Abstract
Purpose
The current study aims to analyze the risk factors for the failure of ileostomy reversal after laparoscopic low anterior resection for rectal cancer.
Methods
All patients who underwent a laparoscopic low anterior resection for rectal cancer with a diverting ileostomy between 2007 and 2014 were abstracted. The patients who underwent and did not undergo a diverting ileostomy procedure were compared regarding patient, tumor, treatment related parameters, and survival.
Results
Among 160 (103 males [64.4%], mean [± standard deviation] age was 58.1 ± 11.9 years) patients, stoma reversal was achieved in 136 cases (85%). Anastomotic stricture (n = 13, 52.4%) was the most common reason for stoma reversal. These were the risk factors for the failure of stoma reversal: Male sex (P = 0.035), having complications (P = 0.01), particularly an anastomotic leak (P < 0.001), or surgical site infection (P = 0.019) especially evisceration (P = 0.011), requirement for reoperation (P = 0.003) and longer hospital stay (P = 0.004). Multivariate analysis revealed that male sex (odds ratio [OR], 7.82; P = 0.022) and additional organ resection (OR, 6.71; P = 0.027) were the risk factors. Five-year survival rates were similar (P = 0.143).
Conclusion
Fifteen percent of patients cannot receive a stoma reversal after laparoscopic low anterior resection for rectal cancer. Anastomotic stricture is the most common reason for the failure of stoma takedown. Having complications, particularly an anastomotic leak and the necessity of reoperation, limits the stoma closure rate. Male sex and additional organ resection are the risk factors for the failure in multivariate analyses. These patients require a longer hospitalization period, but have similar survival rates as those who receive stoma closure procedure.
Defunctioning stomas are commonly created in order to divert the bowel stream mostly in cases of distal anastomosis, particularly after low anterior resection. A temporary ileostomy may decrease the risk of anastomotic leak, which is a lethal complication [12345]. This may limit the septic sequence in cases of anastomotic leak and may help the diseased anastomosis to heal the area of inflammation [16]. Stomas may decrease the necessity of urgent reoperation due to intraabdominal sepsis that may occur after anastomotic leak [67]. Stoma complications are generally easily managed and stoma reversal is associated with limited morbidity [18]. Thus, selective or routine creation of diverting stomas has been recommended in patients who undergo low anterior resection [9].
The failure of stoma closure may occur, which stems from the decision of not performing stoma takedown due to various reasons. This is probably one of the worst scenarios for a patient who recently had a sphincter preserving procedure for rectal cancer and has been expecting to have regular bowel movements through a functional anus after a stoma takedown. However, up to 30% of ‘temporary’ stomas are never closed [910111213141516171819]. Several studies have underlined different factors causing the failure and delay of stoma reversal; but have been criticized, since they analyze heterogeneous patient populations having benign and malignant diseases, elective or emergent procedures, and/or anterior or low anterior resections. They also include different types of stomas (i.e., colostomies, ileostomies, and even end stomas in some analyses) [9101112131417]. Finally, survival has never been previously evaluated in these patients. Thus, the current study aims to present a single-surgeon experience of the rate of diverting ileostomy takedown and the factors affecting the failure of stoma reversal in patients who underwent laparoscopic low anterior resection for rectal cancer. Moreover, these data expose the effect of failure of stoma closure on survival.
Institutional Review Board of Kartal Education and Research Hospital approved the design and content of the study prior to data abstraction (reference number: B104ISM4340029/1009/56). A retrospective chart review has been initiated on patients who underwent laparoscopic low anterior resection for rectal cancer with a diverting ileostomy between 2007 and 2014. In addition, missed or confirmative information was obtained from a computer-based archive. The exclusion criteria in order to homogenize the information were as follows: patients undergoing an operation for a benign or recurrent disease or an emergent condition; patients with in situ cancer or dysplasia; patients with malignant diseases other than adenocarcinoma; patients treated with a restorative proctocolectomy; patients who did not have a definitive procedure but a diverting stoma for a nonresectable tumor; and patients who received a diverting/end colostomy or end ileostomy, even if the aim was temporary. Patients who had a recurrent disease and/or nonresectable metastasis which occurred after stoma creation were also excluded, since these cases required further treatment for their undergoing diseases and the stoma takedown procedure was often impossible or postponed in these cases. Finally, patients who received a temporary stoma during the previous 12 months were also excluded, since they were accepted to be on the waiting list.
The location of cancer was defined considering the distance between the dentate line and the distal edge of the tumor; and tumors located <6 cm, 6 to 12 cm, and >12 cm from the dentate line were labeled as low, mid, and upper rectal cancers, respectively [20]. Patients with an advanced tumor (T3–4 or node positive) located at the distal two thirds of the rectum received preoperative chemoradiation therapy. A multidisciplinary board consisting of specialists from all fields in oncology has been working in our institution for over 2 decades. Patients requiring a multidisciplinary approach were evaluated by this board in order to discuss and choose the treatment plan. A stoma-therapy nurse instructed and informed the patients about stoma care and its sequences, and marked possible stoma sites prior to the operation. The decision for stoma creation was made at the end of the operation considering several aspects including general condition of the patient, receiving/omitting neo-adjuvant radiation therapy, level of anastomosis and intraoperative features such as intraoperative bleeding, operative time, and a narrow pelvis. At the end of the operation, the location of the ileostomy on terminal ileum was laparoscopically decided considering a length of approximately 20 cm from the ileocecal valve. During the stoma creation procedure, the previously marked skin was excised and a vertical incision through the rectus muscle was performed and the ileal segment was taken out. An anastomosis between the serosa and the subdermal tissue was made with 3/0 polyglactin (Vicryl, Ethicon Inc., Somerville, NJ, USA) sutures, after the bowel was bridged over the stoma rod. Stomas were created in the right lower quadrant of the abdomen in all patients. A single surgeon performed the operation or supervised the procedure by scrubbing while deciding all critical points, since our institution is a training hospital.
The rate of ileostomy takedown was determined among all cases, and the risk factors for the failure of stoma closure were analyzed. Patients who received stoma closure were compared with those who did not considering aspects such as: demographics, tumor localization, presence of neoadjuvant radiation therapy, intraoperative information (synchronous hepatic metastasectomy, anastomotic technique, conversion, additional organ resection and reservoir creation rates, operation time, and quantity of bleeding), postoperative data (complications and rate and causes of reoperations), the requirement and amount of transfusions, tumor stage, length of hospital stay, and survival.
Data were analyzed by using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). Results were given as percentages, mean and standard deviations or median and ranges. Quantitative and qualitative variables were compared with Student t-test or Mann-Whitney U-test and chi-square (Pearson or Fischer exact) tests, respectively. A multivariate analysis model was established considering the parameters that had a P-value less than 0.1 in univariate analysis. A Kaplan-Meier analysis was used while evaluating survival. A P-value less than 0.05 was considered to be significant.
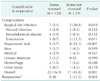
After the exclusion of patients who did not fulfill the inclusion criteria, there were 170 patients who underwent a laparoscopic low anterior resection for rectal cancer. A diverting stoma was absent from 10 cases. Therefore, the current study included a total number of 160 patients (103 males [64.4%], mean [± standard deviation, SD] age was 58.1 ± 11.9 years) (Fig. 1). The numbers of tumors located at low, mid, and upper rectum were 82 (51.3%), 58 (36.3%), and 20 (12.5%), respectively. Stoma reversal was achieved in 136 patients (85%) after a mean (± SD) period of 8.5 ± 4.4 months. If patients whose refusal was not considered as an objective reason not to perform a stoma closure were excluded, the stoma closure rate would increase to 87.5%. Anastomotic leak was the most common reason for the failure of stoma takedown. Three cases, who had had an additional urinary procedure at the time of surgery because of an advanced (clinical T4) disease, had impaired healing and consequent urinary problems including fistula, nephrostomy, and/or urinary incontinence (Table 1). The specialized urologists did not allow the stoma closure procedure to be done during the study period, since these patients required further medical or surgical treatments. Among the evaluated perioperative aspects, having a postoperative complication, particularly an anastomotic leak, were the major risk factors for the failure of stoma closure (Tables 2, 3). Surgical site infection, especially evisceration, and male sex were other risk factors. A multivariate analysis was also completed considering these parameters which had a P-value less than 0.1 in the univariate analysis, which include sex, additional organ resection, evisceration, surgical site infection, anastomotic leak, overall complication, necessity of reoperation and hospital stay. Male sex (odds ratio [OR], 7.82; 95% confidence interval [Cl], 1.34.45.67; P = 0.022) and additional organ resection (OR, 6.71; 95% Cl, 1.24.36.2, P = 0.027) were found to be statistically significant features for the failure of stoma closure (Table 4). There were 3 cases needing re-peration due to anastomotic leak and consequent intraabdominal sepsis. Failure of stoma closure was correlated with the requirement of reoperation and a longer hospitalization period as well (P < 0.05 for both) (Table 3). Five-year survival rates were similar, which were 80.8% and 72.2% in stoma-reversed and stoma not reversed groups, respectively (P = 0.143) (Fig. 1).
Diverting ileostomies may decrease the severity of symptoms and need for reoperation in cases anastomotic leak after low anterior resection [1234562122]. In addition, reversal of loop ileostomy is safe and is shown to be associated with a mortality rate as low as 0.4 % [23]. Unfortunately, some ‘temporary’ stomas cannot be closed, and some of the studies analyzing the risk factors for the failure of stoma closure have some methodical problems mostly due to the heterogeneity of the information [91011121314]. These data consist of different types of stomas including colostomies and ileostomies; surgeries including anterior and low anterior resections or laparoscopic and open procedures, and indications including malignant and benign diseases. Thus, the current study has included a highly select group of patients who underwent laparoscopic low anterior resection with a diverting ileostomy for rectal cancer.
The overall stoma reversal rate after anterior resection varies from 68% to 92% in the literature, and it was 85% in the current study [191011121314]. Moreover, some would not consider patients' refusal as an objective reason for stoma closure; the rate would then increase to 87.5%, after the exclusion of these cases. Besides, poor general condition and presence of comorbidities might also be assumed as uncertain reasons in deciding whether or not to have a stoma closure. Despite these facts, current data reflect a well-defined and highly select group of patients, as it does not include patients with benign disease or those who underwent anterior resection—who are probably more likely to be candidates for a stoma reversal. We believe that surgeons need to consider that at least some ‘temporary’ ileostomies in patients, who receive diverting ileostomy after low anterior resection for rectal cancer, will never be closed; and patients who are candidates for a diverting ileostomy deserve to be informed accordingly.
The factors evaluating the failure of stoma closure have rarely been studied. A notable multivariate analysis on the Dutch preoperative radiation therapy trial has revealed that the stoma reversal rate was significantly low in cases that required a secondary stoma creation due to anastomotic complications including leakage, fistula, or stenosis [11]. Other studies have also disclosed that the rate of stoma reversal is decreased in patients who had anastomotic problems during the initial operation [91013]. The current study showed similar findings and disclosed that anastomotic problems, particularly stricture or fistula, are generally consequences of an anastomotic leakage; hence, these are the leading reasons for the failure of stoma closure. Consequently, the overall complication rate was significantly higher in patients who could not receive a stoma takedown. This was particularly true for those who suffered from anastomotic leakage or surgical site infection, especially evisceration. There were 3 cases in this study needing reoperation for anastomotic problems and secondary septic complications. Stoma closure could not be achieved in these patients. According to our study, postoperative anastomotic problems and accompanying complications including surgical site infections are likely to be the main risk factors preventing stoma closure after laparoscopic low anterior resection.
Stoma reversal was not achieved in three other cases because of urinary complications including urinary incontinence, presence of percutaneous nephrostomy and fistula from ureteroneocystostomy. All of these cases had received additional organ resections because of extended diseases during the initial procedures. A previous article from our institution revealed that 5.5% of patients with colorectal cancer might face colonic, urinary, or biliary anastomotic leakage, if they had received a multivisceral resection [24]. As it was shown to be a significant risk factor in multivariate analysis, we believe that additional organ resections might adversely affect the possibility of stoma reversal. Patients' general condition may also have a role, and either surgeon or the patient himself/herself may refuse to continue with an additional operation for stoma closure. Finally, the current study has concluded that male sex was an important risk factor preventing stoma closure. In our opinion, this is more likely to be related to the narrow construction of the pelvis in males. Male sex has long been known to increase intrapelvic anastomotic complications, and a recent study has shown that it may increase the possibility of anastomotic leak more than three times in cases of low anterior resection (OR, 3.2; 95% CI, 1.8–5.7) [2]. However, although it has been expected, male sex has previously never been underlined as a risk factor decreasing stoma closure rate.
The current study provides significant information about the survival of patients who underwent low anterior resection with a diverting stoma for rectal cancer, which has not been previously studied. We believe that patients who did and did not receive a stoma closure procedure were comparable since oncological information was not statistically different within these groups. Our data have suggested that the failure of stoma closure did not worsen the survival rate (80.8% vs. 72.2%, P = 0.143). This is an important finding that has never been mentioned before. However, it is necessary to be cautious about this finding since the failure of stoma closure is generally related to a septic sequel of an anastomotic leak, which may be related to worsening oncological outcomes, since the lengthened treatment process may alter the immune response and delay the medical oncological treatment.
Some may question that most patients, even those with upper rectal cancers, received a diverting stoma, and the stoma creation was omitted in only 10 out of 170 cases in the current series. However, in our daily practice most cases including those with upper rectal tumors receive a total mesorectal excision instead of a partial one, necessitating a low rectal anastomosis close to the dentate line. Thus, a diverting stoma has been our preference in most instances, although recent analyses omit stoma creation in more than half of these patients [2425].
The current study has some limitations mainly due to the volume and the design of the study. The number of patients was limited in the current study, since the analysis aims to prevent heterogeneity and to reflect the experience of a single colorectal surgeon. Patients with metastasis or recurrent disease were not candidates for stoma closure, and inclusion of these patients may alter the reliability of findings and conclusions. In addition, the cases with incomplete follow-up period of 12 months were also excluded; since they might be on the waiting list in daily practice. Regarding the design of the study, the retrospective nature of data abstraction was the leading limitation restricting the reliability of the current data. However, we still believe that the current study provides notable information on the fortune of patients receiving diverting stoma after laparoscopic low anterior resection performed for rectal cancer.
In conclusions, 85% of patients, who have laparoscopic low anterior resection for rectal cancer have their stomas reversed. Anastomotic stricture is the leading reason for the failure of stoma closure. Having a complication, particularly anastomotic leak and the necessity of reoperation, is also limiting to the possibility of stoma closure. Male sex and additional organ resection are the main risk factors in preventing stoma closure in multivariate analysis. These patients require a longer hospitalization period, but have similar survival as those who receive stoma closure. In our opinion, patients who will receive a low anterior resection for rectal cancer should be informed about the possibility that their stomas may not be closed.
Figures and Tables
Fig. 1
A Kaplan-Meier analysis has revealed that the 5-year survival rates were similar between patients whose stomas were reversed and those whose stomas were not (80.8% vs. 72.2%, P = 0.143).
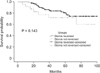
Table 2
Demographics and perioperative aspects in patients underwent stoma closure and those still living with their ileostomies

ACKNOWLEDGEMENTS
The authors would like to thank to Ass. Prof. Hanefi Ozbek, MD, for his expert contribution on statistical analyses of the study.
Notes
References
1. Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, Purkayastha S. The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis. 2009; 24:711–723.
2. Shiomi A, Ito M, Maeda K, Kinugasa Y, Ota M, Yamaue H, et al. Effects of a diverting stoma on symptomatic anastomotic leakage after low anterior resection for rectal cancer: a propensity score matching analysis of 1,014 consecutive patients. J Am Coll Surg. 2015; 220:186–194.
3. Tilney HS, Sains PS, Lovegrove RE, Reese GE, Heriot AG, Tekkis PP. Comparison of outcomes following ileostomy versus colostomy for defunctioning colorectal anastomoses. World J Surg. 2007; 31:1142–1151.
4. Saghir JH, McKenzie FD, Leckie DM, McCourtney JS, Finlay IG, McKee RF, et al. Factors that predict complications after construction of a stoma: a retrospective study. Eur J Surg. 2001; 167:531–534.
5. Huser N, Michalski CW, Erkan M, Schuster T, Rosenberg R, Kleeff J, et al. Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg. 2008; 248:52–60.
6. Karanjia ND, Corder AP, Holdsworth PJ, Heald RJ. Risk of peritonitis and fatal septicaemia and the need to defunction the low anastomosis. Br J Surg. 1991; 78:196–198.
7. Matthiessen P, Hallbook O, Rutegard J, Simert G, Sjodahl R. Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg. 2007; 246:207–214.
8. Kaidar-Person O, Person B, Wexner SD. Complications of construction and closure of temporary loop ileostomy. J Am Coll Surg. 2005; 201:759–773.
9. Poon RT, Chu KW, Ho JW, Chan CW, Law WL, Wong J. Prospective evaluation of selective defunctioning stoma for low anterior resection with total mesorectal excision. World J Surg. 1999; 23:463–467.
10. Bailey CM, Wheeler JM, Birks M, Farouk R. The incidence and causes of permanent stoma after anterior resection. Colorectal Dis. 2003; 5:331–334.
11. den Dulk M, Smit M, Peeters KC, Kranenbarg EM, Rutten HJ, Wiggers T, et al. A multivariate analysis of limiting factors for stoma reversal in patients with rectal cancer entered into the total mesorectal excision (TME) trial: a retrospective study. Lancet Oncol. 2007; 8:297–303.
12. Chand M, Talbot R, Nash G. Closure of temporary stoma after anterior resection. Colorectal Dis. 2007; 9:758–759.
13. Daluvoy S, Gonzalez F, Vaziri K, Sabnis A, Brody F. Factors associated with ostomy reversal. Surg Endosc. 2008; 22:2168–2170.
14. David GG, Slavin JP, Willmott S, Corless DJ, Khan AU, Selvasekar CR. Loop ileostomy following anterior resection: is it really temporary? Colorectal Dis. 2010; 12:428–432.
15. Kim YA, Lee GJ, Park SW, Lee WS, Baek JH. Multivariate analysis of risk factors associated with the nonreversal ileostomy following sphincter-preserving surgery for rectal cancer. Ann Coloproctol. 2015; 31:98–102.
16. Floodeen H, Lindgren R, Matthiessen P. When are defunctioning stomas in rectal cancer surgery really reversed? Results from a population-based single center experience. Scand J Surg. 2013; 102:246–250.
17. Sier MF, van Gelder L, Ubbink DT, Bemelman WA, Oostenbroek RJ. Factors affecting timing of closure and non-reversal of temporary ileostomies. Int J Colorectal Dis. 2015; 30:1185–1192.
18. Waterland P, Goonetilleke K, Naumann DN, Sutcliff M, Soliman F. Defunctioning ileostomy reversal rates and reasons for delayed reversal: does delay impact on complications of ileostomy reversal? A study of 170 defunctioning ileostomies. J Clin Med Res. 2015; 7:685–689.
19. Gastinger I, Marusch F, Steinert R, Wolff S, Koeckerling F, Lippert H, et al. Protective defunctioning stoma in low anterior resection for rectal carcinoma. Br J Surg. 2005; 92:1137–1142.
20. Pilipshen SJ, Heilweil M, Quan SH, Sternberg SS, Enker WE. Patterns of pelvic recurrence following definitive resections of rectal cancer. Cancer. 1984; 53:1354–1362.
21. Peeters KC, Tollenaar RA, Marijnen CA, Klein Kranenbarg E, Steup WH, Wiggers T, et al. Risk factors for anastomotic failure after total mesorectal excision of rectal cancer. Br J Surg. 2005; 92:211–216.
22. Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M. Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg. 1998; 85:355–358.
23. Gezen C, Kement M, Altuntas YE, Okkabaz N, Seker M, Vural S, et al. Results after multivisceral resections of locally advanced colorectal cancers: an analysis on clinical and pathological t4 tumors. World J Surg Oncol. 2012; 10:39.
24. Phatak UR, Kao LS, You YN, Rodriguez-Bigas MA, Skibber JM, Feig BW, et al. Impact of ileostomy-related complications on the multidisciplinary treatment of rectal cancer. Ann Surg Oncol. 2014; 21:507–512.
25. Seo SI, Yu CS, Kim GS, Lee JL, Yoon YS, Kim CW, et al. The role of diverting stoma after an ultra-low anterior resection for rectal cancer. Ann Coloproctol. 2013; 29:66–71.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download