Abstract
Purpose
Although laparoscopic adjustable gastric banding (LAGB) is a popular bariatric procedure, few comprehensive studies have been investigated on the use of non-gastro-gastric sutures (NGGSs) for decreasing postoperative complications. This study aimed to assess and compare the safety and effectiveness of MIDBAND with or without gastro-gastric sutures (GGSs).
Methods
Between February 2013 and March 2014, 41 severely obese patients underwent primary LAGB using pars flaccid technique at double center in South Korea. Excess weight loss, operative time and postoperative complications were assessed and compared between a GGS group (group 1) and a NGGS group (group 2), and patients were followed monthly for 1 year.
Results
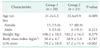
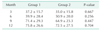
Mean body mass indices in groups 1 and 2 were 38.4 ± 4.7 and 38.9 ± 5.0 kg/m2, respectively, and mean percentage excess weight losses (%EWLs) were 59.9% ± 28.4% and 50.9% ± 20.0%, respectively, at 6 months, and 75.8% ± 26.6% and 72.5% ± 27.5%, respectively, at 12 months, and these intergroup differences of %EWL were not significant (P = 0.256 and P = 0.704, respectively). Mean operative time (57.2 minutes) was shorter in group 2 than in group 1 (79.2 minutes) (P < 0.001). In terms of complications, pouch dilatation rates were similar in the 2 groups, and no case of gastric band erosion was encountered.
Laparoscopic adjustable gastric banding (LAGB) is a restrictive surgical procedure with low morbidity and mortality rates in the immediate postoperative period and produces acceptable weight losses [123]. Nevertheless, long-term complications, such as, gastric pouch dilatation, gastric band slippage and band erosion, are not uncommon [456]. LAGB remains the bariatric procedure of choice in South Korea [7], but, the number of procedures conducted is declining rapidly because of its long-term complications [8]. Gastric erosion after LAGB is a pivotal complication, and is caused by frequent vomiting, band-associated inflammation, and ischemic change at gastric wall. Fried et al. [9] suggested that gastro-gastric sutures (GGSs), which are used to prevent acute gastric band slippage or pouch dilatation, are another cause of gastric band-associated inflammation. They postulated that GGS, themselves, might facilitate band migration, particularly if GGS bite the entire thickness of the gastric wall, creating microtrauma and potential microchannels for infection to travel from inside the stomach toward the band. Therefore, the aim of this prospective study was is to compare excess weight losses, operative times and complication rates after LAGB using MIDBAND (MID, Dardilly, France) in GGS and non-gastro-gastric suture (NGGS) groups at one year after surgery.
This study is prospective randomized controlled trial. All patients received extensive explanations about the aims of the study and on the benefits and risks of the 2 procedures. Those who agreed to participate in this study were allocated randomly to either group by random number table. Twenty-one patients underwent GGS for anterior fixation after pars flaccida technique (group 1), and 21 patients did not (group 2). The study was approved by the hospital ethics committee, and met the requirement of the Helsinki declaration.
Patients were selected using the International Federation for the Surgery of Obesity and Metabolic disorders – Asia-Pacific Chapter criteria (body mass index [BMI] > 35 kg/m2 or BMI > 30 kg/m2 with comorbidities) [10]. Potential candidates were evaluated by a multidisciplinary team. A standard preoperative assessment included nutritional counseling, psychological evaluation, upper gastrointestinal endoscopy, and blood tests. Exclusion criteria were as follows: BMI < 30 kg/m2, age < 18 or > 65 years, previous upper gastrointestinal surgery, hiatal hernia >2 cm, malignant disease, or a connective tissue disorder. Written informed consent was obtained from all patients.
The standardized LAGB procedure was conducted using the pars flaccida technique with 4 trocars. The anterior part of the band was covered using 2 GGSs to minimize the risk of slippage or pouch dilatation (Fig. 1). 2-0 Ethibond Excel (Ethicon Inc., Somerville, NJ, USA) was used for GGSs. A port was placed on the anterior sheath of the rectus abdominis muscle on the left upper abdomen. The newly released MIDBAND in South Korea was used in this study. This highly flexible silicone band measures 11 cm in length and 2 cm in width. It is recommended that saline adjustment of band should not exceed 9 cm3.
Only fluids were allowed on postoperative day (POD) 1. Patients were discharged on POD 1 and reviewed shortly afterward on POD 7. Calibration for band adjustment was performed at 6–7 weeks postoperatively. Thereafter, patients were reviewed 4 weekly during the first postoperative year. All patients were reviewed by the responsible surgeon to evaluate the need for band recalibration or to detect complications. In the event of band slippage, pouch dilatation, or significant esophageal dilatation, the band was partially or totally deflated. Follow-up and diet were the same in the two study groups. At 1 year postoperatively, patients completed a questionnaire that enabled quality of life to be assessed after gastric banding.
Fisher exact test was used to calculate P-values for categorical variables, and the student's T-test was used to calculate P-values for quantitative variables. Results were presented as mean ± standard deviations or as percentages, and P-values of <0.05 were considered as statistically significant.
Twenty-three out of 65 patients initially considered were excluded from this study, and the remaining 42 patients were randomized to the 2 study groups. However, 1 patient in group 1 was excluded due to failure to adhere to the follow-up schedule. Preoperative characteristics of the 41 patients are shown in Table 1. Of these patients, 32 (78.1%) were female and 9 (21.9 %) were male. Mean age was 33.5 years (20–60 years) at the time of LAGB. Preoperative mean weight and BMI were 105.1 kg (77–155 kg) and 38.7 kg/m2 (30.8–50.9 kg/m2). Mean length of surgery was significantly shorted in group 2 (P < 0.001). Intergroup differences in other variables were not statistically significant.
Percentages of excess weight loss (%EWL) in groups 1 and 2 are shown in Table 2, and although %EWL was higher in group 1, the difference was not significant.
Postoperative complications are shown in Table 3. No major complications were encountered in either group. Pouch dilatation developed in 4 patients (2 in groups 1 and 2). Notably, one unbuckled band, rare complication, occurred in group 2. However, no case of gastric erosion was encountered.
Many techniques have been developed to decrease postoperative complications after LAGB, and there is general agreement about posterior fixation using the pars flaccida technique. Classically, the gastric band is fixed by GGS using a variable number of nonabsorbable stitches. This technique was developed to reduce the rate of anterior slippage, but, Sakçak et al. [11] reported that GGS can induce an inflammatory reaction between stomach and band. In addition, changes in pouch pressure and gastric contractions cause imbalanced band movements, which can result in trauma and further increases the risk of migration. In other words, GGS may be a cause of gastric band erosion initiated by acute and chronic tissue damage, and for this reason, tissue damage should be minimized when making the fundal wrap. However, no randomized controlled studies have shown that GGS increases the risk of band migration [912]. Fried et al. [9] concluded imbrication sutures are not indispensable to LAGB and their use can be left to surgeon's discretion. In the present study band erosion was not observed, and thus, we suggest a long-term prospective comparative study be performed to determine the occurrence rate of band erosion, which may occur irrespective of GGS. Postoperative complications, such as, slippage, migration, and pouch dilatation, are known to affect the success of gastric banding. In a retrospective analysis of 3,584 patients that underwent LAGB by Frering and Fontaumard [13], the slippage rate was 3% in patients with GGS, and 1% in those without GGS. In a prospective randomized study, Fried et al. [9], found slippage rates of 2.2% and 2.0% in patients treated with and without GGS, and this difference was not significant. In the present study, band slippage did not occur, and in the event of pouch dilatation, or significant esophageal dilatation, the band was partially or totally deflated. Therefore, regularly follow-up is important to avoid postoperative band complications, such as, slippage, or esophageal dilatation. MIDBAND is most recent band maker developed in Europe. There are several different points between Lap-Band and MIDBAND. First, the width of the MIDBAND (2 cm) is large than lap band. It is our point of view that wider band, if properly placed with minimal dissection of perigastric fat, is more stable, and therefore, gastric prolapse would be less frequent. Second, MIDBAND is more soft and malleable than Lap band. Third, the inner balloon of MIDBAND is a single chamber. We follow up some patients who have MIDBAND as a secondary gastric band, who have had Lap-band and underwent removal. Under the same amount of saline (e.g., > 6 mL), they state that MIDBAND feels less tight (super restriction) than their previous band, and therefore less painful during eating. They also state that clogging of food (vomiting) is less frequent in MIDBAND. In our study, we were most concerned about the occurrence of band slippage in NGGS. Above characteristics of MIDBAND (wide and soft) might help to avoid band slippage in patients who underwent NGGS in this study. However, more large number of patients with longer follow-up may be needed to draw a definite conclusion for this issue. Ramos et al. [14] reported no difference between a GGS and a NGGS group with respect to weight loss or slippage or migration of band in comparative study using a Swedish adjustable gastric band, and Avsar et al. [12] reported no difference %EWLs in patients treated using a Lap-Band (Inamed Health, Santa Barbara, CA, USA). However, no prospective comparative study has been previously performed using MIDBAND. After LAGB with a MIDBAND, Blanc et al. [15] reported %EWLs of 28.3 and 42.3 at 6 and 12 months after surgery. In the present study, excellent short-term weight loss (>70 %EWL at 12 months) was achieved. Generally, patients with a high BMI, have low %EWL values regardless of the procedure chosen. Therefore, preoperative BMI should always be considered when comparing effectivenesses of weight loss between studies. Nevertheless, our data represent excellent weight loss for morbidly obese Korean patients. Regarding weight loss, we found no difference between operative fixation techniques. In other words, band fixation did not modify weight loss in the short-term. Notably, the monthly follow-up schedule adopted in this study probably played an important role in increasing weight loss after LAGB irrespective of the fixation technique used. Operation time was 22 minutes longer with band fixation in the present study. Lazzati et al. [16] reported a 10 minutes longer operation time with fixation, and Avsar et al. [12] reported a 26 minutes longer operation time, which means operation time is extended by the time needed by an experienced bariatric surgeon to create 2 to 3 stitches during laparoscopy. Complications related to the band per se are a cause of reoperation after LAGB [17]. Many operative methods have been developed to decrease the occurrence of complications after LAGB. Not using GGS resulted in significant benefits in operative time with good weight loss and safety in the present short-term comparative study. Furthermore, based on our findings, we believe that the routine use of GGS should be reconsidered. However, the present study is limit by the low number of patients enrolled and a short-term follow-up. Nonetheless, it demonstrates that MIDBAND combined with regularly follow-up and adjustment is effective and safe with or without GGS in the short-term.
In conclusion, the results of this MIDBAND study with or without GGS show good short-term weight loss and safety. GGS was not found to decrease the incidences of pouch dilatation or slippage, but did increase operation time. In the light of our findings, we believe that routine use of GGS should be reconsidered during LAGB using MIDBAND.
Figures and Tables
Fig. 1
The anterior part of the band was covered using 2 gastro-gastric sutures to minimize the risk of slippage or pouch dilatation.

References
1. Steffen R, Biertho L, Ricklin T, Piec G, Horber FF. Laparoscopic Swedish adjustable gastric banding: a five-year prospective study. Obes Surg. 2003; 13:404–411.
2. Mittermair RP, Weiss H, Nehoda H, Kirchmayr W, Aigner F. Laparoscopic Swedish adjustable gastric banding: 6-year follow-up and comparison to other laparoscopic bariatric procedures. Obes Surg. 2003; 13:412–417.
3. Zinzindohoue F, Chevallier JM, Douard R, Elian N, Ferraz JM, Blanche JP, et al. Laparoscopic gastric banding: a minimally invasive surgical treatment for morbid obesity: prospective study of 500 consecutive patients. Ann Surg. 2003; 237:1–9.
4. Himpens J, Cadiere GB, Bazi M, Vouche M, Cadiere B, Dapri G. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 2011; 146:802–807.
5. Brown JJ, Boyle M, Mahawar K, Balupuri S, Small PK. Laparoscopic adjustable gastric band survival in a high-volume bariatric unit. Br J Surg. 2013; 100:1614–1618.
6. Suter M, Calmes JM, Paroz A, Giusti V. A 10-year experience with laparoscopic gastric banding for morbid obesity: high long-term complication and failure rates. Obes Surg. 2006; 16:829–835.
7. Ahn HS, Lee HJ, Kang SH, Kim GJ, Kim SS, Kim YJ, et al. 2013 Nationwide bariatric and metabolic surgery report in Korea. J Metab Bariatr Surg. 2014; 3:38–43.
8. Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N. Bariatric surgery worldwide 2013. Obes Surg. 2015; 25:1822–1832.
9. Fried M, Dolezalova K, Sramkova P. Adjustable gastric banding outcomes with and without gastrogastric imbrication sutures: a randomized controlled trial. Surg Obes Relat Dis. 2011; 7:23–31.
10. Kasama K, Mui W, Lee WJ, Lakdawala M, Naitoh T, Seki Y, et al. IFSO-APC consensus statements 2011. Obes Surg. 2012; 22:677–684.
11. Sakcak I, Avsar MF, Hamamci EO, Bostanoglu S, Sonisik M, Bostanoglu A, et al. Comparison of early and late changes in immunoglobulins and acute phase reactants after laparoscopic adjustable gastric banding in patients with morbid obesity. Obes Surg. 2010; 20:610–615.
12. Avsar FM, Sakcak I, Yildiz BD, Cosgun E, Hamamci EO. Is gastro-gastric fixation suture necessary in laparoscopic adjustable gastric banding? A prospective randomized study. J Laparoendosc Adv Surg Tech A. 2011; 21:953–956.
13. Frering V, Fontaumard E. Does stitching band increase slipping? Surg Obes Relat Dis. 2008; 4:294.
14. Ramos A, Neto M, Galvao M, Murakami A, Lanzarini EG. Stitchless technique with Swedish adjustable gastric band. Surg Obes Relat Dis. 2007; 3:319.
15. Blanc PM, Lagoutte JM, Picot MC, Denève E, de Seguin C, Fabre JM, et al. Preliminary results of the laparoscopic adjustable gastric banding procedure by a new generation of silicone band: MIDBAND. Obes Surg. 2008; 18:569–572.
16. Lazzati A, Polliand C, Porta M, Torcivia A, Paolino LA, Champault G, et al. Is fixation during gastric banding necessary? A randomised clinical study. Obes Surg. 2011; 21:1859–1863.
17. Park JY, Song D, Kim YJ. Causes and outcomes of revisional bariatric surgery: initial experience at a single center. Ann Surg Treat Res. 2014; 86:295–301.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download