Abstract
Purpose
Laparoscopic cholecystectomy (LC) is one of the most commonly performed surgeries in the world today. However, there is no consensus regarding whether LC can be performed in patients with acute cholecystitis while on antithrombotic therapy. The objective of our study was to describe postoperative outcomes of patients who underwent emergent LC without interruption to antithrombotic therapy.
Methods
We performed a retrospective review of patients who underwent LC for acute cholecystitis while on antithrombotic therapy from 2010 to 2015 at Soonchunhyang Universtiy Cheonan Hospital. Patients were divided into 2 groups as underwent emergent LC and elective LC.
Results
A total of 67 patients (emergent group, 22; elective group, 45) were included in the analysis. Elective group had significantly longer duration between the admission and operation (8 [7–10] days vs. 2 [1–3] days, P < 0.001) and longer duration of antithrombotic drugs discontinuation (7 days vs. 1 [0–3] days, P < 0.001). Emergent group had significantly more postoperative anemia (6 patients vs. 0 patient, P = 0.001) and 3 of 6 patients received packed RBC transfusion in postoperative period. However, there was no significant difference in length of postoperative stays, length of intensive care unit stays and mortality rates.
Laparoscopic cholecystectomy (LC) is one of the most commonly performed surgeries in the world today. There is also an increase in the number of patients receiving antithrombotic therapy among patients receiving LC due to increased incidence of cardiovascular and cerebrovascular diseases [1]. Although it is well known that performing early LC in patients with acute cholecystitis (AC) has good results [234], there is no consensus regarding whether LC can be performed in aforementioned patients. In respect to recent guideline [56], surgery associated with massive bleeding and difficult hemostasis (e.g., LC for severe AC) is performed after discontinuation of medication in the patient group receiving antithrombotic therapy due to high incidence of hemorrhagic complications. Therefore, LC is delayed in many cases. Hence, surgeons are concerned about the optimal timing for LC for AC in elderly patients who have multiple comorbidities and medication history, especially if they are on antithrombotic therapy.
Typical medications used for antithrombotic therapy are anticoagulant agents and antiplatelet agents. Recently, it has been reported that there is no significant difference in the long term effect between the 2 groups of medications (anticoagulant agents and antiplatelet agents) [7]. Accordingly, monotherapy and combination therapies are used depending on the underlying diseases and the risk of thromboembolic events in patients. Typically, the bleeding risk is very high when the combination therapy of these two agents is used [89]. Especially, when antiplatelet therapy is used as monotherapy or in combination, it can prevent thrombotic events and manage cardiovascular events by inhibiting various platelet receptors. It has a major role in decreasing mortality and morbidity caused by cardiovascular events in elderly patients. However, antithrombotic effects are associated with increased risk of intraoperative hemorrhage. Therefore, premature discontinuation of antithrombotic therapy has been recommended to patients before surgeries.
The objectives of this study were: (1) to evaluate postoperative outcomes of patients who underwent emergent LC without interruption to antithrombotic therapy among patients with AC while on antithrombotic therapy, and (2) to determine whether antithrombotic agent should be continued or not when performing LC in patients with AC in comparison to patients who underwent elective LC after stopping the medication.
We performed a retrospective review of patients who underwent LC for AC while on antithrombotic therapy from 2010 to 2015 at Soonchunhyang Universtiy Cheonan Hospital. Medical records of all patients were obtained. A total of 67 patients who underwent LC for AC while on antithrombotic therapy were analyzed. Antithrombotic therapy was discontinued more than 7 days before surgery in the elective group and was not stopped or prematurely stopped in the emergent group.
We classified patients into 2 groups: (1) patients underwent elective operation, and (2) patients underwent emergency operation. We considered the severity and duration of abdominal pain, physical examination, laboratory findings (WBC, CRP), presence of fever, and presence of informed consent before deciding emergency LC.
The following data were recorded: demographic data including age and sex, physical examination findings, vital signs, medication history, comorbidities, laboratory parameters, presence of common bile duct stones, preoperative percutaneous transhepatic gallbladder drainage procedure, duration of antithrombotic drugs discontinuation, time to operation, operative intervention details, postoperative complications, postoperative transfusion, length of hospital and intensive care unit (ICU) stay, and in-hospital mortality. We defined intraoperative hemorrhage as intraoperative blood loss of >100 mL, and postoperative anemia was defined as a drop >2 g/dL in hemoglobin postoperatively. Blood transfusion was defined as the units of packed RBC the patients received.
Patients were diagnosed with AC based on clinical findings such as right upper quadrant pain, tenderness including Murphy sign, fever, laboratory findings including leukocytosis, and CT findings such as presence of gall stones, thickened gall bladder wall, pericholecystic fat infiltration, and fluid collection. If patients were suspected of having common bile duct stones with cholangitis, they underwent magnetic resonance cholangiopancreatography. If they were diagnosed with common bile stones with cholangitis, preoperative endoscopic retrograde cholangiopancreatography was performed to remove common bile duct stones.
All data were analyzed by PASW Statistics ver. 18.0 (SPSS Inc, Chicago, IL, USA). Data were presented as mean ± standard deviation for continuous variables and frequency for categorical variables. P-values were derived from independent t-test or Mann-Whitney U-test for continuous variables and chi-square test or Fisher exact test for categorical variables as appropriate. A P-value of <0.05 was considered significant.
This study was approved by the Institutional Review Board at the Soonchunhyang Universtiy Cheonan Hospital (SCHLA 201606021).
We reviewed a total of 67 patients who underwent LC due to AC while on antithrombotic therapy, including 45 patients in the elective LC group and 22 patients in the emergent LC group. The elective group consisted of 19 patients on single antiplatelet therapy, 23 patients on dual antiplatelet therapy, and 3 patients on anticoagulants therapy. The emergency group consisted of 11 patients on single antiplatelet therapy, 10 patients on dual antiplatelet therapy, and 1 patient on anticoagulant therapy.
Their mean age was 71.96 ± 10.24 years. There was no significant difference in age between the 2 groups. There were a total of 44 male patients, 11 of which were in the elective LC group. There was no significant difference in previous operation history, presence of common bile duct stones between the 2 groups. However, the rates of cerebral disease were different significantly between the 2 groups. Cerebral disease was more prevalent in the emergency LC group compared to that in the elective LC group (50.0% vs. 20.0%, P = 0.025). Of the 67 patients, 19 underwent percutaneous transhepatic gallbladder drainage (PTGBD) before operation, including 17 in the elective LC group and 2 in the emergent LC group (17 patients [37.8%] vs. 2 patients [9.1%], P = 0.031). The group of patients who underwent elective LC had longer duration (8 [7–10] days vs. 2 [1–3] days, P < 0.001) between admission and operation and a longer duration following the discontinuation of antithrombotic drugs (7 days vs. 1 [0–3] days, P < 0.001) (Table 1).
There was no significant difference in hemoglobin, platelet count, international normalized ratio, CRP, bilirubin, amylase, or lipase level between the 2 groups. However, WBC counts was more higher in emergent LC group, significantly (10,210 [6,510–13,570] vs. 14,840 [9,130–17,620], P = 0.024) (Table 1).
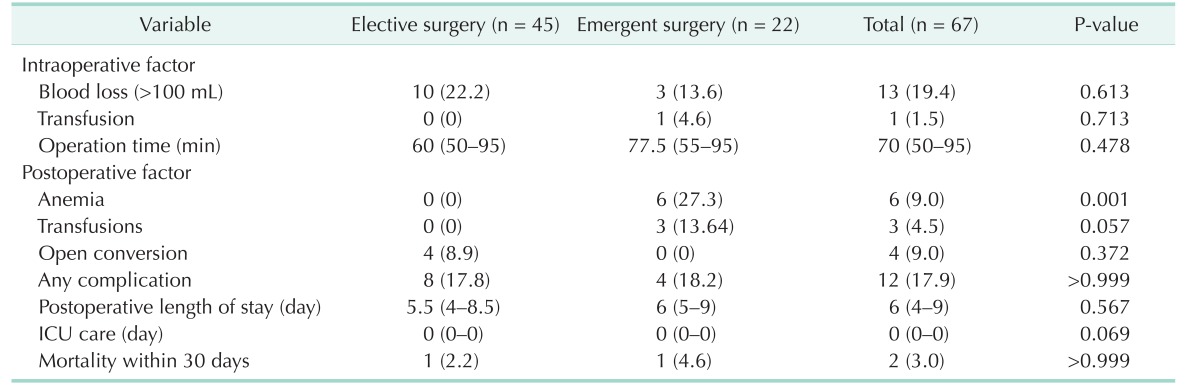
We compared the outcomes between the 2 groups (Table 2). There was no significant difference in intraoperative blood loss, intraoperative transfusion, mean operation time, open conversion rate, rate of in-hospital complication, length of postoperative stay, or length of ICU stay between the 2 groups. Six patients in the emergent LC group developed postoperative anemia while no patient in the elective LC group developed this (P = 0.001). Three of the 6 patients received packed RBC transfusion in postoperative period. Postoperative complication rates were not significantly different between 2 groups (8 patients [17.8%] vs. 4 patients [18.2%], P > 0.999); 3 pulmonary complications, 2 cardiac complications, 1 wound infection and 2 biliary complications in the elective group; 2 pulmonary complications, 1 cardiac complication, and 1 voiding difficulty in the emergent group. Mortality rates were not significantly different between the 2 groups (1 patient [2.2%] vs. 1 patient [4.6%], P > 0.999). The 2 deaths were related to the comorbidities of the 2 patients; The death in the elective group occurred in a male 84-year-old patient who received percutaneous coronary intervention for coronary 3 vessels disease, which was diagnosed in preoperative evaluation. The caridologist recommended the patient continue taking aspirin, stop taking clopidogrel 5 days before surgery and restart within 24 hours after surgery. This regimen was employed. However, the patient's cardiac problems greatly aggravated during the postoperative period and he expired 30 days after surgery due to cardiogenic shock. The death in the emergency group occurred in a male 95-year-old patient who expired 15 days after surgery due to pulmonary complications and septic shock.
Up to date, comparative studies on whether medication should be continued in patients with AC who undergo LC while on antiplatelet therapy have been rarely conducted [110]. In particular, a few study has compared the outcomes of scheduled LC and emergent LC in patients with AC while on antithrombotic therapy. Most surgeons follow the recommendation to suspend medications for a minimum of 5 days [11] in case of anticoagulants and a minimum of 7–10 days [12] in case of antiplatelet drugs considering the half-life of medication and decaying of anticoagulants in general because the intake of antithrombotic agent can increase perioperative bleeding risk [6]. However, in minor surgeries e.g., procedures with lower bleeding risk, it has been reported that there is no significant difference even if antithrombotic agent is not suspended [13141516]. In addition, significantly lower incidences of myocardial infarction in patients with high risk of cardiovascular events who have undergone noncardiac surgeries have been reported when the intake of aspirin is continued [17]. As a result, it has been recommended that the decision on suspension of medication should be made based on cardiovascular risk and bleeding risk in patients [6]. Generally, the abdominal surgery including LC has been thought to have intermediate risk among all types of surgeries [14].
Antiplatelet therapy is known to be the most effective treatment that can prevent primary and secondary cardiovascular events up to date. Therefore, high risk patients of potential cardiovascular or cerebrovascular events are advised to take antiplatelet drugs for a lifetime. If the intake of antiplatelet drug is discontinued in patients with very high risk of potential cardiovascular complications, the incidence rates of myocardial infarction, stent thrombosis, cerebral strokes, and the mortality rate in coronary stenting have been reported to increase by 45% [18]. In case of aspirin, such development is explained as a rebound phenomenon from a sudden suspension of the medication before surgery to increase thromboxane A2 activity while reducing fibrinolysis. In addition, the surgery itself can cause thrombosis by increasing the pro-thrombotic state [17]. In our study, postoperative cardiac complication was found in 1 patient who underwent delayed LC for AC after stopping the antiplatelet drug. The patient was receiving a dual antiplatelet therapy for coronary vessel disease. Although the patient underwent delayed LC after PTGBD insertion while taking aspirin, the patient died of cardiogenic shock due to postoperative ST-segment elevation myocardial infarction.
If emergent LC for patients with AC should be performed while maintaining antiplatelet drugs, the possibility of hemorrhagic complication should be kept in mind [1920]. In our study, when the period of medication suspension was not sufficient enough and emergent LC was performed in patients who were on antithrombotic therapy, significantly more incidences of postoperative anemia was found. However, the actual intraoperative blood loss did not show any difference. In addition, there was no significant difference in postoperative complication, length of stays, length of ICU stays, or mortality between the 2 groups. These results indicated that postoperative anemia did not have any effect on operative outcomes. Patients could be controlled without any invasive procedures such as reoperation and angiography. According to some recent reports, when surgery is performed in the high risk group of patients with potentially high cardiovascular adverse effects without interruption to antithrombotic therapy, the incidence rate of hemorrhagic complication is higher or similar whereas morbidity and mortality are not significantly different [1018]. In another study, it was reported that the aspirin group who underwent noncardiac surgery without interruption of medication showed higher incidence rate of bleeding complication based on a meta-analysis [21]. In our study, there was no significant difference in the severity of bleeding complication or mortality due to such complication.
Delayed LC in patients with AC needs additional pain management and PTGBD. It can lead to possible rehospitalization after discharge. Several studies have recently showed that there is no significant difference in postoperative complication, conversion rate, operating time, and postoperative analgesic requirements [234]. It is well known that early LC can reduce the length of total hospital stay. Early LC is likely to become a cost effective approach [234]. In our study, the elective LC group also showed significantly higher PTGBD insertion rates with significantly longer time from admission to operation without any significant difference in the length of postoperative hospital stays. To reduce cost caused by the increases in the time of the pain and in the length of hospital stay, performing surgery while maintaining antiplatelet agent therapy would be more effective if there is no significantly more incidence of perioperative complications.
In conclusion, our study showed that performing emergent LC without interruption to antithrombotic therapy was relatively safe and useful. Nevertheless, this study had limitations. It was a single center study with a retrospective design. It did not conduct classifications of patients by risks for thromboembolic events. It did not conduct differentiation between anticoagulant therapy groups dual antiplatelet therapy group and aspirin monotherapy group. In addition, the sample size was small. Moreover, there was a lack of approaches on long-term outcomes. Therefore, a well-designed multicenter randomized controlled trial will be needed to compare the outcome of LC for AC with the suspension of antithrombotic therapy with that of LC for AC with the continuation of antithrombotic therapy.
References
1. Anderson K, Jupiter DC, Abernathy SW, Frazee RC. Should clopidogrel be discontinued before laparoscopic cholecystectomy? Am J Surg. 2014; 208:926–931. PMID: 25435299.

2. Casillas RA, Yegiyants S, Collins JC. Early laparoscopic cholecystectomy is the preferred management of acute cholecystitis. Arch Surg. 2008; 143:533–537. PMID: 18559744.

3. Kolla SB, Aggarwal S, Kumar A, Kumar R, Chumber S, Parshad R, et al. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a prospective randomized trial. Surg Endosc. 2004; 18:1323–1327. PMID: 15803229.

4. Lau H, Lo CY, Patil NG, Yuen WK. Early versus delayed-interval laparoscopic cholecystectomy for acute cholecystitis: a metaanalysis. Surg Endosc. 2006; 20:82–87. PMID: 16247580.

5. Chassot PG, Marcucci C, Delabays A, Spahn DR. Perioperative antiplatelet therapy. Am Fam Physician. 2010; 82:1484–1489. PMID: 21166368.
6. Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e326S–e350S. PMID: 22315266.
7. Homma S, Thompson JL, Pullicino PM, Levin B, Freudenberger RS, Teerlink JR, et al. Warfarin and aspirin in patients with heart failure and sinus rhythm. N Engl J Med. 2012; 366:1859–1869. PMID: 22551105.

8. Little JW, Miller CS, Henry RG, McIntosh BA. Antithrombotic agents: implications in dentistry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 93:544–551. PMID: 12075203.

9. Hansen ML, Sorensen R, Clausen MT, Fog-Petersen ML, Raunso J, Gadsboll N, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010; 170:1433–1441. PMID: 20837828.

10. Joseph B, Rawashdeh B, Aziz H, Kulvatunyou N, Pandit V, Jehangir Q, et al. An acute care surgery dilemma: emergent laparoscopic cholecystectomy in patients on aspirin therapy. Am J Surg. 2015; 209:689–694. PMID: 25064416.

11. Kovacs MJ, Kearon C, Rodger M, Anderson DR, Turpie AG, Bates SM, et al. Single-arm study of bridging therapy with low-molecular-weight heparin for patients at risk of arterial embolism who require temporary interruption of warfarin. Circulation. 2004; 110:1658–1663. PMID: 15364803.

12. Roth GJ, Majerus PW. The mechanism of the effect of aspirin on human platelets. I. Acetylation of a particulate fraction protein. J Clin Invest. 1975; 56:624–632. PMID: 1159076.

13. Mortezavi A, Hermanns T, Hefermehl LJ, Spahn DR, Seifert B, Weber D, et al. Continuous low-dose aspirin therapy in robotic-assisted laparoscopic radical prostatectomy does not increase risk of surgical hemorrhage. J Laparoendosc Adv Surg Tech A. 2013; 23:500–505. PMID: 23611162.

14. Task Force for Preoperative Cardiac Risk Assessment and Perioperative Cardiac Management in Non-cardiac Surgery. European Society of Cardiology (ESC). Poldermans D, Bax JJ, Boersma E, De Hert S, et al. Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery. Eur Heart J. 2009; 30:2769–2812. PMID: 19713421.

15. Friedland S, Soetikno R. Colonoscopy with polypectomy in anticoagulated patients. Gastrointest Endosc. 2006; 64:98–100. PMID: 16813811.

16. Marietta M, Bertesi M, Simoni L, Pozzi S, Castelli I, Cappi C, et al. A simple and safe nomogram for the management of oral anticoagulation prior to minor surgery. Clin Lab Haematol. 2003; 25:127–130. PMID: 12641617.

17. Oscarsson A, Gupta A, Fredrikson M, Jarhult J, Nystrom M, Pettersson E, et al. To continue or discontinue aspirin in the perioperative period: a randomized, controlled clinical trial. Br J Anaesth. 2010; 104:305–312. PMID: 20150346.

18. Chassot PG, Delabays A, Spahn DR. Perioperative antiplatelet therapy: the case for continuing therapy in patients at risk of myocardial infarction. Br J Anaesth. 2007; 99:316–328. PMID: 17650517.

19. Korte W, Cattaneo M, Chassot PG, Eichinger S, von Heymann C, Hofmann N, et al. Peri-operative management of antiplatelet therapy in patients with coronary artery disease: joint position paper by members of the working group on Perioperative Haemostasis of the Society on Thrombosis and Haemostasis Research (GTH), the working group on Perioperative Coagulation of the Austrian Society for Anesthesiology, Resuscitation and Intensive Care (ÖGARI) and the Working Group Thrombosis of the European Society for Cardiology (ESC). Thromb Haemost. 2011; 105:743–749. PMID: 21437351.
20. Payne DA, Hayes PD, Jones CI, Belham P, Naylor AR, Goodall AH. Combined therapy with clopidogrel and aspirin significantly increases the bleeding time through a synergistic antiplatelet action. J Vasc Surg. 2002; 35:1204–1209. PMID: 12042732.

21. Burger W, Chemnitius JM, Kneissl GD, Rucker G. Low-dose aspirin for secondary cardiovascular prevention - cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation - review and meta-analysis. J Intern Med. 2005; 257:399–414. PMID: 15836656.

Table 1
Baseline characteristics per group
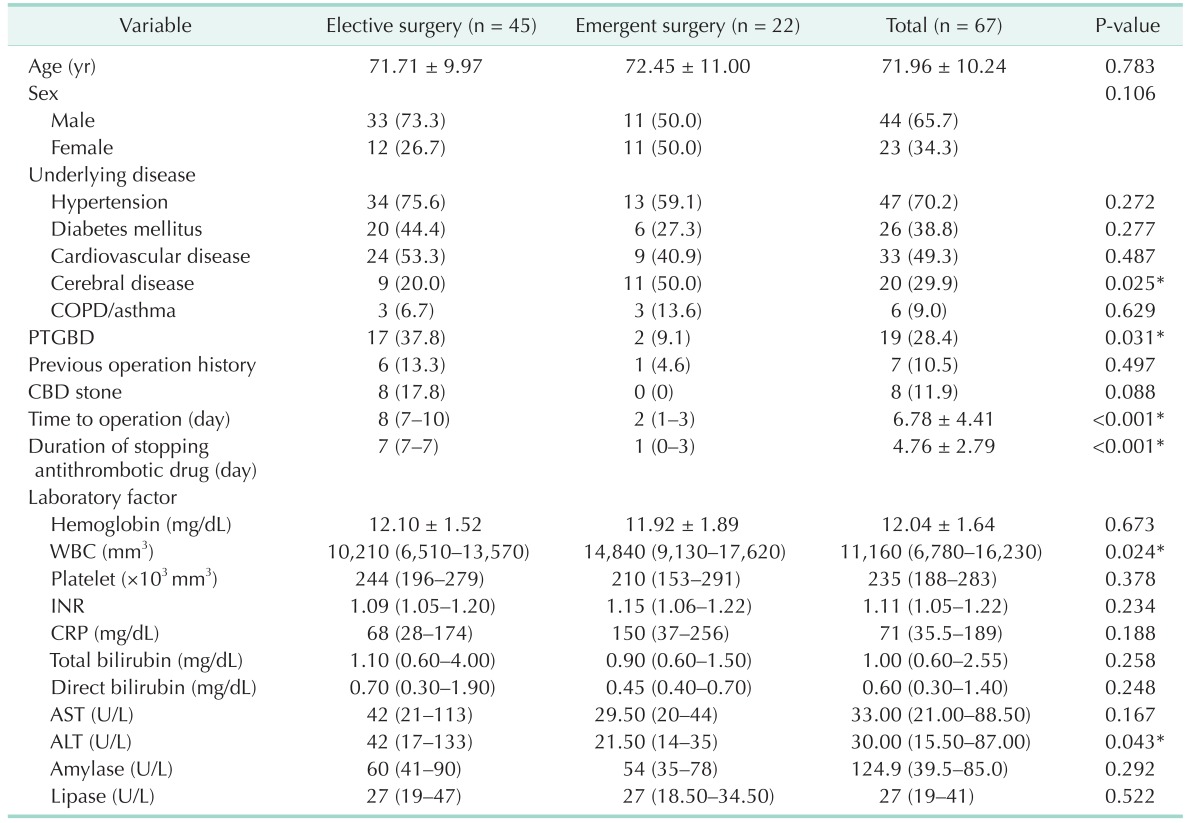
Values are presented as mean ± standard deviation, number (%), or median (interquartile range). P-values were derived by independent t-test or Mann-Whitney U-test for continuous variables and chi-square test or Fisher exact test for categorical variables as appropriate.
COPD, chronic obstructive pulmonary disease; PTGBD, percutaneous transhepatic gallbladder draninage; CBD, common bile duct; INR, international normalized ratio.
*P < 0.05, statistically significant difference.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download