Abstract
Purpose
To compare the outcome between laparoscopic gastrojejunostomy (LapGJ) and duodenal stenting (DS) in terms of oral intake, nutritional status, patency duration, effect on chemotherapy and survival.
Methods
Medical records of 115 patients, who had LapGJ or duodenal stent placement between July 2005 and September 2015 in Seoul National University Bundang Hospital, have been reviewed retrospectively. Oral intake was measured with Gastric Outlet Obstruction Scoring System. Serum albumin and body weight was measured as indicators of nutritional status. The duration of patency was measured until the date of reintervention. Chemotherapy effect was calculated after the procedures. Survival period and oral intake was analyzed by propensity score matching age, sex, T-stage, comorbidities, and chemotherapy status.
Results
Forty-three LapGJ patients and 58 DS patients were enrolled. Improvement in oral intake was shown in LapGJ group versus DS group (88% vs. 59%, P = 0.011). Serum albumin showed slight but significant increase after LapGJ (+0.75 mg/dL vs. −0.15 mg/dL, P = 0.002); however, there was no difference in their body weight (+5.1 kg vs. −1.0 kg, P = 0.670). Patients tolerated chemotherapy longer without dosage reduction after LapGJ (243 days vs. 74 days, P = 0.006) and maintained the entire chemotherapy regimen after the procedure longer in LapGJ group (247 days vs. 137 days, P = 0.042). LapGJ showed significantly longer survival than DS (220 vs. 114 days, P = 0.004).
Gastric outlet obstruction (GOO) most commonly occurs in patients with advanced cancer such as gastric cancer, duodenal cancer, and periampullary cancer [1]. About 50% of all patients with GOO present with nausea and vomiting, even when mechanical obstruction is not visible in radiologic examinations [2].
There are several treatments available including gastrojejunostomy (GJ), duodenal stenting (DS), and enteral or intravenous hyperalimentation [3]. Traditionally, those with good performance status despite underlying diseases underwent palliative bypass surgeries, most commonly a GJ [4]. Patients who are not expected to withstand general anesthesia and endure postoperative burden, have typically been candidates of DS. Most patients tend to be poor surgical candidates due to malnutrition [5].
Many studies have reported that DS is a relatively simpler and safer alternative procedure to GJ for management of malignant GOO [678]. GJ and DS have very high success rates of over 90%, which means 9 out of 10 patients resume oral intake [59]. Although GJ has higher rates of early morbidity and mortality than DS, recent studies have reported GJ to be much more durable and to require less reintervention than DS [10]. However, debate still remains as to which method has a better outcome in survival, oral intake, or quality of life in the long term.
With the introduction of laparoscopic technique, surgeons began to adopt laparoscopy for many types of surgeries, such as cholecystectomy, gastrectomy, and colectomy. Laparoscopic gastrojejunostomy (LapGJ) was one of these attempts. Few studies have reported open GJ in associated with higher morbidity and mortality than LapGJ [911].
Most of the patients who undergo palliative procedures like LapGJ or DS receive chemotherapy either before or after. Since LapGJ or DS is done to relieve symptoms, chemotherapy is important in the whole treatment process.
The objective of this study is to compare the long-term outcome between LapGJ and DS in oral intake, nutritional status, patency duration, effect on chemotherapy, and survival.
We performed a retrospective study of 115 patients who underwent LapGJ or DS for GOO with unresectable gastric cancer only between July 2005 and September 2015 in Seoul National University Bundang Hospital. Fourteen patients were excluded because they did not have follow-up records after discharge. Therefore, 58 and 43 patients who had undergone DS and LapGJ, respectively, were evaluated. Patient characteristics are shown in Table 1. All the surgeries were done by 2 experienced surgeons from the start.
LapGJ consisted of 4 incisions for trocar insertion. A 12-mm-sized umbilical port was used for a flexible scope, and a 12-mm trocar and a 5-mm trocar were inserted on the operator's side (right) in a V shape, 8–9 cm apart. An additional 5-mm trocar was inserted on the 1st assistant's side (left) for minimal support. Linear staplers were used for intracorporeal GJ. Anastomosis was done on the posterior wall of the stomach body with the closest part of the jejunum from the stomach, either antecolic or retrocolic. A small hole on the stomach posterior side and the jejunum was made for linear stapler entry. For the common entry hole, one additional linear stapler was used in some cases, and interrupted intracorporeal sutures were used in others.
DS was performed using either endoscopic or fluoroscopic guidance. The stent was introduced over a guidewire and deployed under fluoroscopic monitoring. Twelve cases were done solely by endoscopy and nine cases were done only by fluoroscopy. However, most of the cases (n = 37) were performed with fluoroscopy by intervention radiologists and were checked by endoscopists to confirm adequate placement.
Oral intake was measured with the widely known Gastric Outlet Obstruction Scoring System (GOOSS: 0, no oral intake, 1, liquids only; 2, soft solids; 3, low-residue or full diet) (Table 2) [5]. GOOSS was measured after LapGJ or DS before discharge and compared with the value after 1 month of follow-up. GOOSS was evaluated through detailed chart review, individually, to see whether there was any improvement or deterioration in oral intake after each procedure. Improved or maintained diet after discharge was compared between the 2 groups. Only patients matched with age, sex, T-stage, comorbidities, and chemotherapy status using the propensity scoring method were evaluated.
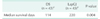
Nutritional status was estimated with serum albumin levels and body weight measurements (Table 3). The values before the procedure and 1 month after the procedure were compared.
Duration of patency after the procedure was defined as the period until reintervention. In obstruction cases, DS patients underwent additional stenting. However, LapGJ patients underwent de novo stent placements instead of surgery. Several types of stent obstructions were observed in DS group (Table 4).
The effects on chemotherapy were analyzed in 2 manners (Table 5). Tolerance without dose reduction was calculated by reviewing medical charts for duration until dose reduction of regimen due to patient condition after the procedure. Maintenance days were calculated from start of chemotherapy after the procedure until the final chemotherapy.
Survival was calculated from the date of the procedure until death (Table 6). Patients were matched with the propensity scoring method, the same as in GOOSS analysis.
The statistical calculations of this study were done with the statistical software R (Version 3.3.2, R Foundation for Statistical Computing, Vienna, Austria).
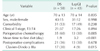
Table 1 shows baseline patient characteristics for the 2 groups. There was no difference in age, sex, comorbidity, or clinical T-stage. Comorbidity consists of cardiovascular, respiratory, cerebrovascular problems, and diabetes mellitus. DS patients had significantly more chemotherapy than LapGJ patients (60% vs. 30%, P = 0.005). Most DS patients were already going through chemotherapy while LapGJ patients started their chemotherapy after the procedure. Complications were evaluated according to Clavien-Dindo (CD) classification [12]. Postoperative complications did not differ between the 2 groups, but in DS group there were significantly more severe complications over CD grade IIIa (intervention needed not under general anesthesia) (17 patients vs. 4 patients, P = 0.015). There were 25 cases of stent reinterventions in 17 DS patients, and 2 cases of percutaneous transhepatic biliary drainage due to CBD obstruction by tumor (CD IIIa), 1 case of small bowel resection and anastomosis due to ileus under general anesthesia (CD IIIb), and 1 case of ICU care due to aspiration pneumonia in four GJ patients (CD IVa).
Short-term outcomes were evaluated between the 2 groups in 2 categories: time to first meal and postoperative complications during admission. DS group demonstrated significantly shorter time to first meal than LapGJ group (1.9 days vs. 3.2 days, P < 0.001). There were no postoperative complications during admission after DS but in 7 patients (16%) from LapGJ group. Patients presented with ileus in 5 cases and infection in 2 cases.
Table 2 shows GOOSS for each group. Two groups were matched with the propensity scoring method for more accurate analysis. In the DS group, patients who were able to tolerate full diet decreased after a 1-month interval (25 to 12 patients) and those with no intake increased from 1 patient to 4. After LapGJ, 74% of the patients could tolerate full diet and after 1 month rates did not decrease. When we compared the patients who showed undiminished diet, there was significant difference between LapGJ and DS groups (88% vs. 59%, P = 0.011). GOOSS was analyzed using the Wilcoxon signed rank test.
Table 3 shows serum albumin and body weight change between the 2 groups from before and 1 month after the procedure. Serum albumin levels showed significant change between LapGJ and DS groups (+0.75 mg/dL vs. -0.15 mg/dL, P = 0.002). However, no significant change was found in terms of body weight (-1 kg vs. +5.1 kg, P = 0.670).
Several patients from both groups showed recurrent obstructive symptoms (Table 4). Those who had DS previously went through stent interventions again and those who had LapGJ received stent placements on the anastomosis site. There were 19 cases of repeated stent placements in DS group and none in LapGJ group. The most common type of obstruction was tumor growth on the stent, either ingrowth or outgrowth leading to stent compression. Two cases showed stent migration, into the duodenum or jejunum. Malfunction of the stent itself presented in 5 cases in DS group. GJ site obstruction occurred in 2 patients and both underwent stent placements. A total of 17 patients underwent reintervention more than 2 times; 6 patients needed 3 stent placements and 1 patient underwent 4 placements. The mean time to reintervention was 116 days in DS group and 426 days in LapGJ group. Since there were only 2 cases of reinterventions in LapGJ group, statistical comparison was meaningless.
The effects of LapGJ and DS on postoperative chemotherapy were analyzed (Table 5). A significant difference was observed in chemotherapy tolerance duration. LapGJ group endured the same chemotherapy regimen longer than DS group (243 days vs. 74 days, P = 0.006). Also, LapGJ patients could maintain chemotherapy longer after surgery than DS patients (247 days vs. 137 days, P = 0.04).
Among the 101 patients, 43 patients from each group were chosen after propensity score matching (Table 6). All patients were evaluated for survival confirmation on September 2016 which allowed us at least 1 year to follow up on the last patients. The median survival of the LapGJ and DS group were 220 days and 114 days, respectively, which showed significant difference with Kaplan Meier log rank analysis (P = 0.004) (Fig. 1).
Malignant GOO occurs in up to 20% of the patients with local extension of pancreas, stomach, or duodenal cancer [13]. For decades, the only option available for palliation was via open GJ [14]. Unfortunately, many patients are not fit enough to survive surgical palliative bypass operations. Endoscopic stenting is associated with lower morbidity and mortality, as well as providing the advantage of being performed in an outpatient setting [15], whereas GJ is not so effective in this setting because of impaired gastric motility and the risk of tumor bleeding [3]. Treatment of GOO is indicated because of poor clinical conditions caused by vomiting, dehydration, and malnutrition, which develop quickly in these patients [5]. The aim of palliation is to maintain oral intake, allow sustained chemotherapy, and to improve the quality of life [16].
Whereas there are many studies that compared DS with open GJ, very few studies have compared DS with LapGJ. This study may be the largest study comparing DS with LapGJ only. Previous studies have demonstrated the effectiveness of LapGJ in comparison to open GJ and it has been adopted as the procedure of choice at many institutions [911]. Some studies have suggested that LapGJ is less invasive and is therefore associated with a shorter hospital stay than open GJ [711]. LapGJ is also said to be associated with less blood loss, lower morbidity, and less use of opiate analgesia compared to open GJ [17].
The primary aim of DS and LapGJ is to be able to resume oral intake as soon as possible. Therefore, the short-term outcomes are just as important as the long-term outcomes. Short-term results differed from study to study but all showed DS group to have shorter time to first diet, 5 to 7 days after DS and eight days after GJ [51618]. In our study, patients in DS group resumed diet in 1.9 days, whereas it took 3.2 days for those who underwent LapGJ. Our results seem to have superior outcomes compared to previous studies. These studies defined restoration of oral intake as having GOOSS score of above 2 (soft solids). However, our hospital's semifluid diet stands between GOOSS score 1 and 2, so in terms of our definition of return of oral intake, it may have been faster than in other studies. Another short-term outcome is postoperative complication during admission. GJ itself is associated with significant morbidity (13%–55%) [192021]. In our study, postoperative complication during admission in LapGJ group occurred in 7 patients (16%), which was within a similar range. DS did not show in admission complications but showed delayed complications that led to reintervention.
There are several parameters determining the nutritional status of patients. The Nutritional Risk Index, developed by the Veteran's Affairs Total Parenteral Nutrition group in 1991 for use in the evaluation of the efficacy of perioperative total parenteral nutrition in patients undergoing thoracic or abdominal surgery, was used for the parameters of serum albumin and recent body weight loss [22]. In our study, we also used serum albumin and body weight to determine the change in nutritional status before the procedure and 1 month after the procedure. When body weight did not show significant difference between the 2 groups, patients in DS group showed significant decrease in the serum albumin values (-0.15 mg/dL vs. +0.75 mg/dL, P = 0.002). This might suggest that although DS patients resumed oral intake earlier than LapGJ patients (1.9 days vs. 3.2 days), diet was not maintained long enough. This is consistent with the results of change in oral intake after DS and LapGJ. After one month postprocedure, only 28% of the patients could tolerate full diet where as 74% could after LapGJ. The SUSTENT study also demonstrated that after 30 days, patients who underwent DS showed decreased oral intake. After 2 months, patients who had GJ showed significantly better oral intake (P = 0.050) [16].
After each procedure, how well the gastric-outlet is kept patent is important. Jeurnink et al. demonstrated that reinterventions were performed in 41% of their cases, whereas other studies including ours (29% and 5% in DS and LapGJ, respectively) have reported lower rates [23242526]. The duration, however, from the initial procedure to reintervention did not show a significant difference between DS and LapGJ group (116 days vs. 426 days, P = 0.424). There were only 2 patients in the LapGJ group who underwent reintervention so it was not appropriate to compare the duration to reintervention. Adler et al. [5] showed that the mean time to reintervention in patients with obstruction after initial stent insertion was 98.6 days, which is not so different from our results. Known causes of obstruction of stents were tumor overgrowth, tumor ingrowth, stent migration, extrinsic compression, and stent angulation [5]. Our study showed the same problems, which needed reintervention and in some cases more than once (25 cases).
Recently, chemotherapy has become important for unresectable or marginally resectable cancer because it can prolong overall survival and provide better quality of life. Few studies have demonstrated that chemotherapy is associated with longer duration of oral intake and increase in reintervention-free periods [2728]. Whereas these studies focus on chemotherapy's effect on the symptoms, our study emphasized the effect of LapGJ and DS on chemotherapy compliance. LapGJ allowed for patients to receive more effective chemotherapy without dose reduction and to maintain longer chemotherapy than DS. Therefore, we suggest a 2-step approach for those patients who show suspicious resectability. First, if the tumor is proven unresectable under diagnostic laparoscopic examination, only LapGJ should be done. If the patient can tolerate aggressive chemotherapy and the tumor extent decreases, a second-look operation should be planned. Second, if the tumor becomes resectable after chemotherapy, radical surgery would then be helpful in the long term.
Survival showed significant difference in the 2 groups. Patients were matched with age, sex, T-stage, comorbidities, and chemotherapy status by the propensity scoring method to reduce selection bias. Although the last few patients were followed up only a year for survival analysis, a similar number of patients were distributed evenly at each procedure grouping, and most of them were dead at the time of follow-up. Patients who underwent LapGJ tended to live longer (114 days vs. 220 days, P = 0.004). Median survival rates in other studies also ranged from 7 to 141 days after DS and 70 to 249 days after GJ including LapGJ [17252930].
In nonrandomized retrospective studies, patient selection bias is likely to be significant. It is likely for surgeons and other doctors to suggest advanced and malnutritioned patients who are not fit for general anesthesia to receive DS. However, the paradox lies in that more advanced patients with fully obstructed outlet can only receive GJ and less advanced patients with only stenosis can undergo DS. Due to this nature, we had to take extra precautions and applied the propensity scoring method for oral intake and survival analysis.
There were significant limitations present in this study. First, preprocedural functional status such as Eastern Cooperative Oncology Group and Karnofsky score were not analyzed. Functional capacity before the procedures would have influenced the decision on whether to undergo DS or LapGJ from the beginning. However, the evaluation of functional capacity is difficult in a retrospective study. We therefore analyzed the facts shown in Table 1 about each patient in order to evaluate the status of the patient. Second, the cost of each procedure was not analyzed. Many studies comparing DS and GJ focus on costs, but due to the difference in cost of stents and cost of surgery in Korea, it seemed unnecessary to compare them. Third, there were very few studies that compared DS with LapGJ. Therefore, some comparison with other studies had to be done with open GJ.
Our results suggest that even though DS provides faster return of oral intake, LapGJ patients showed better survival and undiminished oral intake. This in turn suggests that LapGJ patients can sustain better chemotherapy than DS patients having far fewer additional interventions due to obstruction. Therefore, LapGJ would be the first choice in GOO patients with unresectable gastric cancer who can withstand general anesthesia and can endure the postoperative burden.
Figures and Tables
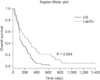 | Fig. 1A Kaplan-Meier log rank analysis of overall survival. DS, duodenal stenting; LapGJ, laproscopic gastrojejunostomy. |
Table 2
Oral intake

Values are presented as number of patients (%).
DS, duodenal stenting; LapGJ, laproscopic gastrojejunostomy.
a)GOOSS, Gastric Outlet Obstruction Scoring System (0, no intake; 1, liquids; 2, soft solids; 3, full diet). b)Patients matched with age, sex, T-stage, chemotherapy, and comorbidity by propensity scoring method.
References
1. Del Piano M, Ballarè M, Montino F, Todesco A, Orsello M, Magnani C, et al. Endoscopy or surgery for malignant GI outlet obstruction? Gastrointest Endosc. 2005; 61:421–426.
2. Arciero CA, Joseph N, Watson JC, Hoffman JP. Partial stomach-partitioning gastrojejunostomy for malignant duodenal obstruction. Am J Surg. 2006; 191:428–432.
3. Kubota K, Kuroda J, Origuchi N, Kaminishi M, Isayama H, Kawabe T, et al. Stomach-partitioning gastrojejunostomy for gastroduodenal outlet obstruction. Arch Surg. 2007; 142:607–611.
4. Lillemoe KD, Pitt HA. Palliation. Surgical and otherwise. Cancer. 1996; 78:3 Suppl. 605–614.
5. Adler DG, Baron TH. Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: experience in 36 patients. Am J Gastroenterol. 2002; 97:72–78.
6. Fiori E, Lamazza A, Volpino P, Burza A, Paparelli C, Cavallaro G, et al. Palliative management of malignant antro-pyloric strictures. Gastroenterostomy vs. endoscopic stenting. A randomized prospective trial. Anticancer Res. 2004; 24:269–271.
7. Mittal A, Windsor J, Woodfield J, Casey P, Lane M. Matched study of three methods for palliation of malignant pyloroduodenal obstruction. Br J Surg. 2004; 91:205–209.
8. Dormann A, Meisner S, Verin N, Wenk Lang A. Self-expanding metal stents for gastroduodenal malignancies: systematic review of their clinical effectiveness. Endoscopy. 2004; 36:543–550.
9. Alam TA, Baines M, Parker MC. The management of gastric outlet obstruction secondary to inoperable cancer. Surg Endosc. 2003; 17:320–323.
10. Siddiqui A, Spechler SJ, Huerta S. Surgical bypass versus endoscopic stenting for malignant gastroduodenal obstruction: a decision analysis. Dig Dis Sci. 2007; 52:276–281.
11. Choi YB. Laparoscopic gatrojejunostomy for palliation of gastric outlet obstruction in unresectable gastric cancer. Surg Endosc. 2002; 16:1620–1626.
12. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.
13. Kulke MH. Metastatic pancreatic cancer. Curr Treat Options Oncol. 2002; 3:449–457.
14. Di Fronzo LA, Cymerman J, Egrari S, O'Connell TX. Unresectable pancreatic carcinoma: correlating length of survival with choice of palliative bypass. Am Surg. 1999; 65:955–958.
15. Yim HB, Jacobson BC, Saltzman JR, Johannes RS, Bounds BC, Lee JH, et al. Clinical outcome of the use of enteral stents for palliation of patients with malignant upper GI obstruction. Gastrointest Endosc. 2001; 53:329–332.
16. Jeurnink SM, Steyerberg EW, van Hooft JE, van Eijck CH, Schwartz MP, Vleggaar FP, et al. Surgical gastrojejunostomy or endoscopic stent placement for the palliation of malignant gastric outlet obstruction (SUSTENT study): a multicenter randomized trial. Gastrointest Endosc. 2010; 71:490–499.
17. Al-Rashedy M, Dadibhai M, Shareif A, Khandelwal MI, Ballester P, Abid G, et al. Laparoscopic gastric bypass for gastric outlet obstruction is associated with smoother, faster recovery and shorter hospital stay compared with open surgery. J Hepatobiliary Pancreat Surg. 2005; 12:474–478.
18. Mauro MA, Koehler RE, Baron TH. Advances in gastrointestinal intervention: the treatment of gastroduodenal and colorectal obstructions with metallic stents. Radiology. 2000; 215:659–669.
19. Holt AP, Patel M, Ahmed MM. Palliation of patients with malignant gastroduodenal obstruction with self-expanding metallic stents: the treatment of choice? Gastrointest Endosc. 2004; 60:1010–1017.
20. Lopera JE, Brazzini A, Gonzales A, Castaneda-Zuniga WR. Gastroduodenal stent placement: current status. Radiographics. 2004; 24:1561–1573.
21. Maetani I, Tada T, Ukita T, Inoue H, Sakai Y, Nagao J. Comparison of duodenal stent placement with surgical gastrojejunostomy for palliation in patients with duodenal obstructions caused by pancreaticobiliary malignancies. Endoscopy. 2004; 36:73–78.
22. Veterans Affairs Total Parenteral Nutrition Cooperative Study Group. Perioperative total parenteral nutrition in surgical patients. N Engl J Med. 1991; 325:525–532.
23. Jeurnink SM, Steyerberg EW, Hof Gv, van Eijck CH, Kuipers EJ, Siersema PD. Gastrojejunostomy versus stent placement in patients with malignant gastric outlet obstruction: a comparison in 95 patients. J Surg Oncol. 2007; 96:389–396.
24. Nevitt AW, Vida F, Kozarek RA, Traverso LW, Raltz SL. Expandable metallic prostheses for malignant obstructions of gastric outlet and proximal small bowel. Gastrointest Endosc. 1998; 47:271–276.
25. Razzaq R, Laasch HU, England R, Marriott A, Martin D. Expandable metal stents for the palliation of malignant gastroduodenal obstruction. Cardiovasc Intervent Radiol. 2001; 24:313–318.
26. Soetikno RM, Lichtenstein DR, Vandervoort J, Wong RC, Roston AD, Slivka A, et al. Palliation of malignant gastric outlet obstruction using an endoscopically placed Wallstent. Gastrointest Endosc. 1998; 47:267–270.
27. Telford JJ, Carr-Locke DL, Baron TH, Tringali A, Parsons WG, Gabbrielli A, et al. Palliation of patients with malignant gastric outlet obstruction with the enteral Wallstent: outcomes from a multicenter study. Gastrointest Endosc. 2004; 60:916–920.
28. Khashab M, Alawad AS, Shin EJ, Kim K, Bourdel N, Singh VK, et al. Enteral stenting versus gastrojejunostomy for palliation of malignant gastric outlet obstruction. Surg Endosc. 2013; 27:2068–2075.
29. Espinel J, Vivas S, Muñoz F, Jorquera F, Olcoz JL. Palliative treatment of malignant obstruction of gastric outlet using an endoscopically placed enteral Wallstent. Dig Dis Sci. 2001; 46:2322–2324.
30. Johnsson E, Thune A, Liedman B. Palliation of malignant gastroduodenal obstruction with open surgical bypass or endoscopic stenting: clinical outcome and health economic evaluation. World J Surg. 2004; 28:812–817.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download