-out. The suture penetrated an end of the pancreas stump in a straight manner, then the seromuscular layer of the other jejunal wall was inverted by the transpancreatic U-shaped suture going out-in followed by a full thickness stitch in the jejunal wall going in-out. Finally, in the same way, a U-shaped suture at the other corner of the jejunum fixed the other end of the pancreas.
(6) The 5–6 U-shaped sutures, including the sutures at both corners of the jejunum, were pulled over using adequate tension (Fig. 1D) and tied at the anterior wall and at both corners of the jejunum, thereby enclosing the jejunal opening around the remnant pancreas. A p-duct stent was fixed on the Roux limb stump using three or four sutures for prevention of spontaneous removal (Fig. 1E).
The drain fluid was routinely tested for amylase on postoperative days 1, 3, 5 and an additional day when needed. The general definition provided by the ISGPF is as follows: a drain output of any measurable volume after postoperative day 3 with amylase content greater than 3 times the serum amylase activity. Patients with pancreatic fistula were classified into grades A, B, or C [6]. If the drain amylase was less than three times the serum amylase, the drain was removed. If not, the drain was retained until the drain output was <10 mL/day [7].
Postoperative complications were graded on a scale from 0 to 5 according to the Clavien-Dindo Classification.
Postoperative mortality was defined as all deaths before hospital discharge or up to 90 days following surgery. Patients were typically discharged after recovery from a medical condition or complete resolution of POPFs. Therefore, some patients retained the closed drain after discharge and the condition of their drain was followed up in an outpatient department. The surgeon decided whether the drain was to be removed or not according to the previously described criteria.
Patients were diagnosed with diabetes mellitus (DM) according to the World Health Organization's definition: (1) a single elevated plasma glucose reading with symptoms, (2) raised values on 2 occasions of either fasting plasma glucose (>126 mg/dL) or a positive oral glucose tolerance test (a plasma level > 140 mg/dL at 2 hours after oral consumption of 1.75-g glucose per kg body weight). Incidence of DM was reviewed for all cases in preoperative and postoperative conditions.
Pancreatic exocrine insufficiency was defined as diarrhea, steatorrhea, and weight loss, which improved with pancreatic enzyme replacement in some cases [8].
Postoperative pathological outcomes were compared with suspected preoperative diagnosis retrospectively. Long-term complications included incisional hernia, small bowel obstruction, persistent POPFs (>90 days), pseudocyst, and superior mesenteric vein thrombosis [9].
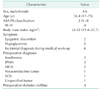
The present analysis included 6 female and 4 male patients, with a median age of 56.4 years (range, 17–75 years) and a mean American Society of Anesthesiologists (ASA) physical status classification of II. The mean body mass index was 24.32 kg/m2 (range, 19.4–35.7 kg/m2). Two patients presented with epigastric discomfort, and 2 patients experienced with episodes of hypoglycemia. However, >50% of patients did not have any symptoms and their respective pancreatic lesions were detected incidentally during medical work-up. Four patients had DM before CP. Preoperative diagnoses included insulinoma, intraductal papillary mucinous neoplasm, mucinous cystic neoplasm, neuroendocrine tumor, serous cystadenoma, and unspecified tumor (Table 1).
The mean operative time was 286 minutes (range, 205–410 minutes). Two patients were in surgery for >400 minutes because of previous operative adhesion and simultaneous common bile duct exploration for choledocholithiasis. The mean intraoperative estimated blood loss was 490 mL (range, 200–1,000 mL) and 2 patients received packed cell transfusion in the operative field. The spleen was preserved in all patients.
In 3 cases, the proximal stump was stapled only, whereas in 7 cases, this stump was over-sewn by a continuous running suture using nonabsorbable 4-0 sutures. In all patients, end-to-side IM-PJ of the distal stump was performed and closed suction drains were placed on the proximal stump and distal IM-PJ anastomosis. Nine patients had an external pancreatic stent of IM-PJ; however, 1 patient did not have this stent due to atrophy of the distal pancreatic remnant.
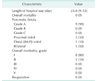
In the final pathological report, the mean tumor size was 34.3 mm and the mean length of resected pancreas was 54.9 mm. One patient who was preoperatively diagnosed with an unspecified tumor revealed a desmoid tumor, and a patient with suspected insulinoma preoperatively was finally confirmed as neuroendocrine tumor after surgery. All resection margins were microscopically negative (Table 2).
Postoperative results are summarized in Table 3. The mortality rate was 0 and no patient required reoperation. The overall morbidity rate was 90%, although there were no severe complications (Clavien-Dindo Classification III–V). POPFs were the main cause of postoperative complications and occurred in 90% of patients; all cases were POPF grade A. POPFs were presumed to originate from the proximal pancreatic stump in 30% of patients and from the IM-PJ in 10% and were bilateral in 50%. In 1 case, wound complications occurred with POPFs and this was resolved via bedside suture under local anesthesia. None of the patients required additional percutaneous drains, diet management (nothing by mouth and/or total parenteral nutrition), or medical treatment (for example, Octreotide). POPFs were controlled with intraoperative inserted-closed suction drains. The mean duration of hospital stay was 23.8 days (range, 9-53 days).
With the mean follow-up of 30.5 months (range, 1–64 months), patients remained well without evidence of recurrence and 1 patient succumbed to advanced prostate cancer. In conventional pancreatic resections (distal pancreatectomy and PD), pancreatic parenchyma was extended and resected, and postoperative pancreatic endocrine and exocrine function could be decreased. However, no patients experienced new onset of DM or preexisting DM worsening. One patient had diarrhea and steatorrhea that recovered without pancreatic enzyme replacement (Table 4).
After a mean follow-up of 30.5 months, there was 1 long-term complication, superior mesenteric vein partial thrombosis. However, this partial thrombosis was not associated with any symptoms and was relieved naturally during the outpatient follow-up period.
Traditionally, formal pancreatectomy, which includes pancreatoduodenectomy and distal pancreatectomy, may involve excessive resection of the normal pancreatic parenchyma and be associated with the risk of postoperative DM and exo- and endocrine pancreatic insufficiency. Because of this, CP has been suggested as an alternative procedure for the treatment of benign and low-grade tumors located in the neck or body of the pancreas [10]. This procedure preserves normal pancreatic tissue, particularly insulin cells that are predominantly located in the pancreatic body and tail, thus avoiding the risk of DM, exo- and endocrine pancreatic insufficiency. Furthermore, preservation of the spleen is another major advantage of CP, as it eliminates the infective and hematological complications associated with splenectomy. However, these benefits may be surpassed by the increased pancreatic fistula rate associated with CP. It has been reported that the POPFs rate after CP is higher than after PD or DP (average rate: 30%–40%), because of the presence of 2 pancreatic resection stumps. Conversely, soft pancreas texture and a small sized main pancreatic duct may be risk factors associated with the development of POPFs. Since POPFs remains one of the most common complications, many groups have suggested various techniques for the prevention of POPFs. In particular, there have been various reports related to distal pancreatic stump management as the fistula originating from the distal pancreatic anastomosis had poorer clinical results than the proximal remnant. Xiang et al. [11] reported that pancreaticogastrostomy (PG) of the distal pancreatic remnant reduced the occurrence of pancreatic fistula; whereas Venara's group showed that there was a lower anastomotic leakage rate with pancreaticojejunostomy (PJ) than PG [12]. Some groups have suggested that the type of reconstruction (PG or PJ) did not affect the rates of formation of POPFs [13]. Therefore, controversy remains concerning the ideal distal pancreatic anastomosis for decreasing POPFs.
In our study, using the IM-PJ technique for reconstruction of distal pancreatic stump, the incidence of all pancreatic fistula grades was 90%. The incidence of POPFs following CP with IM-PJ is apparently higher than the generally accepted pancreatic leak rate. In grade A POPF, closed suction drains were not necessary for monitoring of pancreatic leakage if there are no clinical doubts for POPFs. That is, if we did not place drains on both stumps, POPFs could not have been discovered. We inserted drains and checked the amylase levels regularly, so the grade A POPF rate might be higher than in any other studies. However, there were no grades B and C POPFs detected, especially postpancreatectomy hemorrhage (PPH) was not observed. In addition, there were no additional surgical treatments or radiological interventions for the control of POPFs. There was no mortality and no cases required reoperation. For POPFs management, closed suction drains were retained until the drain fluid amylase levels were less than three times that of serum amylase, or when drain output was <10 mL/day.
In the present cases, the external pancreatic stents may have reduced the high-grade POPFs as some reports have suggested that an external pancreatic duct stent may reduce the occurrence and severity of POPFs after pancreatic resection [14]. However, there is a dissenting opinion about the effect of external or internal stent for preventing POPFs, so our data have a limitation in proving the stent's effect.
No patient without preoperative diabetes developed new onset DM after successful CP during the follow-up period. A literature review reported that the rate of de novo DM following CP is 0%–7.7% [15]. The incidence of new-onset DM after PD is 10%–15%, which increases up to 40% in patients with chronic pancreatitis [1617]. Notably, about 25%–90% new-onset DM developed after distal pancreatectomy for chronic pancreatitis [1718]. As our experience and other recent reports suggest, CP could preserve pancreatic function.
There was a low rate of long-term complications and one complication spontaneously recovered during the outpatient follow-up period without additional medical or surgical treatments.
Although there are some limitations to our report, (e.g., a retrospective study and a small number of cases), there were no clinically meaningful grades B and C POPFs, PPH, new onset DM and/or preexisting DM worsening.
In conclusion, our data suggested that the IM-PJ method after CP probably could be effective and feasible for the prevention of high-grade POPFs and preservation of pancreatic exocrine and endocrine functions.
Figures and Tables
Fig. 1
Inverted mattress pancreaticojejunostomy technique. (A) Three to 4 U-shaped mattress sutures were placed starting at the serosa of the posterior jejunal wall. The inverted seromuscular stitches were made going in-out. (B) These sutures penetrated the pancreatic remnant in a straight manner. (C) After penetrating the pancreatic parenchyma with a needle, the seromuscular layer of the anterior jejunal wall was inverted with the sutures going out-in, followed by a full thickness stitch of the anterior jejunal wall going in-out. (D) The U-shaped sutures were pulled with adequate tension and tied at the anterior wall and both corners of the jejunum. (E) A p-duct stent was fixed on theRoux limb stump using three or four sutures for prevention of spontaneous removal.

References
1. Letton AH, Wilson JP. Traumatic severance of pancreas treated by Roux-Y anastomosis. Surg Gynecol Obstet. 1959; 109:473–478.
2. Zhou YM, Zhang XF, Wu LP, Su X, Li B, Shi LH. Pancreatic fistula after central pancreatectomy: case series and review of the literature. Hepatobiliary Pancreat Dis Int. 2014; 13:203–208.
3. Goldstein MJ, Toman J, Chabot JA. Pancreaticogastrostomy: a novel application after central pancreatectomy. J Am Coll Surg. 2004; 198:871–876.
4. Iacono C, Verlato G, Ruzzenente A, Campagnaro T, Bacchelli C, Valdegamberi A, et al. Systematic review of central pancreatectomy and meta-analysis of central versus distal pancreatectomy. Br J Surg. 2013; 100:873–885.
5. Kwon HJ, Ha HT, Choi YY, Kim SG. The effects of the end-to-side inverted mattress pancreaticojejunostomy on postoperative pancreatic fistula: a single surgeon's experience. Ann Surg Treat Res. 2015; 89:61–67.
6. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13.
7. Brown KM, Shoup M, Abodeely A, Hodul P, Brems JJ, Aranha GV. Central pancreatectomy for benign pancreatic lesions. HPB (Oxford). 2006; 8:142–147.
8. Ocuin LM, Sarmiento JM, Staley CA, Galloway JR, Johnson CD, Wood WC, et al. Comparison of central and extended left pancreatectomy for lesions of the pancreatic neck. Ann Surg Oncol. 2008; 15:2096–2103.
9. Goudard Y, Gaujoux S, Dokmak S, Cros J, Couvelard A, Palazzo M, et al. Reappraisal of central pancreatectomy a 12-year single-center experience. JAMA Surg. 2014; 149:356–363.
10. Zhou J, Dong M, Kong F, Li Y, Tian Y. Central pancreatectomy for benign tumors of the neck and body of the pancreas: report of eight cases. J Surg Oncol. 2009; 100:273–276.
11. Xiang GM, Tan CL, Zhang H, Ran X, Mai G, Liu XB. Central pancreatectomy for benign or borderline lesions of the pancreatic neck: a single centre experience and literature review. Hepatogastroenterology. 2012; 59:1286–1289.
12. Venara A, de Franco V, Mucci S, Frampas E, Lermite E, Regenet N, et al. Central pancreatectomy: comparison of results according to the type of anastomosis. J Visc Surg. 2012; 149:e153–e158.
13. Sauvanet A, Partensky C, Sastre B, Gigot JF, Fagniez PL, Tuech JJ, et al. Medial pancreatectomy: a multi-institutional retrospective study of 53 patients by the French Pancreas Club. Surgery. 2002; 132:836–843.
14. Zhou Y, Yang C, Wang S, Chen J, Li B. Does external pancreatic duct stent decrease pancreatic fistula rate after pancreatic resection?: a meta-analysis. Pancreatology. 2011; 11:362–370.
15. Kang CM, Lee JM, Kim MW, Yoon DS, Park JS, Lee WJ. Experiences in central pancreatectomy. Dig Surg. 2011; 28:57–62.
16. Jalleh RP, Williamson RC. Pancreatic exocrine and endocrine function after operations for chronic pancreatitis. Ann Surg. 1992; 216:656–662.
17. Slezak LA, Andersen DK. Pancreatic resection: effects on glucose metabolism. World J Surg. 2001; 25:452–460.
18. Hutchins RR, Hart RS, Pacifico M, Bradley NJ, Williamson RC. Long-term results of distal pancreatectomy for chronic pancreatitis in 90 patients. Ann Surg. 2002; 236:612–618.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download