Abstract
Purpose
To develop a simple and reliable rat model of in situ reversible obstructive jaundice with low morbidity and mortality rates.
Methods
Rats were divided into 4 groups with 8 rats each: the sham-operated (SH) group only underwent laparotomy, the control internal drainage (ID-C) group underwent choledochoduodenostomy, the new internal drainage (ID-N) group and the long-term internal drainage (ID-L) group underwent choledochocholedochostomy. Common bile duct ligation was performed in all the drainage groups 7 days before reversal procedures. All rats were sacrificed for samples 7 days after the last operation except rats of the ID-L group that survived 28 days before sacrifice. Body weight, liver function, histopathological changes, morbidity and mortality were assessed.
Results
One rat died and 2 rats had complications with tube blockage in the ID-C group. No death or complications occurred in the ID-N and ID-L groups. The drainage tube remained patent in the long-term observation ID-L group. Body weight showed no significant difference between the ID-C and ID-N groups after 7 days drainage. Liver function was not fully recovered in the ID-C and ID-N groups after 7 days drainage, but statistical differences were only observed in the ID-C group compared with the SH and ID-L groups. Periportal inflammation and bile duct proliferation showed severer in the ID-C group than in the ID-N group.
Nowadays, the models of obstructive jaundice (OJ) and its reversal are frequently used in many experimental studies such as on the benefits and risks of preoperative internal and external drainage, short-term and long-term outcomes after surgery, and metabolism changes in liver and digestive tract [1234]. An ideal model for OJ and its reversal should be technically easy, stable during the study period, and associated with low mortality and morbidity rates. There already have been various kinds of methods for inducing and releasing OJ in rats, such as subcutaneously tunneled cannulation technique and tube-to-tube choledochocholedochostomy and choledochoduodenostomy [567]. However, they more or less have their own defects. It was reported that tube dislodgement and blockage were common disadvantages of cannulation techniques, and the technical complexity and high mortality and morbidity rates were common disadvantages of diverting techniques [56789]. These defects may limit the use of these models and influence the reliability of experimental results. Thus, in the present study we developed a simple and reliable rat model of OJ and in situ reversal and compared this new model with the commonly used choledochoduodenostomy model.
Thirty-two male Sprague-Dawley rats weighing 200–220 g were included in this study. They were housed under controlled temperature, humidity, and 12-hour alternate light-dark cycles. Standard rat chow and tap water were allowed ad libitum. This experiment was performed in compliance with the standards for animal use and care set by the Animal Ethics Committee of Chinese PLA General Hospital.
The rats were randomized divided into 4 groups with 8 rats each. The sham-operated (SH) group only underwent laparotomy. Other rats underwent common bile duct (CBD) double ligation and transection in the first laparotomy for inducing OJ. The releasing procedure of OJ was performed with two different internal drainage (ID) methods. A commonly used method named choledochoduodenostomy constituted the control internal drainage (ID-C) group and the new method described in the present study constituted another internal drainage (ID-N) group. To check the effect of long-term drainage of this new method, a long-term internal drainage (ID-L) group was also presented in this study.
All rats were allowed only tap water 12 hours before surgery. Operations were performed under sterile conditions with ether inhalational anesthesia. An operating microscope (Binocular Operation Microscope; Type GX.SS.22-3; Shanghai Medical Optical Instruments Co., Ltd, Shanghai, China) for small animal surgery was used during the entire operation.
CBD ligation was performed in rats of the 3 drainage groups except the SH group. The abdomen was shaved free of hair and disinfected before operation. An upper midline abdominal incision about 2.0–3.0 cm was made. The abdominal wall was separated with retractors designed for small animals (Fig. 1A). A short section of the bile duct between the beginning of the CBD and the entrance to the pancreas was selected for bile duct ligation where there was little connective tissue around. Two 8-0 black monofilament nylon sutures (Nonabsorbable Suture, Shanghai Pudong Jinhuan Medical Products Co., Ltd., Shanghai, China) were passed through under the bile duct. OJ was performed by double ligation and transection of the CBD (Fig. 1B). The use of precision surgical instruments and fine sutures could maximally reduce tissue adhesion. The abdominal wall was closed by layers with a 3-0 nonabsorbable silk suture (Mersilk, Johnson Medical Ltd., Shanghai, China). All the procedures took less than 10 minutes.
The releasing procedure of OJ was performed through the previous incision 7 days after bile duct ligation. After exposure of the dilated CBD and the pancreas, the pancreatic side of the CBD could be found near the dilated CBD with a black knot due to a little tissue adhesion (Fig. 2A). The upper part of the pancreatic side of the CBD, close to the black knot, was dissected and half-cut with precision surgical instruments. An 8-0 monofilament nylon suture was passed through under the bile duct. A plastic tube, cut from an intravenous catheter (Disposable Sterile intravascular catheters, Shanghai Pudong Jinhuan Medical Co., Ltd.), 8 mm in length, 0.8 mm in diameter, was inserted into the duodenal side of the original bile duct and tied in position with the previously placed suture with half left outside the bile duct (Fig. 2B). Transparent liquid ascending from the tube indicated the successful cannulation. Subsequently, the end of the dilated CBD was dissected and an 8-0 monofilament nylon suture was placed under the distal end. The dilated end was punctured and aspirated with a 1-mL syringe, followed by expanding the puncture point with a 16-G needle. The outside part of the tube that had been placed into the distal CBD was inserted into the dilated CBD through the punctured point and tied in position with the 8-0 suture (Fig. 2C). To avoid dislodging of the tube, suture ends of the 2 sides were tied separately. Then the tube was entirely involved in the bile duct. The operation took less than 20 minutes to complete.
Choledochoduodenostomy was performed according to the technique reported by Li and Chung [5]. Briefly, 7 days after bile duct ligation, the abdominal wall was reopened and internal drainage was achieved by connecting the dilated CBD and duodenum with a short polyvinylchloride tube (10 mm in length, 2.5 mm in diameter). The suture ends of the 2 sides were tied separately to prevent tube dislodgement. The entire procedure took 20 to 30 minutes.
Body weights were collected before operation and sacrifice. Blood sample and liver tissue were acquired under inhalation anesthesia on day 7 in the SH group and day 14 in the ID-C and ID-N groups (on day 7 after biliary drainage). In the ID-L group, samples were collected on day 35 (on day 28 after biliary drainage). The patency of the tubes were checked in all the drainage groups.
Blood samples were withdrawn from the inferior vena cava and centrifuged at a speed of 4,000 rpm for 10 minutes to isolate the serum which was stored at -80℃ until use. Serum albumin (ALB), ALT, ALP, and total bilirubin (TB) were measured in the Biochemical Laboratory of the Chinese PLA General Hospital.
Liver tissue was removed and fixed in 10% formalin. After embedded in paraffin, liver tissue was cut into 5-µm-thick sections and stained with hematoxylin and eosin (H&E). A light microscope was used to check the histopathological findings.
Data are expressed as means ± standard deviation. Statistical analysis was performed using SPSS ver. 17 (SPSS Inc., Chicago, IL, USA). Body weight was evaluated by sample t-tests and liver function parameters were analyzed by 1-way analysis of variance. A P-value of <0.05 was considered significant.
All operations were performed successfully in each group. The rats that received CBD ligation and transection in the first laparotomy showed apparent physical changes like inappetence, dark urine, and clay-colored stools. All rats survived without complications until the second laparotomy. During the second operation, mild tissue adhesion could be seen around dilated CBD in each rat. In the ID-C group, one rat died of duodenal obstruction 4 days after the second operation and 2 rats survived to sacrifice with chyme blockage in the drainage tube. No death or complications occurred in the ID-N and ID-L groups and the tubes remained patent without bile leakage even following 28 days internal drainage. Due to the large drainage tube, tissue proliferation and adhesion around the operating fields were severer in the ID-C group than the ID-N group after the second operation.
Body weight of rats changed markedly in all the groups as time went on (Fig. 3). Seven days after the first laparotomy, body weight was significantly lower in 3 CBD ligated groups than the SH group (P < 0.01). No significant difference of body weight was observed among the 3 CBD ligated groups. Following 7 days of internal drainage, body weight in both ID-C and ID-N groups had increased a lot and were significantly higher than those before the second operation, respectively (P < 0.05). Body weight showed no difference between the ID-C and ID-N groups after 7 days drainage. In the ID-L group, body weight on day 35 was significantly higher than before the second laparotomy (P < 0.001). The changes of body weight reflected that the in situ choledochocholedochostomy internal drainage was successfully established in the rats of the ID-N and ID-L groups.
Liver function parameters were still abnormal after 7 days drainage but completely recovered after 28 days drainage. Due to the 2 rats with tube blockage, the average values of ALT, ALP, and TB were higher in the ID-C group than other groups, while ALB level of the ID-C group was lower than other groups (Table 1). Statistical analysis showed that ALP and TB levels were significantly higher in the ID-C group than the SH and ID-L groups, respectively (P < 0.05). ALB level was significantly lower in the ID-C group than in the ID-L group (P < 0.05). Tube blockage led to re-obstruction of the CBD and then impaired liver function in the ID-C group. There were no significant differences between the ID-C and ID-N groups in those parameters except the TB level. Compared with the ID-C group, TB level was significant lower in the ID-N group (P < 0.05), indicating the drainage procedure of the ID-N group was more efficient and reliable than that of the ID-C group.
Histopathological changes of the liver were focused on the portal and periportal areas. The liver displayed normal hepatic lobules and portal areas in SH and ID-L groups (Fig. 4A, B). No difference was observed between the 2 groups. Microscopic inspection showed integral hepatic lobules and mild bile duct proliferation, and periportal inflammation in both ID-C and ID-N groups after 7 days drainage (Fig. 4C, D). However, the bile duct proliferation and periportal inflammation appeared lighter in the ID-N group than the ID-C group, indicating better effects of internal drainage by the new method.
The present study provided a new rat model for inducing and releasing OJ. This kind of choledochocholedochostomy performed with a fine tube within the bile duct was close to the physiological structure of CBD, which was similar to the reconstruction of bile ducts in rat liver transplantation [10]. Liver function tests and histopathological findings confirmed the efficiency of this model. ALT, TB, and ALP were significantly increased after the first operation and returned to normal after the second operation. Histopathological findings were also in accordance with other reported studies. Compared with choledochoduodenostomy, this method is technically easier with shorter operation time and rare morbidity and mortality rates. The well preserved duodenal side of the transected CBD, which was found in our experiment, contributed to the establishment of this new OJ and reversal method. By the usage of an operating microscope and an 8-0 suture, precise operation was achieved to minimize tissue adhesion, which might cause difficulties in performing a second or third laparotomy if necessary.
In current experimental studies, various kinds of rat models have been developed for inducing and releasing OJ. For example, choledochoduodenostomy described by Ryan et al. [11] have been used as the classic method but with a high mortality from drainage. Hirazawa et al. [12] designed a kind of tube-tube choledochocholedochostomy in which 2 tubes were inserted into the hepatic side and pancreatic side of the CBD, respectively, and the free ends were pulled out of the abdominal wall to induce OJ. However, cannulation failure and tube dislodgement still led to high mortality and morbidity rates in the early stage of experiments [81213]. Some studies made use of Roux-en-Y choledochojejunostomy for drainage, which is a complex method and requires skilled operators [1415]. Kahramansoy et al. [16] ligated the CBD with rapidly absorbable suture materials, and spontaneous biliary drainage was presented when these materials were degraded. This method faces a contradictory problem in that tight ligation may cause injury to the CBD in the second operation while loose ligation may fail to induce OJ.
Although there are various different rat models to choose from, researchers do not seem to accept most of them. In newly published articles, choledochoduodenostomy was still the prior internal drainage technique for many researchers [11718192021]. However, choledochoduodenostomy was not suitable in some studies because of high mortality and morbidity rates and poor stability [45916222324]. There are several common complications, such as bile leakage, biloma and tube dislodgement and blockage. When performing choledochoduodenostomy with a tube, blockage occurred in most studies due to a direct connection between CBD and duodenum. The incidence of tube blockage was as high as 50%, and Suzuki had to change from a solid diet to an oral liquid diet to prevent tube obstruction [425]. In the present study, one rat was precluded and 2 rats experienced tube blockage, which influenced the liver function tests of the ID-C group. In contrast, there were no complications or death in the ID-N and ID-L groups. For stable long-term study, reliable choledochocholedochostomy would be an ideal method.
Our new method effectively decreased most tube-related complications that occurred in other reported methods. There were no dislodgement, blockage, or mortality after surgery in our experiments with this new method. Compared with choledochoduodenostomy, this new method also minimized tissue adhesion after the second laparotomy. The possible disadvantage of this model exists in the second laparotomy: when the pancreatic side of the CBD was not directly found, it can be exposed along the black suture knot which was used for bile duct ligation in the first operation. Once the second operation is performed successfully, the rats can survive with low mortality and morbidity, and is especially suitable for long-term study of OJ and its reversal.
In conclusion, this study provided a simple and reliable rat model for the study of OJ and its reversal. Technically easy with minimal adhesion and low mortality and morbidity rates were outstanding features of this new method. It is suitable for long-term or consecutive studies which require a reliable rat model of reversible OJ.
Figures and Tables
Fig. 1
Surgical procedure of inducing obstructive jaundice (OJ). (A) Expose the common bile duct (CBD) without pulling out the duodenum. The arrow showed the whole CBD. (B) Double ligation and transection of the CBD for inducing OJ. The white arrow showed the hepatic side of the CBD. The black arrow showed the pancreatic side of the CBD.
Fig. 2
Surgical procedure of releasing obstructive jaundice (OJ) in situ. (A) Operating field before the reversal procedure. The arrow showed the pancreatic side of the CBD. (B) A plastic tube was inserted into the pancreatic side of the CBD. (C) Operating field after the second operation. The 2 sides of the CBD were connected with the tube.

Fig. 3
Body weight changes in the 4 groups. ID-C, control internal drainage group; ID-L, long-term internal drainage group; ID-N, new internal drainage group; SH, shamoperated group. *P < 0.05, 14 days vs. 7 days in ID-C and ID-N, respectively. **P < 0.01, SH vs. ID-C, ID-N, and ID-L, respectively. ***P < 0.001. 35 days vs. 7 days in ID-L.
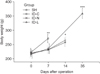
Fig. 4
Morphologic changes of the liver in the 4 groups. (A) Normal liver of the SH group (H&E, ×200). (B) Recovered portal area of the ID-L group (H&E, ×200). (C) Moderate periportal inflammation and bile duct proliferation of the ID-C group (H&E, ×100). (D) Mild periportal inflammation and bile duct proliferation of the ID-N group (H&E, ×100). ID-C, control internal drainage group; ID-L, longterm internal drainage group; ID-N, new internal drainage group.

Table 1
Liver function tests of the 4 groups

Values are presented as mean ± standard deviation.
SH, sham-operated group; ID-C, control internal drainage group; ID-N, new internal drainage group; ID-L, long-term internal drainage group; TB, total bilirubin; ALB, serum albumin.
a)ID-C vs. SH and ID-L, P < 0.05. b)ID-C vs. ID-N, P < 0.05. c)ID-C vs. ID-L, P < 0.05.
ACKNOWLEDGEMENTS
This work was supported by the National Key Technology R&D Program of China (2012BAI06B01).
References
1. Wang ZK, Xiao JG, Huang XF, Gong YC, Li W. Effect of biliary drainage on inducible nitric oxide synthase, CD14 and TGR5 expression in obstructive jaundice rats. World J Gastroenterol. 2013; 19:2319–2330.
2. Lai EC, Lau SH, Lau WY. The current status of preoperative biliary drainage for patients who receive pancreaticoduodenectomy for periampullary carcinoma: a comprehensive review. Surgeon. 2014; 12:290–296.
3. Wang S, Wang X, Li L, Dai H, Han J. Association of preoperative obstructive jaundice with postoperative infectious complications following pancreaticoduodenectomy. Hepatogastroenterology. 2013; 60:1274–1279.
4. Mizuguchi K, Ajiki T, Onoyama H, Tomita M, Kuroda Y. Short-term effects of external and internal biliary drainage on liver and cellular immunity in experimental obstructive jaundice. J Hepatobiliary Pancreat Surg. 2004; 11:176–180.
5. Li W, Chung SC. An improved rat model of obstructive jaundice and its reversal by internal and external drainage. J Surg Res. 2001; 101:4–15.
6. Yu JL, Wang LQ, Andersson R, Persson BG, Bengmark S. New model of reversible obstructive jaundice in rats. Eur J Surg. 1993; 159:163–166.
7. Hsien CS, Huang CC, Huang LT, Chung JC, Chou MH. Reversible cholestasis and cholangitis induced by biliary drainage and infusion in the rat. Eur Surg Res. 2006; 38:11–17.
8. Fukushima S, Okuno H, Shibatani N, Nakahashi Y, Seki T, Okazaki K. Effect of biliary obstruction and internal biliary drainage on hepatic cytochrome P450 isozymes in rats. World J Gastroenterol. 2008; 14:2556–2560.
9. Wu L, Li W, Wang Z, Yuan Z, Hyder Q. Bile acid-induced expression of farnesoid X receptor as the basis for superiority of internal biliary drainage in experimental biliary obstruction. Scand J Gastroenterol. 2013; 48:496–503.
10. Wang H, Li C, Xu H, Hu J, Zhang A, Ye S, et al. Precise reconstruction of veins and bile ducts in rat liver transplantation. Cell Biochem Biophys. 2014; 68:55–65.
11. Ryan CJ, Than T, Blumgart LH. Choledochoduodenostomy in the rat with obstructive jaundice. J Surg Res. 1977; 23:321–331.
12. Hirazawa K, Oka M, Ogura Y, Miyahara M, Hazama S, Suzuki T. New technique for inducing reversible obstructive jaundice in the rat. Eur Surg Res. 1997; 29:195–201.
13. Diamond T, Dolan S, Rowlands BJ. An improved technique for choledochoduodenostomy in a rat model of obstructive jaundice. Lab Anim Sci. 1991; 41:82–83.
14. Lee JS, Hong TH. The rat choledochojejunostomy model for microsurgical training. Ann Surg Treat Res. 2016; 90:246–249.
15. Takagi T, Yokoyama Y, Kokuryo T, Yamaguchi J, Nagino M. Liver regeneration following experimental major hepatectomy with choledochojejunostomy. Br J Surg. 2015; 102:1410–1417.
16. Kahramansoy N, Erkol H, Yilmaz EE, Şit M, Yilmaz F, Tosun M, et al. A new model of reversible obstructive jaundice using rapidly absorbable suture materials. Clin Invest Med. 2012; 35:E351–E357.
17. Matsumoto T, Ajiki T, Kajiwara E, Mita Y, Fujita T, Morimoto H, et al. Decreased expression of intestinal chemokine TECK/CCL25 in experimental obstructive jaundice and its reversal following internal biliary drainage. J Gastroenterol. 2008; 43:390–396.
18. Liu YJ, Mao EQ, Ouyang B, Chen J, Tang YQ, Huang SW, et al. Effect of biliary tract external drainage on cytokine expression and histomorphology of intestine, liver, and lung in rats with hemorrhagic shock. Crit Care Med. 2009; 37:2800–2806.
19. Yiming Z, Lei J, Renyou Z, Shan K, Xue L, Min L, et al. Evaluation of the uptake function of liver in rats with obstructive jaundice before and after relief from obstruction by superparamagnetic iron oxide-enhanced magnetic resonance imaging. Oncol Lett. 2012; 4:221–226.
20. Padillo FJ, Cruz A, Segura-Jiménez I, Ruiz-Rabelo J, Vázquez-Ezquerra MR, Perea-Alvarez MD, et al. Anti-TNF-alpha treatment and bile duct drainage restore cellular immunity and prevent tissue injury in experimental obstructive jaundice. Int J Immunopathol Pharmacol. 2007; 20:855–860.
21. Tian Y, Xia M, Zhang S, Fu Z, Wen Q, Liu F, et al. Initial study of sediment antagonism and characteristics of silver nanoparticle-coated biliary stents in an experimental animal model. Int J Nanomedicine. 2016; 11:1807–1817.
22. Oruc MT, Ozmen MM, Han U. A new technique for inducing and releasing obstructive jaundice in rats. Eur Surg Res. 2009; 43:354–359.
23. Mizuta A, Chijiiwa K, Saiki S, Kuroki S, Nakamura K, Tanaka M. Differences in biliary lipid excretion after major hepatectomy in obstructive jaundiced rats with preoperative internal, external, or no biliary drainage. Eur Surg Res. 2002; 34:291–299.
24. Sano T, Ajiki T, Takeyama Y, Kuroda Y. Internal biliary drainage improves decreased number of gut mucosal T lymphocytes and MAdCAM-1 expression in jaundiced rats. Surgery. 2004; 136:693–699.
25. Suzuki H, Iyomasa S, Nimura Y, Yoshida S. Internal biliary drainage, unlike external drainage, does not suppress the regeneration of cholestatic rat liver after partial hepatectomy. Hepatology. 1994; 20:1318–1322.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download