Abstract
Purpose
To demonstrate the feasibility, safety, and technical strategies of hand-assisted laparoscopic complete mesocolic excision (HAL-CME) and to compare oncological outcomes between HAL-CME and the open approach (O-CME) for right colon cancers.
Methods
Patients who were scheduled to undergo a right hemicolectomy were divided into HAL-CME and O-CME groups. Measured outcomes included demographic variables, perioperative parameters, and follow-up data. Demographic variables included age, sex distribution, body mass index (BMI), American Society of Anesthesiologists (ASA) physical status classification, previous abdominal surgery, tumor localization, and potential comorbidities. Perioperative parameters included incision length, operative time, blood loss, conversion rate, postoperative pain score, postoperative first passage of flatus, duration of hospital stay, total cost, number of lymph nodes retrieved, TNM classification, and postoperative complications. Follow-up data included follow-up time, use of chemotherapy, local recurrence rate, distant metastasis rate, and short-term survival rate.
Results
In total, 150 patients (HAL-CME, 78; O-CME, 72) were included. The groups were similar in age, sex distribution, BMI, ASA classification, history of previous abdominal surgeries, tumor localization, and potential comorbidities. Patients in the HAL-CME group had shorter incision lengths, longer operative times, less operative blood loss, lower pain scores, earlier first passage of flatus, shorter hospital stay, higher total costs, similar numbers of lymph nodes retrieved, similar TNM classifications, and a comparable incidence of postoperative complications. The 2 groups were also similar in local recurrence rate, distant metastasis rate, and short-term survival rate.
Total mesorectal excision (TME) is now considered the ‘standard’ surgical approach for rectal cancers, which requires appropriate surgical technique and leads to an improved recurrence rate and 5-year survival [12]. It is based on the principle that dissection in the mesorectal plane produces an intact fascial-lined specimen containing all of the blood vessels, lymphatic vessels, and lymph nodes, where possible metastasis was present [3]. Recently, likewise with the concept of TME, the term “complete mesocolic excision” (CME) has been introduced in colon cancer [45]. It is defined as a sharp dissection of the visceral fascia layer from the parietal layer, resulting in complete mobilization of the mesocolon, covered by an intact visceral fascia layer, and tying of the roots of the supplying arteries [6]. Some researchers have proposed that CME using central vascular ligation (CVL) should be a standard approach for colon cancer surgery, reducing local recurrence and improving long-term survival compared with previous procedures [34]. Presently, however, CME is still a novel concept, and more clinical data regarding CME are needed to support wider acceptance of this approach worldwide.
Since its first introduction in 1991, laparoscopic colorectal surgery for colorectal cancer has increased rapidly, based on its particular benefits, including minimal trauma, decreased postoperative pain, earlier ambulation, faster recovery, and shortened hospital stay [2678]. Additionally, the oncological outcomes of laparoscopic colorectal surgery for colorectal cancer are comparable with those of an open colectomy [19]. However, some shortcomings have also been addressed, including prolonged operative time, steep learning curve, and lack of tactile feedback [1011]. Thus, despite reports that laparoscopy yields ‘better’ clinical outcomes, its utilization is estimated to be only 20%–30% in Western countries [1213]. The use of hand-assisted laparoscopic surgery (HALS), a relatively new, minimally invasive surgical technique, began in the mid 1990s; it can be considered as an effective alternative to total laparoscopic procedures [14]. In HALS, the nondominant hand of the surgeon is inserted into the abdomen through a special hand port; then, with the help of laparoscopic visualization, that hand can assist with exposure, retraction, dissection, and hemostasis during the operation [11]. Due to the combined advantages of both laparoscopic and conventional laparotomies, many studies have demonstrated the feasibility of HALS in various laparoscopic procedures, such as hepatectomy, splenectomy, gastrectomy, and nephrectomy [151617]. Regarding colectomy, a few studies have demonstrated that hand-assisted laparoscopic colectomy can be a safe and minimally invasive approach and a potentially more appropriate operation than a laparoscopic or an open colectomy [1114].
Regarding laparoscopic CME in colectomy, an increasing number of studies have evaluated the technique, reporting encouraging outcomes [161819]. However, to our knowledge, there is no study in the literature that has compared shortterm outcomes between hand-assisted laparoscopic CME (HALCME) and a conventional open approach (O-CME). The aim of this retrospective study was to assess the feasibility, safety, and technical strategies of HAL-CME and to compare the oncological outcomes between HAL-CME and O-CME for right hemicolon cancers.
All patients admitted to The First Affiliated Hospital of College of Medicine, Zhejiang University to undergo a right hemicolectomy between May 2012 and April 2014 were enrolled. The study criteria included cecal, ascending colon, or hepatic flexure cancer, confirmed by a pathological examination, no distant metastasis or extracolonic invasion (en bloc resection of adjacent tissues must be performed), and patients with ASA classification I–III and ability to tolerate the operation. The exclusion criteria included colon cancer with distant metastasis or extracolonic invasion, ‘huge’ tumors (diameter, >7 cm), malignant lymphoma or other noncancer cases, and emergency operation cases (bowel obstruction or intestinal perforation). All enrolled patients were divided into the hand-assisted laparoscopic CME group (HAL-CME group) and the conventional open approach group (O-CME), according to the patient's own preferences after a detailed discussion with the surgeon and the availability of the necessary laparoscopic instruments. All patients and their families provided written informed consent.
Preoperative chest CT and abdominal enhanced CT were routinely performed to exclude pulmonary and hepatic metastasis. The abdominal CT was also used to assess size and location of the tumor, identify extracolonic invasion, and evaluate its resectability. Preoperative colonoscopy and biopsy were necessary for the diagnosis of patients. Patients were put on a liquid diet the day before the operation and underwent preoperative mechanical bowel preparation the night before surgery [11].
In this group, the patient was placed in a modified low lithotomy position at a 15° tilt to the left side. A 6.0-cm midline incision of 3-finger breadth around the umbilicus was made first for the placement of the hand-port (Lap-Disc; Ethicon Endo-Surgery, Somerville, NJ, USA), which enables nondominant hand exchanges into each quadrant of the abdomen without gas leakage. After establishment of pneumoperitoneum, a 10-mm trocar for the harmonic scalpel was created in the anti-McBurney point of the left lower quadrant, and another 10-mm trocar for a 30° telescope was inserted in the left midclavicular line at the level of the umbilicus. The chief surgeon stood between the patient's legs, using his left (nondominant) hand for the operation, while the assistant stood to the left of the patient to control the telescope.
A routine exploration of the abdominopelvic cavity was made first, and then a medial-to-lateral dissection was performed. The dissection started along the superior mesenteric vein (SMV) after identifying the pedicle of ileocolic vessels. The ileocolic vessels were exposed completely and transected at the root. Next, the dissection was extended caudally to the peritoneal reflection of the terminal ileum, laterally under the right paracolic peritoneal reflection, and superiorly above the pancreas and duodenum to the fused fasciae of the lesser epiploic sac. As a result, an avascular surgical plane composed of Toldt's and prerenal fascia was exposed. Then, the dissection was continued upwards to the right colic vessels (if present) and the gastrocolic trunk. The colic branch of the gastrocolic trunk was transected, and the pancreatic and gastric branches were preserved. Next, the middle colic vessels were identified and severed at the root of the right branch (for tumors located in the cecum and ascending colon) or at the origin from the superior mesenteric vessels (for tumors located in the proximal transverse colon and hepatic flexure). Division of the greater omentum resected en bloc with the right colon and exposure of the lesser sac were performed. Then, dissection of the subpyloric lymph nodes was performed after ligation at the origin of the right omentum veins (for tumors located in the proximal transverse colon and hepatic flexure). The fusion fascia was detached between the omentum and transverse mesocolon until the point below the lower edge of the pancreas, uncovering the SMV. Finally, the dissection was completed at the right part of the gastrocolic ligament, the peritoneum of the right paracolic sulci, and at the peritoneal reflection of the terminal ileum. Subsequently, the mobilized right hemicolon was brought out through the hand-port. Extracorporeal ileotransverse side-to-side anastomosis was then performed, and the mesenteric defect was closed. Finally, a suction drain was inserted into the pelvis, and the abdominal wall wounds were closed, layer-by-layer.
In this group, the patient was also placed in a supine position, and the operation was performed in a standard manner including CME and CVL. A midline incision approximately 15–20 cm was made, and a medial-to-lateral dissection was performed subsequently. The dissection was started along the superior mesenteric vessels, below the third portion of the duodenum. Corresponding vessels including the ileocolic vessels, right colic vessels (if present), colic branch of the gastrocolic trunk and middle colic vessels were transected at the root. Dissection of the lymph nodes and lymphatic tissues at the origin of these vessels was also performed. After the right hemicolon was mobilized completely and the mesenteric division had been made, an ileotransverse side-to-side anastomosis was performed. Then, a suction drainage tube was inserted into the right paracolic sulci and the abdominal wall wounds were closed, layer-by-layer.
The 2 groups were compared in terms of demographics variables, perioperative parameters, and follow-up data. Demographics variables included age, gender distribution, body mass index (BMI), ASA classification, previous abdominal surgeries, tumor localization, and potential comorbidities. Perioperative parameters included incision length, operative time, blood loss, conversion rate, postoperative pain score, postoperative first passage of flatus, duration of hospital stay, total cost, number of lymph nodes retrieved, TNM classification, and postoperative complications. Follow-up data included follow-up time, use of chemotherapy, local recurrence rate, distant metastasis rate, and short-term survival rate. All patients were followed up by the surgical clinic or by a telephone interview, and data in the medical records were checked.
The SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used. Continuous variables were expressed as means ± standard deviations, and discrete variables were expressed as numbers and percentages. Statistical analysis was performed using independent-samples t-tests or chi-square test where appropriate. For all analyses, a P-value < 0.05 was considered to indicate statistical significance.
In total, 150 patients with right hemicolon cancer meeting the inclusion criteria were assessed (HAL-CME, 78; O-CME, 72). All operations in both groups were performed by the same surgical team. There was no conversion to O-CME for any patient undergoing the HAL-CME procedure in this study.
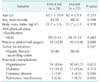
The demographic variables of the 2 groups are listed in Table 1. The 2 groups were similar in age, sex distribution, BMI, ASA classification, previous abdominal surgical history, tumor localization, and potential comorbidities (all P > 0.05). The perioperative parameters of both groups are presented in Table 2. As for surgical parameters, patients in the HALCME group had a shorter incision length (5.8 ± 0.5 cm vs. 16.3 ± 4.9 cm, P < 0.05), longer operative time (156 ± 20 minutes vs. 130 ± 15 minutes, P < 0.05), and less operative blood loss (120 ± 56 mL vs. 127 ± 56 mL, P < 0.05) than those of the patients in the O-CME group. After the operation, patients in the HAL-CME group had a lower pain score (3.0 ± 0.7 vs. 5.1 ± 0.6, P < 0.05), earlier first passage of flatus (50.9 ± 2.3 hours vs. 77.6 ± 2.3 hours, P < 0.05), shorter hospital stay (7.2 ± 1.1 days vs. 9.6 ± 1.9 days, P < 0.05), higher total costs (34,660 ± 1,458 renminbi [RMB] vs. 30,721 ± 2,135 RMB, P < 0.05), similar number of lymph nodes retrieved (19.2 ± 2.8 vs. 19.9 ± 2.5, P > 0.05), similar TNM classification (P > 0.05), and a comparable incidence of postoperative complications (P > 0.05) compared with the O-CME group. Postoperative follow-up data are presented in Table 3. The median follow-up period for the 2 groups was 20.1 ± 4.6 months. During follow-up, the use of postoperative adjuvant chemotherapy (Xelox or mFolfox6) was similar between the groups (P > 0.05). The 2 groups of patients were also similar in terms of local recurrence rate (1.3% vs. 1.4%), distant metastasis rate (1.3% vs. 1.4%), and short-term survival rate (79.5% vs. 77.8%) (all P > 0.05).
There is global consensus that TME, derived from an embryological concept, is the ‘standard’ for rectal cancer surgery; the procedure focuses on achieving intact block resection of the mesorectum, tumor, and lymphatic drainage [1820]. Like the mesorectum, the embryonic anatomical theory states that both visceral and parietal planes also cover a mesocolonlike envelope. Hohenberger et al. [4], who recently brought the concept of the mesocolonic envelope to colon cancer surgery, proposed that laparotomic CME is superior to ‘traditional’ colon cancer surgery in terms of 5-year local recurrence rate and 5-year cancer-related survival. Compared with traditional radical surgery for right colon, technical strategies for CME include two aspects: sharp separation of visceral and parietal fascia, based on embryonic anatomy, to minimize the likelihood of an incomplete resection, and ligation at the root of central supply vessels and more radical lymph node dissection for improving oncological outcomes [1418]. Although the right hemicolectomy is performed routinely worldwide today, the feasibility and safety of CME has only recently been demonstrated in open surgeries and in select centers [5721]. In the present study, we compared short-term outcomes between HAL-CME and O-CME groups and demonstrated the feasibility, safety, and technical strategies of HAL-CME. Patients in the HAL-CME group experienced a shorter incision length, less operative blood loss, lower pain scores, earlier first passage of flatus, and shorter hospital stay than those of patients in the O-CME group. Finally, short-term oncological outcomes were comparable and generally good with both approaches for treating right hemicolon cancer.
Laparoscopic colectomy has become a standard surgical treatment for colon cancer; short-term benefits, such as decreased postoperative pain, more rapid postoperative recovery, shortened hospital stay, improved quality of life, and similar oncological results compared with open colectomy have been demonstrated [162022]. With the emergence of CME, laparoscopic CME in colectomy has been reported increasingly and has achieved encouraging outcomes. However, some deficiencies have been raised regarding the lack of tactile feedback, the prolonged operative time, the steep learning curve, the cost-effectiveness of laparoscopic techniques, and the potential for port-site tumor recurrence [11]. Moreover, a laparoscopic CME is not easy to perform because of the complex and variable vascular anatomy of the right hemicolon [621]. Many studies have shown that HALS is a valid surgical approach for colorectal resection that offers similar short- and long-term MIS benefits, compared with laparoscopic procedures, while being less technically demanding, have a shorter learning curve for less experienced surgeons, and a low conversion rate to open approaches [10111423]. However, no reported study has evaluated the feasibility, safety, or technical strategies for HAL-CME. In our study, we demonstrated that this technique is a safe, useful, and feasible method for patients with right hemicolon cancer. The HAL-CME procedure is associated with a smaller incision, less operative blood loss, less postoperative pain, earlier postoperative passage of flatus, shorter hospital stay, and similar short-term oncological outcomes compared with O-CME.
The operative approach of CME includes lateral or medial access. According to the literature, lateral access or medial access is used to conduct CME procedures [2425]. For right hemicolectomies, lateral access is usually performed in most open surgeries, whereas medial access is used in most laparoscopic approaches. Lateral access begins with complete mobilization of the total right hemicolon, followed by a sharp separation between the visceral and parietal fascia. Then, a high ligation at the root of the central supply vessels to the right hemicolon is performed. Medial access begins with ligation of the ileocolic vessels and proceeds along the superior mesenteric vessel in the mesocolon to enter the genuine surgical plain between the visceral and parietal fascia. After high ligation at the root of the central supply vessels to the right hemicolon, complete mobilization of the total right hemicolon is performed.
Although there is no consensus or large-scale comparative studies on the proper dissection plane in a laparoscopic colectomy, some authors have advocated medial access [2627], while others have suggested lateral access [6]. We consider that medial access involves decreased manipulation of the cancer, earlier detection of retroperitoneal structures, and reduced bleeding from prior division of vessels.
The impact of the number of lymph nodes retrieved after colon cancer surgery on oncological outcomes has recently been emphasized. Retrieving an adequate number of lymph nodes is crucial for accurate tumor staging in the management of colorectal cancer. Some studies have suggested that the number of lymph nodes harvested and the ratio of involved to uninvolved nodes appear to be significant prognostic factors even in patients with stage III disease, in which improved survival is seen with increased lymph node yield [62829], with the optimum number of nodes ranging between 15 and 28 [430]. It has been demonstrated that CME and CVL remove more tissue around a tumor and are more likely to resect in the mesocolic plane, resulting in a maximal lymph node harvest [3]. In the present study, the numbers of lymph nodes retrieved in the 2 groups were 19.2 ± 2.8 (HAL-CME) and 19.9 ± 2.5 (O-CME), more than that in our previous study [11]. Moreover, with regard to oncological outcomes, the 2 groups showed very low local recurrence (1.3% and 1.4%) and distant metastasis rates (1.3% and 1.4%). The short-term overall survival rate was 78.7%.
In conclusion, we performed a retrospective study demonstrating the feasibility, safety, and technical strategies of HALCME and compared the oncological outcomes between HALCME and O-CME for right hemicolon cancers. The results from the present study demonstrate that the HAL-CME procedure is a safe, valid, and feasible surgical method for right hemicolon cancers. It is associated with smaller incisions, less operative blood loss, less postoperative pain, earlier recovery after operation, and shorter hospital stays compared with O-CME. However, to address the role of HAL-CME in the curative management of right hemicolon cancers, longer-term follow-up is needed.
Figures and Tables
ACKNOWLEDGEMENTS
The study was supported by the Natural Science Foundation of Zhejiang Province (No. LY13H030004).
References
1. Adamina M, Manwaring ML, Park KJ, Delaney CP. Laparoscopic complete mesocolic excision for right colon cancer. Surg Endosc. 2012; 26:2976–2980.
2. Zheng MH, Feng B, Hu CY, Lu AG, Wang ML, Li JW, et al. Long-term outcome of laparoscopic total mesorectal excision for middle and low rectal cancer. Minim Invasive Ther Allied Technol. 2010; 19:329–339.
3. West NP, Hohenberger W, Weber K, Perrakis A, Finan PJ, Quirke P. Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol. 2010; 28:272–278.
4. Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation: technical notes and outcome. Colorectal Dis. 2009; 11:354–364.
5. Gouvas N, Pechlivanides G, Zervakis N, Kafousi M, Xynos E. Complete mesocolic excision in colon cancer surgery: a comparison between open and laparoscopic approach. Colorectal Dis. 2012; 14:1357–1364.
6. Kang J, Kim IK, Kang SI, Sohn SK, Lee KY. Laparoscopic right hemicolectomy with complete mesocolic excision. Surg Endosc. 2014; 28:2747–2751.
7. Li JC, Leung KL, Ng SS, Liu SY, Lee JF, Hon SS. Laparoscopic-assisted versus open resection of right-sided colonic cancer: a prospective randomized controlled trial. Int J Colorectal Dis. 2012; 27:95–102.
8. Lim SW, Kim HR, Kim YJ. Single incision laparoscopic colectomy for colorectal cancer: comparison with conventional laparoscopic colectomy. Ann Surg Treat Res. 2014; 87:131–138.
9. Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg. 2010; 97:1638–1645.
10. Aalbers AG, Biere SS, van Berge Henegouwen MI, Bemelman WA. Hand-assisted or laparoscopic-assisted approach in colorectal surgery: a systematic review and meta-analysis. Surg Endosc. 2008; 22:1769–1780.
11. Sheng QS, Lin JJ, Chen WB, Liu FL, Xu XM, Lin CZ, et al. Hand-assisted laparoscopic versus open right hemicolectomy: short-term outcomes in a single institution from China. Surg Laparosc Endosc Percutan Tech. 2012; 22:267–271.
12. Alnasser M, Schneider EB, Gearhart SL, Wick EC, Fang SH, Haider AH, et al. National disparities in laparoscopic colorectal procedures for colon cancer. Surg Endosc. 2014; 28:49–57.
13. Rea JD, Cone MM, Diggs BS, Deveney KE, Lu KC, Herzig DO. Utilization of laparoscopic colectomy in the United States before and after the clinical outcomes of surgical therapy study group trial. Ann Surg. 2011; 254:281–288.
14. Meshikhes AW. Controversy of hand-assisted laparoscopic colorectal surgery. World J Gastroenterol. 2010; 16:5662–5668.
15. Dai LH, Xu B, Zhu GH. Hand-assisted laparoscopic surgery of abdominal large visceral organs. World J Gastroenterol. 2006; 12:4736–4740.
16. Wong SK, Tsui DK, Li MK. Laparoscopic distal gastrectomy for gastric cancer: initial experience on hand-assisted technique and totally laparoscopic technique. Surg Laparosc Endosc Percutan Tech. 2009; 19:298–304.
17. Moore NW, Nakada SY, Hedican SP, Moon TD. Complications of hand-assisted laparoscopic renal surgery: single-center tenyear experience. Urology. 2011; 77:1353–1358.
18. Feng B, Sun J, Ling TL, Lu AG, Wang ML, Chen XY, et al. Laparoscopic complete mesocolic excision (CME) with medial access for right-hemi colon cancer: feasibility and technical strategies. Surg Endosc. 2012; 26:3669–3675.
19. Chow CF, Kim SH. Laparoscopic complete mesocolic excision: West meets East. World J Gastroenterol. 2014; 20:14301–14307.
20. Mori S, Baba K, Yanagi M, Kita Y, Yanagita S, Uchikado Y, et al. Laparoscopic complete mesocolic excision with radical lymph node dissection along the surgical trunk for right colon cancer. Surg Endosc. 2015; 29:34–40.
21. Bae SU, Saklani AP, Lim DR, Kim DW, Hur H, Min BS, et al. Laparoscopic-assisted versus open complete mesocolic excision and central vascular ligation for right-sided colon cancer. Ann Surg Oncol. 2014; 21:2288–2294.
22. Baek JH, Lee GJ, Lee WS. Comparison of long-term oncologic outcomes of stage III colorectal cancer following laparoscopic versus open surgery. Ann Surg Treat Res. 2015; 88:8–14.
23. Sheng QS, Lin JJ, Chen WB, Liu FL, Xu XM, Hua HJ, et al. Comparison of hand-assisted laparoscopy with open total colectomy for slow transit constipation: a retrospective study. J Dig Dis. 2014; 15:419–424.
24. Ding J, Liao GQ, Xia Y, Zhang ZM, Pan Y, Liu S, et al. Medial versus lateral approach in laparoscopic colorectal resection: a systematic review and meta-analysis. World J Surg. 2013; 37:863–872.
25. Rotholtz NA, Bun ME, Tessio M, Lencinas SM, Laporte M, Aued ML, et al. Laparoscopic colectomy: medial versus lateral approach. Surg Laparosc Endosc Percutan Tech. 2009; 19:43–47.
26. Hasegawa S, Kawamura J, Nagayama S, Nomura A, Kondo K, Sakai Y. Medially approached radical lymph node dissection along the surgical trunk for advanced right-sided colon cancers. Surg Endosc. 2007; 21:1657.
27. Pigazzi A, Hellan M, Ewing DR, Paz BI, Ballantyne GH. Laparoscopic medial-to-lateral colon dissection: how and why. J Gastrointest Surg. 2007; 11:778–782.
28. Schumacher P, Dineen S, Barnett C Jr, Fleming J, Anthony T. The metastatic lymph node ratio predicts survival in colon cancer. Am J Surg. 2007; 194:827–831.
29. Moore J, Hyman N, Callas P, Littenberg B. Staging error does not explain the relationship between the number of lymph nodes in a colon cancer specimen and survival. Surgery. 2010; 147:358–365.
30. Vather R, Sammour T, Zargar-Shoshtari K, Metcalf P, Connolly A, Hill A. Lymph node examination as a predictor of long-term outcome in Dukes B colon cancer. Int J Colorectal Dis. 2009; 24:283–288.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download