Abstract
Purpose
To retrospectively assess the impact of high-grade obstructions identified on initial CT on outcomes of patients with appendiceal inflammatory masses managed by nonoperative treatment.
Methods
Institutional Review Boards approved this retrospective study and informed consent was waived. Included were 52 consecutive patients diagnosed with appendiceal inflammatory masses by CT scan and managed by nonoperative treatment. The main outcome measure was treatment failure and secondary outcomes were complications and initial and total hospital stay. Patient demographics, inflammatory markers, and CT findings for presence of an appendiceal inflammatory mass and high-grade obstruction were assessed. Patients with and without high-grade obstruction were compared for patient characteristics and outcomes using Fisher exact test and Student t-test.
Results
Among 52 patients, 14 (27%) had high-grade obstruction on CT examination at presentation. No significant differences were observed in patient characteristics (P > 0.05), treatment failure (P = 0.33), complications (P = 0.29), or initial (P = 0.73) or total (P = 0.72) hospitalization between patients with and without high-grade obstruction.
Enclosed appendiceal inflammatory masses, i.e., phlegmons or abscesses, develop in approximately 2%–10% of patients with acute appendicitis [1234]; however, controversy remains about the best treatment course [56]. During initial admission, nonoperative treatments, particularly percutaneous drainage and/or antibiotics, followed by interval appendectomy, are accepted as the initial treatment for ameliorating the acute inflammatory process and avoiding a potentially hazardous operation [78]. However, this approach is associated with risk of missing or delaying diagnosis of an underlying malignancy in about 1.2% and of Crohn disease in 0.7% of patients [3]. Some studies, therefore, advocate immediate appendectomy in spite of the potential hazards of unnecessary extensive resections. This approach is technically feasible and is as safe as nonoperative treatment, with shorter hospital stays and acceptable morbidity [4910].
The evolution and use of CT have enabled accurate diagnosis of enclosed appendiceal inflammatory masses and have facilitated drainage of intra-abdominal abscesses by providing guidance for percutaneous drainage. Several studies have shown that CT helps predict the severity of appendicitis [11] or treatment outcomes in patients with appendiceal inflammatory masses [1213]. Our previous study [12] found that high-grade obstruction identified on preoperative CT is associated with immediate postoperative complications in patients who underwent immediate appendectomy for appendiceal inflammatory mass. However, we did not explore nonoperative treatment as an alternative treatment approach. To our knowledge, little previous research has addressed the impact of nonoperative treatments in this patient population, although several studies have reported predictors associated with adverse outcomes [1314151617]. The purpose of our study was, therefore, to retrospectively assess the impact of high-grade obstruction identified on initial CT on outcomes in patients with appendiceal inflammatory mass who were managed by nonoperative treatment.
This retrospective study was approved by Institutional Review Boards of Kangbuk Samsung Hospital and Bundang Jesaeng Hospital, and the requirement for informed consent was waived. From January 2005 to May 2015 and from January 2012 to December 2015, 1,288 patients were discharged with diagnosis of perforated appendicitis from 1 hospital, and 795 were discharged from another, Data were collected in an electronic database based on the Korean Standard Classification of Disease Code-7 [18]. Of the patients, 1995 who underwent immediate appendectomy as an initial treatment were excluded. Among them, 36 patients were excluded for the following reasons: 32 because CT examination was not performed at presentation, and four because initial CT scan did not indicate appendiceal inflammatory mass. Appendiceal inflammatory mass was defined as a mass consisting of an inflamed appendix enclosed by adjacent viscera and omentum, ranging from a phlegmon to a well-defined abscess [319], that was identified on CT examination at presentation. Phlegmon was characterized as diffuse and substantial inflammation of periappendiceal fat with ill-defined fluid collections. Abscess was characterized as a well-delineated, discrete collection with rim-enhancement [520]. Ultimately, 52 patients managed by a nonoperative approach (mean ± standard deviation [SD] age, 50.1 ± 23.0 years; range, 5–90 years) for an appendiceal inflammatory mass on initial CT examination were included (Fig. 1). Nonoperative treatment was defined as broad-spectrum intravenous antibiotics with percutaneous drainage or aspiration if amenable, received for at least 24 hours as an initial treatment for appendiceal inflammatory mass, regardless of interval appendectomy. These patients included 28 men (mean age, 48.9 ± 19.3 years; range, 5–78 years) and 24 women (mean age, 51.5 ± 27.2 years; range, 8–90 years).
The main outcome measure was failure of nonoperative treatment. Failed nonoperative treatment was considered to be appendectomy for persistent fever or subjective complaints (pain or tenderness) during the same hospital stay after an initial period of nonoperative treatment, appendectomy earlier than initially planned, or treatment with antibiotics for a distinct recurrent episode of abdominal pain after discharge.
Secondary outcomes were complications and hospital stay at initial and total hospital stays. A complication was defined as any adverse event attributable to appendicitis or its treatment but distinct from treatment failure. Complication rate calculation included complications associated with initial hospitalization and with interval appendectomy when applicable. Length of stay for initial hospitalizations was defined as time interval from first hospital admission to first hospital discharge [21]. Total hospitalization included the length of stay for initial hospitalization and for interval appendectomy or readmission when applicable. Outcomes were estimated based on medical records and follow-up imaging studies.
Multidetector CT examinations were performed with a 16- or 64-detector row higher scanners (Brilliance or iCT; Philips Healthcare, Cleveland, OH, USA) or 64-detector row CT machine (Somatom Sensation; Siemens Healthcare, Erlangen, Germany). CT protocols were based effective level of 50–250 mAs, 100–120 kVp, 0.625 or 1.25 collimation, 3- to 5-mm thickness reconstruction at 4- to 5-mm intervals, 0.5- or 0.75-second rotation time, and 2 mL/kg intravenous contrast agent injection after a 60- to 70-second delay given at a rate of 2 mL/sec. Images were acquired from the diaphragm dome through the pubic symphysis. Both transverse and coronal reconstruction images were obtained.
Transverse and coronal reconstruction images for initial CT scans on admission were retrospectively reviewed on a picture archiving and communication system workstation. Two abdominal radiologists (H.J.K, and M.S.K with 13 and 15 years of experience, respectively) assessed images at presentation and during follow-up by consensus. Assessors were blinded to pathological results, outcomes, and original CT interpretations, although they were aware of the inclusion criteria. They evaluated the presence of appendiceal inflammatory mass (phlegmon or abscess) and high-grade obstruction on initial CT examination at presentation and the presence of complications on follow-up images. Intestinal obstruction was assessed using the same criteria as in our previous study [12], in which low-grade obstructions were excluded to avoid ambiguity in differentiating mechanical obstruction from paralytic ileus. High-grade obstruction was defined as intestinal obstruction directly caused by appendiceal inflammation, with a greater than 50% difference in caliber between the proximal dilated bowel and the distal collapsed bowel [22], in addition to the presence of a transition zone.
Baseline characteristics including age, sex, body mass index, comorbidities, and inflammatory markers from leukocyte counts, segmented neutrophils, and C-reactive protein levels at presentation were collected from patient medical records by 2 radiologists (H.J.K, and M.S.K). Time intervals from hospital admission to percutaneous drainage procedure, from admission to appendectomy, and from admission to last hospital visit for follow-up were estimated based on medical records.
The study sample was divided into 2 groups: patients with and without high-grade obstruction identified on CT examination at presentation. The 2 groups were compared for patient characteristics and outcomes using Fisher exact test and Student t-test. Statistical analyses were performed using PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA) and a P-value less than 0.05 was considered statistically significant.
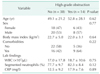
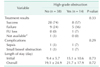
Among 52 patients, 14 (27%) had high-grade obstruction on CT examination at presentation. Table 1 summarizes the demographic characteristics and laboratory findings of patients stratified by absence or presence of high-grade obstruction identified on initial CT exam. No significant differences were observed in age, (P = 0.62), sex (P = 0.77), body mass index (P = 0.64), comorbidities (P = 0.22), leukocyte count (P = 0.75), segmented neutrophils (P = 0.12), or CRP level (P = 0.89) between patients with and without high-grade obstruction.
Outcomes of treatment failure, complications, and length of hospitalization are summarized in Table 2. No significant differences were seen in these outcomes between patients with and without high-grade obstruction.
Nonoperative management was successful in 36 patients (69%). One patient was transferred to a convalescent hospital after insertion of a percutaneous drainage catheter and was lost to follow-up. One with preexisting coronary heart disease and lung cancer cannot evaluate the treatment response because he died 3 days after initial admission due to sepsis. Failure of nonoperative management occurred in 14 patients (27%). Of these, five patients had high-grade obstruction on CT examination at presentation, while nine did not; this difference was not significant (P = 0.33).
Among 14 patients with high-grade obstruction, 8 (57%) were successfully treated by a nonoperative approach (Fig. 2); this approach failed in five who underwent appendectomy. Appendectomies were performed during the initial hospital stay in 3 patients because of persistent pain, increase in abscess size, or sepsis; interval appendectomy earlier than initially planned was needed in two patients because of recurrent pain.
The overall complication rate was 8% (4 patients). Two patients had high-grade obstruction on CT examination at presentation, and the remaining two patients did not (Table 2); this difference was not significant different (P = 0.29). Complications developed during initial hospitalization in three patients, and after appendectomy performed earlier than initially planned in one. Sepsis occurred in two patients during initial hospitalization: one with preexisting coronary heart disease and lung cancer who died three days after initial admission; one who had high-grade obstruction on initial CT underwent appendectomy and recovered. Small bowel obstruction occurred in two patients after appendectomy: one had a high-grade obstruction on initial CT exam.
The mean (±SD) length of stay was 9.4 ± 5.7 days at initial hospitalization and 19.1 ± 24.9 days total hospitalization for patients without high-grade obstruction. Mean stays were 15.1 ± 10.6 days initial and 21.7 ± 17.9 days total hospitalization, for patients with high-grade obstruction. Initial (P = 0.73) and total (P = 0.72) lengths of hospital stay were not significantly different between patients with or without high-grade obstruction (Table 2).
Percutaneous drainage catheters were inserted in 39 patients (75%) with antibiotics treatment, antibiotics alone were used in 12 (23%), and percutaneous aspiration with use of antibiotics was performed in one (2%). No significant difference was seen in the performance of percutaneous drainage between patients with or without high-grade obstruction (P = 0.47).
Interval appendectomy was performed in 36 patients (69%). Of these, 12 underwent appendectomy before the electively scheduled time because of treatment failure; five of these 12 patients had high-grade obstruction on initial CT exam.
Mean (±SD) time intervals measured from hospital admission were 12.4 ± 7.1 hours for percutaneous drainage procedure, 12.9 ± 16.0 weeks for appendectomy, and 19.0 ± 25.3 weeks for last follow-up visit.
Since nonoperative attempts at managing appendiceal mass were first described by McPherson and Kinmonth [23], many studies have reported success with conservative management such as use of antibiotics alone, or percutaneous drainage with antibiotics [72425]. Excellent outcomes measured as lower complication rate but similar length of stay as an operative group, have also been reported [2425]. While some studies demonstrate the feasibility and safety of immediate operative approaches for appendiceal inflammatory masses [4910], centers and individual surgeons lack consensus on how to best determine treatment strategies (i.e., operative vs. nonoperative approaches) for patients with appendiceal inflammatory mass. Consensus is also lacking about which patients are best suited for which treatment strategy [123457101920].
Previous studies have investigated variables affecting outcomes according to individual treatment approach [121314151617]. Our recent study reported that high-grade obstruction identified on preoperative CT is a predictor associated with 30-day adverse events in patients who underwent immediate appendectomy for appendiceal inflammatory mass [12]. However, that study did not explore the impact of high-grade obstruction on outcomes in patients with appendiceal inflammatory mass treated nonoperatively. Therefore, our present study sought to determine if presence of high-grade obstruction identified on initial CT could affect outcomes for patients with appendiceal inflammatory mass managed with nonoperative treatment.
Our results demonstrated no significant difference in treatment failure between patients with and without high-grade obstruction identified on CT scan at presentation when appendiceal inflammatory mass was managed with non-operative treatment. This finding conflicts with a previous study by Bufo et al. [26] of 88 children with perforated appendicitis over a 2-year period, 41 of whom were treated nonoperatively followed by an interval appendectomy. Our finding also conflicts with results from Aprahamian et al. [13] of 75 children with perforated appendicitis over a 2-year period who were nonoperatively managed. These studies found that small bowel obstruction predicts treatment failure. However, the studies differed from our study in the following aspects: first, our population included all age groups with an appendiceal inflammatory mass identified on initial CT scan, whereas previous studies included only children with a perforated appendicitis, who did not necessarily have an abscess or phlegmon. The presence of appendiceal masses was not clarified in the study of Bufo et al. [26], while the study of Aprahamian et al. [13] had 56 patients (75%) in this category. Second, as nonoperative management, Bufo et al. [26] used intravenous fluid resuscitation and antibiotics without percutaneous drainage, and Aprahamian et al. [13] performed percutaneous drainage in 14 patients (19%). In our study, 77% patients received percutaneous drainage procedures. Third, the previous studies did not clarify the definition of bowel obstruction, which was evaluated by simple radiograph or CT scan. Our study included only high-grade obstruction identified on initial CT scan and excluded low-grade obstructions. We found that high-grade obstruction in appendiceal inflammatory masses could be successfully controlled and resolved, as infection and its source were effectively eliminated by broad-spectrum antibiotics with a combination of percutaneous drainage where possible (Fig. 3). Of 14 patients with high-grade obstructions, 3 (21%) underwent appendectomy at 6, 8, and 12 days during initial hospitalization; initial nonoperative approach did not improve the high-grade obstruction. The remaining 11 patients (79%) recovered from high-grade obstruction according to follow-up images of CT or simple radiographs performed until appendectomy or symptom resolution (median, 66.5 days; range, 6–525 days).
The advent of broad-spectrum antibiotics, and the percutaneous drainage technique and the use of isotonic fluid resuscitation and intestinal tube decompression have greatly reduced the mortality rate [27] and increased successful management of patients with mechanical bowel obstruction. In the patients in our study, many cases of high-grade obstructions were successfully resolved by conservative treatment. No sign of strangulation was seen in involved bowels in the initial or follow-up CT images or clinical findings. Based on our experience, we believe that high-grade obstruction attributable to appendicitis did not seem to cause strangulation, which can be a main cause of treatment failure in patients with intestinal obstruction managed with a conservative approach. It was supported by studies showing that conservative management can be successful in 79% of cases of small bowel obstruction [28].
In this study, the number of complications was too small to evaluate significant differences between patients with and without high-grade obstruction. However, three of four patients who developed complications showed treatment failure (P = 0.003); treatment response for the remaining patient could not be evaluated because he died three days after admission from sepsis. This result was consistent with a previous study that demonstrated complications to be associated the treatment failure [29].
Patients with a high-grade obstruction had an approximately six days longer initial hospitalizations and three days longer overall stay than patients without high-grade obstruction; this difference was not significant.
Our study had some limitations. First, this was a retrospective study that might have been biased in patient selection and information. Second, our study included all age groups without age stratification because of the small sample size, even though clinical presentation, course, and outcomes might differ between adult and pediatric populations. Third, the sample size was relatively small even though patients were enrolled from two tertiary centers. Additional multi-institutional studies with larger sample sizes are required to validate our results. Finally, we evaluated only the presence of high-grade obstruction among bowel obstructions assessed on initial CT examination at presentation, as in our previous study [12], because of ambiguity in differentiating low-grade mechanical obstruction from paralytic ileus [30]. Despite strict criteria for bowel obstruction that excluded milder forms, we found that high-grade obstruction could be relatively well controlled by conservative management and was not associated with adverse outcomes.
This study design was similar to that of our previous study [12] in patient selection criteria and independent variables to assess the impact of high-grade obstruction when nonoperative treatment was initially chosen over an operative approach. In conclusion, the presence of high-grade obstruction identified on initial CT scan did not significantly affect outcomes, including treatment failure, complications, or initial and total hospitalization in patients managed by nonoperative treatments for appendiceal inflammatory mass, while our previous study demonstrated the impact of high-grade obstruction on postoperative adverse outcomes when operative treatment was initially chosen. We therefore carefully suggest that nonoperative treatment might be an alternative and more optimal approach than operative treatment for managing appendiceal inflammatory masses when high-grade obstruction is identified on CT scan at presentation.
Figures and Tables
 | Fig. 2A 11-year-old girl who had an appendiceal abscess with high-grade obstruction. (A) Contrast-enhanced coronal CT image shows an appendiceal abscess (arrows) with appendicolith (arrowhead), and a point of transition (open arrow) adherent to the abscess with dilated small bowel loops (SB) proximal to the transition point, indicating high-grade obstruction. (B) Follow-up CT image obtained 14 days after percutaneous abscess drainage reveals the collapsed abscess cavity (arrows) with remaining appendicolith (arrowhead). High-grade obstruction is completely relieved. |
 | Fig. 3A 46-year-old man who had a perforated appendicitis with an appendiceal abscess. (A) Coronal CT scan at presentation shows an appendiceal abscess (arrows) with inflamed appendix (arrowhead). Dilated small bowel loop (SB) with an abrupt transition (open arrow), indicating high-grade obstruction, is adherent to the appendiceal mass (arrows). (B) Follow-up CT image obtained 7 days after percutaneous abscess drainage shows nearly collapsed abscess pocket (arrowhead) at drain catheter (asterisk) site and recovering small bowel obstruction. |
References
1. Shipsey MR, O'Donnell B. Conservative management of appendix mass in children. Ann R Coll Surg Engl. 1985; 67:23–24.
2. Tannoury J, Abboud B. Treatment options of inflammatory appendiceal masses in adults. World J Gastroenterol. 2013; 19:3942–3950.
3. Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007; 246:741–748.
4. Senapathi PS, Bhattacharya D, Ammori BJ. Early laparoscopic appendectomy for appendicular mass. Surg Endosc. 2002; 16:1783–1785.
5. Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery. 2010; 147:818–829.
6. Lane JS, Schmit PJ, Chandler CF, Bennion RS, Thompson JE Jr. Ileocecectomy is definitive treatment for advanced appendicitis. Am Surg. 2001; 67:1117–1122.
7. Hoffmann J, Lindhard A, Jensen HE. Appendix mass: conservative management without interval appendectomy. Am J Surg. 1984; 148:379–382.
8. Bleker RJ, Wereldsma JC. Colonic malignancy mimicking an appendiceal mass. Neth J Surg. 1989; 41:42–46.
9. Goh BK, Chui CH, Yap TL, Low Y, Lama TK, Alkouder G, et al. Is early laparoscopic appendectomy feasible in children with acute appendicitis presenting with an appendiceal mass? A prospective study. J Pediatr Surg. 2005; 40:1134–1137.
10. Vakili C. Operative treatment of appendix mass. Am J Surg. 1976; 131:312–314.
11. Kitaoka K, Saito K, Tokuuye K. Important CT findings for prediction of severe appendicitis: involvement of retroperitoneal space. World J Emerg Surg. 2014; 9:62.
12. Kim MS, Kim MS, Kim DH, Park HW, Park HJ, Hong HP, et al. Pre-operative CT predictors associated with 30-day adverse events in patients with appendiceal inflammatory masses who underwent immediate appendectomies. Abdom Imaging. 2015; 40:2263–2271.
13. Aprahamian CJ, Barnhart DC, Bledsoe SE, Vaid Y, Harmon CM. Failure in the nonoperative management of pediatric ruptured appendicitis: predictors and consequences. J Pediatr Surg. 2007; 42:934–938.
14. St Peter SD, Aguayo P, Fraser JD, Keckler SJ, Sharp SW, Leys CM, et al. Initial laparoscopic appendectomy versus initial nonoperative management and interval appendectomy for perforated appendicitis with abscess: a prospective, randomized trial. J Pediatr Surg. 2010; 45:236–240.
15. Maxfield MW, Schuster KM, Bokhari J, McGillicuddy EA, Davis KA. Predictive factors for failure of nonoperative management in perforated appendicitis. J Trauma Acute Care Surg. 2014; 76:976–981.
16. Nadler EP, Reblock KK, Vaughan KG, Meza MP, Ford HR, Gaines BA. Predictors of outcome for children with perforated appendicitis initially treated with nonoperative management. Surg Infect (Larchmt). 2004; 5:349–356.
17. Samuel M, Hosie G, Holmes K. Prospective evaluation of nonsurgical versus surgical management of appendiceal mass. J Pediatr Surg. 2002; 37:882–886.
18. Statistics Korea. Korean Standard Classification of Disease Code-7 [Internet]. Daejeon: Statistics Korea;c2017. cited 2016 Apr 6. Available from: https://kssc.kostat.go.kr:8443/ksscNew_web/index.jsp#.
19. Nitecki S, Assalia A, Schein M. Contemporary management of the appendiceal mass. Br J Surg. 1993; 80:18–20.
20. Martin M, Lubrano J, Azizi A, Paquette B, Badet N, Delabrousse E. Inflammatory appendix mass in patients with acute appendicitis: CT diagnosis and clinical relevance. Emerg Radiol. 2015; 22:7–12.
21. Kim MS, Park HW, Park JY, Park HJ, Lee SY, Hong HP, et al. Differentiation of early perforated from nonperforated appendicitis: MDCT findings, MDCT diagnostic performance, and clinical outcome. Abdom Imaging. 2014; 39:459–466.
22. Fukuya T, Hawes DR, Lu CC, Chang PJ, Barloon TJ. CT diagnosis of small-bowel obstruction: efficacy in 60 patients. AJR Am J Roentgenol. 1992; 158:765–769.
23. McPherson AG, Kinmonth JB. Acute appendicitis and the appendix mass. Br J Surg. 1945; 32:365–370.
24. Oliak D, Yamini D, Udani VM, Lewis RJ, Arnell T, Vargas H, et al. Initial nonoperative management for periappendiceal abscess. Dis Colon Rectum. 2001; 44:936–941.
25. Brown CV, Abrishami M, Muller M, Velmahos GC. Appendiceal abscess: immediate operation or percutaneous drainage? Am Surg. 2003; 69:829–832.
26. Bufo AJ, Shah RS, Li MH, Cyr NA, Hollabaugh RS, Hixson SD, et al. Interval appendectomy for perforated appendicitis in children. J Laparoendosc Adv Surg Tech A. 1998; 8:209–214.
27. Wangensteen OH. Historical aspects of the management of acute intestinal obstruction. Surgery. 1969; 65:363–383.
28. Fevang BT, Jensen D, Svanes K, Viste A. Early operation or conservative management of patients with small bowel obstruction? Eur J Surg. 2002; 168:475–481.
29. Kogut KA, Blakely ML, Schropp KP, Deselle W, Hixson SD, Davidoff AM, et al. The association of elevated percent bands on admission with failure and complications of interval appendectomy. J Pediatr Surg. 2001; 36:165–168.
30. Maglinte DD, Gage SN, Harmon BH, Kelvin FM, Hage JP, Chua GT, et al. Obstruction of the small intestine: accuracy and role of CT in diagnosis. Radiology. 1993; 188:61–64.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download