Abstract
Purpose
Pancreaticoduodenectomy (PD) is a complex surgery associated with high morbidity, mortality, and cost. Municipal hospitals have their important role in the public health and welfare system. The purpose of this study was to identify the feasibility as well as the cost-effectiveness of performing PD in a mid-volume municipal hospital based on 13 years of experience with PD.
Methods
From March 2003 to November 2015, 183 patients underwent PD at Seoul Metropolitan Government - Seoul National University Boramae Medical Center.. Retrospectively collected data were analyzed, with a particular focus on complications. Hospital costs were analyzed and compared with a national database, with patients divided into 2 groups on the basis of medical insurance status.
Results
The percentage of medical aid was significantly higher than the average in Korean hospitals. (19.1% vs. 5.8%, P = 0.002). Complications occurred in 88 patients (44.3%). Postoperative pancreatic fistula (POPF) occurred in 113 cases (61.7%), but the clinically relevant POPF was 24.6% (grade B: 23.5% and grade C: 1.1%). The median hospital stay after surgery was 20 days (range, 6–137 days). In-hospital mortality was 3.8% (n = 7), with pulmonary complications being the leading cause. During the study period, improvements were observed in POPF rate, operation time, and hospital stay. The mean total hospital cost was 13,819 United States dollar (USD) per patient, and the mean reimbursement from the National Health Insurance Service (NHIS) to health care providers was 10,341 USD (74.8%). The patient copayment portion of the NHIS payment was 5%.
Pancreaticoduodenectomy (PD) is a complex surgery associated with high morbidity, mortality, and cost. Owing to its complexity, the tendency for this surgery to be centralized to high-volume hospitals has increased despite the high cost. In terms of hospital costs, public hospitals play an important role in the public health and welfare system in providing patients with high-cost procedures at a subsidized price. However, the functions and roles of these hospitals within the medical system have been underestimated. The purpose of this study was to assess the feasibility of performing PD in a mid-volume municipal hospital with regard to clinical outcomes and medical expense based on 13 years of experience.
Seoul Metropolitan Government - Seoul National University Boramae Medical Center is a public municipal hospital covering the southwestern area of Seoul, Korea, which is subsidized by the Seoul Metropolitan Government and is managed by Seoul University Hospital. From March 2003 to November 2015, 183 patients underwent PD in this hospital. Clinicopathological data were retrospectively collected from medical records until 2014 and then prospectively collected from January 2015. Clinical data including age, sex, underlying disease, operation data, and relevant clinical outcomes were analyzed. The status of a patient's medical insurance was defined by the policy of the Korean National Health Insurance Service (NHIS). This study was approved by the Institutional Review Board of Seoul Metropolitan Government - Seoul National University Boramae Medical Center (IRB No. 16-2015-176).
We followed the definition of Kim et al. [1], who graded “hospital volume” according to the number of annual PD cases: very low (<10), low (10–18), medium (19–35), high (54–111), and very high (215).
The Clavien-Dindo classification was used for grading postoperative complications. Postoperative surgical complications were considered to have occurred in cases that were classified above grade II [2]. Postoperative pancreatic fistula (POPF) was defined and graded according to the criteria of the International Study Group of Pancreatic Fistula [3]. Only clinically relevant POPF (grade B or C) was regarded as a postoperative complication. Delayed gastric emptying (DGE) was also graded according to the definition of the International Study Group of Pancreatic Surgery [4]. Intra-abdominal fluid collection was defined as complicated fluid detected in the operative field on CT on the 7th postoperative day, regardless of the existence of POPF. In-hospital mortality was defined as patient death within a 30-day postoperative hospital stay during the index admission, regardless of its cause. For comparison of clinical outcomes, an article [1] that has analyzed nationwide PD data was used as a reference. To evaluation of long term outcome, survival analysis was performed in pancreatic head cancer.
Three surgeons performed the surgical procedures. All PD surgeries were performed in laparotomy fashion. Pylorus-preserving PD (PPPD) was preferred to conventional PD in the interest of organ preservation. Pancreaticoenteric anastomoses were performed in pancreaticojejunostomy (PJ) fashion using the duct-to-mucosa method. Although the use of pancreatic stents was left to the surgeon's discretion, external pancreatic stenting was usually performed when the pancreatic texture was soft and the diameter of the main pancreatic duct was less than 3 mm, and internal pancreatic stents were inserted when the diameter of the main pancreatic duct was greater than 5 mm and the pancreas had a hard texture. Prophylactic intravenous antibiotics were administered only on the day of surgery. Octreotide was not routinely administered. The nasogastric tube was removed on the 1st postoperative day. Small sips of water were allowed from the second postoperative day, and a blended diet was attempted after gas was passed. Amylase levels in abdominal drainage fluid were checked on the postoperative third, fifth, and seventh days. Abdominal CT was routinely performed on the seventh day after surgery to rule out arterial pseudoaneurysm and to examine fluid collections.
In cases in which arterial pseudoaneurysm was suspected or postpancreatic hemorrhage was evident, angiography in the interventional radiology suite was preferred to relaparotomy. Intra-abdominal drains were removed when no fluid collection was evident on CT scan and clinically relevant POPF had not occurred.
The social security system of South Korea is composed of 3 fields including social insurance, public assistance, and social welfare service. As a compulsory social insurance program, the Korean health insurance system covers the entire population living in the country. Therefore, if all residents pay their medical insurance premium according to their income, the finances of the health care system are secured. The NHIS is the governmental agency that deals with medical tax revenue, then comprehensively manages it for all medical insurance services. The operational system of national health insurance in South Korea is shown in Fig. 1 (http://www.nhis.or.kr). In brief, total medical costs for a certain health care service consist of (1) NHIS payment: sum of payment for healthcare services from NHIS with a certain rate of copayment by the insured; and (2) Non-NHIS payment: cost for various health care services which do not meet the criteria for NHIS payment (e.g., ultrasonography, magnetic resonance imaging, robotic surgery). These costs are unpayable by the NHIS but should be paid by the patients themselves, with prices reasonably determined by the health care providers.
Health care providers can ask for reimbursement from the NHIS for the health care services provided to the patients, for which the ratio of actual NHIS payment to copayment by the patient is determined by the patient's economic status. For the beneficiaries of national basic livelihood, in other words the patients with low economic status, the proportion of NHIS payment will be increased. Particularly in the case of the destitute poor, the charge to the patients goes to nearly zero. The Health Insurance Review and Assessment Service (HIRA) audits and reviews the bills from health care providers, then announces the review results to the NHIS and gives feedback to health care providers. In the current study, we divided the patients into 2 groups based on the proportion of the payment from the NHIS: (1) Health insurance group: the NHIS paid about 80% of all medical costs as social insurance; and (2) Medical aid (beneficiaries) group: the NHIS covered 95%–100% of all medical costs for the basic livelihood group as public assistance. In particular, since cancer patients were preferentially allowed to pay only 5% of health care service costs, they were also included in the medical aid group in this study to equally compare the costs with those of other hospitals.
The hospital costs for PD patients in the 3 previous years (from January 2013 to November 2015) were analyzed. To specifically compare the hospital costs of PD with those of other hospitals, the overall costs for the patients with pancreatic head cancer were selectively analyzed using the data extracted from the database of the NHIS (http://www.nhis.or.kr) and the open database at the website of HIRA (http://www.hira.or.kr).
Kim et al. [1] analyzed and reported Korean data regarding PD. The authors used this article as a clinical reference regarding PD in Korea.
All statistical analyses were performed with IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA). Nominal data were compared with the chi-square test and Fisher exact test and continuous data with the Kruskal-Wallis test. Kaplan-Meier survival analysis was performed to evaluation of long term outcome. P-values less than 0.05 were considered statistically significant.
Annual PD cases in the study hospital have been consistently increasing and reached an average of 14 cases annually, ranging from 4 to 25 (Fig. 2). According to this finding, the study hospital could be classified as a low- to medium-volume center by definition [1].
The median age of the patients was 67 years (range, 14–89) and the male:female ratio was 99:84 (54.1%:45.9%). The number of patients with Charlson comorbidity index scores of greater than 3 was 122 (66.7%). The proportion of patients in the health insurance group was 80.9% and the proportion in the medical aid beneficiaries group was 19.1%. Preoperative biliary drainage was performed in 137 patients (74.8%), endoscopic retrograde biliary drainage (ERBD) in 64 (35.0%), percutaneous transhepatic biliary drainage (PTBD) in 59 (32.3%), and endoscopic nasobiliary drainage (ENBD) in 14 (7.7%). PPPD accounted for 76% of all PD cases. One hundred thirty-nine cases of PJ were externally diverted through a pancreatic stent, while 34 cases were internally drained. Ten patients had no stent. Sixteen cases were diagnosed as benign disease (8.7%) while the other 167 cases were diagnosed as malignant disease (91.3%) The most common diagnosis was distal common bile duct cancer (65 cases, 35.5%).
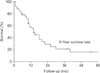
The median operation time was 350 minutes (range, 169–600 minutes). Packed red blood cells were transfused in 88 cases (48.1%). Eighty-eight patients (48.1%) experienced more than one postoperative complication. POPF occurred in 113 patients (61.7%), but clinically relevant POPF developed in only 45 patients (24.6%; grade B, 43; grade C, 2). Twenty-one patients had intra-abdominal fluid collection and 18 patients experienced DGE. Fifteen patients developed postoperative pneumonia, and the number of patients who experienced wound complications was 15. Among the nine patients who developed postoperative bleeding, 7 patients bled from arterial pseudoaneurysm, one from arterial erosive bleeding from the dorsal pancreatic artery, and the other due to unknown causes. Six out of the 7 cases of pseudoaneurysmal bleeding originated from the gastroduodenal artery stump and the remaining one originated from the proximal right hepatic artery. All of the 7 cases were embolized with coils in the interventional radiology suite and were successfully controlled, but 1 patient eventually died from pneumonia with pulmonary edema. The case of arterial erosive bleeding from the dorsal pancreatic artery was also well controlled with coil embolization, and the patient who experienced bleeding due to an unknown cause underwent relaparotomy twice, on the second and third postoperative days. However, these 2 patients eventually died due to pulmonary edema and pneumonia. In-hospital mortality was 3.8% (n = 7). Pulmonary problems were the main cause of death (n = 4), followed by sepsis (n = 1), renal failure (n = 1), and cerebral infarction (n = 1). The median length of stay in the hospital after surgery was 20 days (range, 6–137 days). The 5-year survival rate of 36 pancreatic head cancer patients was 15.0% (Fig. 3)
When the total number of cases was sequentially divided into 3 groups, 61 cases could be evenly allocated to the first (March 2003 to April 2009, 6 years), the second (May 2009 to April 2013, 4 years), and the third period (May 2013 to November 2015, 2.5 years), respectively. The overall complication rate was similar among the 3 periods (41.0% vs. 41.0% vs. 50.8%, P = 0.451) but the overall POPF rate was observed to have improved significantly (P = 0.015). The rate of clinically relevant POPF gradually decreased without statistical significance from the first period to the third (27.9% vs. 24.6% vs. 11.5%, P = 0.065). The mean operation time and the length of hospital stay were found to have diminished significantly (P = 0.007, P = 0.008, respectively).
Among the patients, 148 were partially supported by the health insurance system while the other 35 patients, accounting for 19.1% of the total patient population, were fully subsidized as medical aid beneficiaries (Fig. 4). In comparison with the reported data for South Korea [1], the proportion of medical aid beneficiaries in the study hospital was significantly higher than that of other hospitals in the country (P = 0.002).
Fig. 5 shows the composition of the average medical cost for the patients who underwent PD in the study hospital. The mean total cost was 16,583,755 Korean won (KRW) (13,819 USD). The total NHIS payment of 13,243,315 KRW (11,036 USD), which constituted 79.8% of the total cost, was made up of both payment from the NHIS (12,409,315 KRW [10,341 USD], 74.8%) and patient copayments (834,000 KRW [695 USD], 5%). The actual burden to the patients included both the patient copayment portions of the NHIS payment (834,007 KRW [695 USD], 5%) and non-NHIS payments (3,339,629 KRW [2,783 USD], 20.1%), reaching a total of 4,173,636 KRW (3,478 USD) (25.1%).
Particularly useful data from HIRA reported that a total of 70 hospitals in Korea performed PD for pancreatic head cancer from January 2014 to December 2014, and the average NHIS payment per patient was 12,160,000 KRW (10,133 USD). During the same period, 6 PD operations were performed for pancreatic head cancer in the study hospital, and the mean total NHIS payment was 11,619,493 KRW (9,682 USD).
PD is a complex procedure with high mortality and morbidity. In South Korea, the morbidity and mortality rates of this procedure were reported to be 10.9%–53% and 0%–2.6%, respectively, [567] while those of other countries were 20%–53% and 1.1%–4.3%, respectively, with no statistical difference respectively, showing no statistical difference [89101112]. Although the mortality rate was relatively constant at lower than 5%, the postoperative complication rate showed a wide range, which might be due to different institutional definitions [131415]. However, overall clinical outcomes associated with PD have improved due to developments in surgical skills, perioperative management, and interventional radiology, among other factors.
Owing to the high complexity of PD, the tendency of patients undergoing this procedure to be consolidated at high-volume centers has naturally been accelerated. Moreover, a well-developed public transportation system within a relatively small territory has enabled individuals to visit large centers in a half-day. It is worth noticing that 126 hospitals performed at least one PD procedure from 2005 to 2008, for a total of 4,975 cases, out of which 38.5% were performed at only four hospitals. Consequently, major studies reporting the results of PD have been uniformly released from the mid- to high-volume hospitals in South Korea to date. [5671316]. On the other hand, accessibility to large hospitals is relatively limited for those who are subsidized by the public welfare system due to its high cost. The present study focused on the clinical outcomes of PD along with its cost-effectiveness in a mid- to low-volume hospital, specifically a public municipal institution.
Many previous studies emphasized the "volume effect" on PD, such that the performance of procedures in high-volume centers would have a more positive influence on outcomes than their performance in low-volume centers [11415171819]. Indeed, long-term outcomes such as survival rates, as well as short-term outcomes, were reported to be much more favorable in high-volume centers [2021]. These studies have supported and asserted the necessity of concentration of medical resources. However, specialized low-volume hospitals were also reported as competent to perform PD with favorable results comparable to those of high-volume hospitals [222324]. Apart from clinical outcomes, low-volume hospitals have their own roles in regard to community needs as well as social welfare [25]. For countries with wider territory, low-volume centers are necessary to cover the regional areas due to large distances to metropolitan areas [26].
The definitions of low- and high-volume hospitals are rather ambiguous from the surgical aspect. Some studies reported their institutional definition of a high-volume hospital as one with “more than 5 annual cases of PD per one surgeon” [172728]. Birkmeyer et al. [29] defined a high-volume hospital as one with “more than 11 cases annually per one center”. Three grading systems including low-, mid-, and high-volume hospitals were also introduced in some studies [2030]. Kim et al. [1] classified hospital volume into five subgroups of very low, low, medium, high, and very high, which were adjusted for Korean medical society. The number of cases in each group was approximately 20% of the total cases. In the study hospital, the average number of annual cases of PD was 14, ranging from 4 to 25 cases. The surgical capacity of the authors' hospital has gradually moved from low to medium based on the report of Kim et al. [1].
The analysis of total hospital costs is very complex in South Korea. Data regarding the amount of total NHIS payments in certain hospitals is partially open to the public at the HIRA website (www.hira.or.kr). However, released data related to the copayment portion of the NHIS payment is unreliable, and furthermore, to determine the exact cost of non-NHIS payments in other hospitals is by no means easy. Fortunately, it was clarified that although the numbers were very small, the cost of the NHIS payment for the patient with pancreatic head cancer who underwent PD in the study hospital was compared and turned out to be much lower than that of other hospitals. Moreover, several indexes demonstrated that the price of non-NHIS payments in public municipal hospitals was definitely set lower than the mean cost of other hospitals (data not shown here).
Kim et al. [1] also reported the proportion of medical aid beneficiaries in Korea as 5.8% of total patients. The proportion of medical aid beneficiaries in the study hospital was 19.1%, revealing a large difference. The relatively low medical costs in the study hospital might attract a higher proportion of patients of low socioeconomic status compared to other hospitals. In terms of comorbidity, the fact that the proportion of patients with Charlson comorbidity index scores above 3 was 66.7% in the study hospital compared to 35.0% of patients according to national data [1] might have influenced the postoperative outcomes and should also be taken into consideration.
This study showed overall complication and mortality rates of 48.1% and 3.8%, respectively. When the cases of combined resection, such as hepatectomy, gastrectomy, or colectomy were excluded, as in the report of Kim et al. [1], the mortality rate decreased to 2.6% (n = 4), which was a comparable figure to that obtained for the low-volume hospitals in their analysis (10–18 cases per year, mortality 2.5%). The support of nonsurgical departments seemed to play an important role in generating comparable outcomes of PD. Seven cases of arterial pseudoaneurysm and one case of erosive arterial bleeding were effectively controlled with transarterial embolization. In addition, preoperative biliary drainages such as PTBD, ERBD, or ENBD were performed to improve the preoperative condition of patients. Well-equipped systems and qualified personnel including gastroenterologists and interventional radiologists have contributed to the favorable and improved outcomes of PD.
In periodic analysis, POPF rate was decreased over time, even though overall complication rate was consistently high. Especially in third period, not only overall rate but also clinically relevant POPF rate dramatically decreased compared to the first and the second period. But, clinically relevant POPF has not reached significant level. We attributed it to accumulated surgical experience and improved perioperative management.
To evaluation of long-term outcome, we performed survival analysis of pancreatic head cancer. The range of survival rate of pancreatic cancer in South Korea is wide according to the period and institute (9.6%–28.8%). [5671316] Our result of survival rate as a long term outcome was comparable with other institute in South Korea.
In conclusion, PD was demanding but feasible, cost-beneficial procedure even in low-mid volume hospital. Well-equipped system and qualified personnel were considered to prerequisite for the comparable postoperative outcomes.
Figures and Tables
Fig. 1
National Health Insurance Operation System (NHIS) of Korea (http://www.nhis.or.kr). HIRA, Health Insurance Review & Assessment Service.

Fig. 2
Annual change of pancreaticoduodenectomy cases in this hospital. Annual pancreaticoduodenectomy case in this hospital has been consistently increasing and reached to average 14 cases annually, ranging from 4 to 25.

Fig. 4
Comparison of the proportion of medical aid patients between this hospital and national data In comparison with the reported data of South Korea, the proportion of medical aid beneficiaries in this hospital was significantly higher than that of other hospitals in our country. SMG-SNU, Seoul Metropolitan Government-Seoul National University Boramae Medical Center. *Kim, et al. World J Gastroenterol 2012;18:4175-81 [1].

Fig. 5
Composition of mean cost of health care service per one patient who have undergone pancreaticoduodenectomy in this hospital. The mean of total cost was 16,583,755 Korean won (KRW) (13,819 United States dollar [USD]). Total National Health Insurance Operation System (NHIS) payment 13,243,315 KRW (11,036 USD) which occupied 79.8% of total cost was made up of both payment from NHIS (12,409,315 KRW [10,341 USD], 74.8%) and patient's copayment (834,000 KRW [695 USD], 5%). And actual burden to the patients was both patient's copayment in NHIS payment (834,000 KRW [695 USD], 5%) and non-NHIS payment (3,339,629 KRW [2,783 USD], 20.1%), reaching 4,173,636 KRW (3,478 USD) (25.1%).

References
1. Kim CG, Jo S, Kim JS. Impact of surgical volume on nationwide hospital mortality after pancreaticoduodenectomy. World J Gastroenterol. 2012; 18:4175–4181.
2. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.
3. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13.
4. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007; 142:761–768.
5. Moon HJ, Jang KT, Heo JS, Choi SH, Joh JW, Kim YI. A result of surgical treatment for ductal adenocarcinoma of the head of the pancreas. Korean J Gastroenterol. 2003; 42:156–163.
6. Lee KB, Min BW, Song TJ, Suh SO, Kim YC, Choi SY. Prognosis for periampullary cancers after pancreaticoduodenectomy. J Korean Surg Soc. 2003; 64:236–242.
7. Cho JY, Han HS, Yoon YS, Hwang DW, Jung K, Kim YK. Postoperative complications influence prognosis and recurrence patterns in periampullary cancer. World J Surg. 2013; 37:2234–2241.
8. Hoem D, Viste A. Improving survival following surgery for pancreatic ductal adenocarcinoma-- a ten-year experience. Eur J Surg Oncol. 2012; 38:245–251.
9. Chamberlain RS, Gupta C, Paragi P. In defense of the whipple: an argument for aggressive surgical management of pancreatic cancer. Oncologist. 2009; 14:586–590.
10. Brown EG, Yang A, Canter RJ, Bold RJ. Outcomes of pancreaticoduodenectomy: where should we focus our efforts on improving outcomes? JAMA Surg. 2014; 149:694–699.
11. Aziz AM, Abbas A, Gad H, Al-Saif OH, Leung K, Meshikhes AW. Pancreaticoduodenectomy in a tertiary referral center in Saudi Arabia: a retrospective case series. J Egypt Natl Canc Inst. 2012; 24:47–54.
12. Yoshioka R, Yasunaga H, Hasegawa K, Horiguchi H, Fushimi K, Aoki T, et al. Impact of hospital volume on hospital mortality, length of stay and total costs after pancreaticoduodenectomy. Br J Surg. 2014; 101:523–529.
13. Kim WS, Choi DW, Choi SH, Heo JS, Kim MJ, Song SC, et al. Clinical validation of the ISGPF classification and the risk factors of pancreatic fistula formation following duct-to-mucosa pancreaticojejunostomy by one surgeon at a single center. J Gastrointest Surg. 2011; 15:2187–2192.
14. Topal B, Van de Sande S, Fieuws S, Penninckx F. Effect of centralization of pancreaticoduodenectomy on nationwide hospital mortality and length of stay. Br J Surg. 2007; 94:1377–1381.
15. Teh SH, Diggs BS, Deveney CW, Sheppard BC. Patient and hospital characteristics on the variance of perioperative outcomes for pancreatic resection in the United States: a plea for outcome-based and not volume-based referral guidelines. Arch Surg. 2009; 144:713–721.
16. Park JS, Hwang HK, Kim JK, Cho SI, Yoon DS, Lee WJ, et al. Clinical validation and risk factors for delayed gastric emptying based on the International Study Group of Pancreatic Surgery (ISGPS) Classification. Surgery. 2009; 146:882–887.
17. Enomoto LM, Gusani NJ, Dillon PW, Hollenbeak CS. Impact of surgeon and hospital volume on mortality, length of stay, and cost of pancreaticoduodenectomy. J Gastrointest Surg. 2014; 18:690–700.
18. Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand consecutive pancreaticoduodenectomies. Ann Surg. 2006; 244:10–15.
19. Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002; 346:1128–1137.
20. Fong Y, Gonen M, Rubin D, Radzyner M, Brennan MF. Long-term survival is superior after resection for cancer in high-volume centers. Ann Surg. 2005; 242:540–544.
21. Al-Refaie WB, Muluneh B, Zhong W, Parsons HM, Tuttle TM, Vickers SM, et al. Who receives their complex cancer surgery at low-volume hospitals? J Am Coll Surg. 2012; 214:81–87.
22. Afsari A, Zhandoug Z, Young S, Ferguson L, Silapaswan S, Mittal V. Outcome analysis of pancreaticoduodenectomy at a community hospital. Am Surg. 2002; 68:281–284.
23. Schell MT, Barcia A, Spitzer AL, Harris HW. Pancreaticoduodenectomy: volume is not associated with outcome within an academic health care system. HPB Surg. 2008; 2008:825940.
24. Akhtar K, Perricone VV, Chang D, Watson RJ. Experience of pancreaticoduodenectomy in a district general hospital. Br J Surg. 2000; 87:362–373.
25. Chamberlain RS, Tichauer M, Klaassen Z, Paragi PR. Complex pancreatic surgery: safety and feasibility in the community setting. J Gastrointest Surg. 2011; 15:184–190.
26. Kanhere HA, Trochsler MI, Kanhere MH, Lord AN, Maddern GJ. Pancreaticoduodenectomy: outcomes in a low-volume, specialised Hepato Pancreato Biliary unit. World J Surg. 2014; 38:1484–1490.
27. Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003; 349:2117–2127.
28. Eppsteiner RW, Csikesz NG, McPhee JT, Tseng JF, Shah SA. Surgeon volume impacts hospital mortality for pancreatic resection. Ann Surg. 2009; 249:635–640.
29. Birkmeyer JD, Finlayson EV, Birkmeyer CM. Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery. 2001; 130:415–422.
30. van Heek NT, Kuhlmann KF, Scholten RJ, de Castro SM, Busch OR, van Gulik TM, et al. Hospital volume and mortality after pancreatic resection: a systematic review and an evaluation of intervention in the Netherlands. Ann Surg. 2005; 242:781–788.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download