Abstract
Purpose
The aim of this study was to determine whether focused or complete parathyroidectomy was more appropriate and to compare follow-up data in primary hyperparathyroidism (PHPT).
Methods
We retrospectively analyzed 225 operations for PHPT at Yonsei University Health System between 2000 and 2012. After excluding 93 patients, the remaining 132 were divided into 2 groups: those who underwent focused parathyroidectomy (FP) and those who underwent conventional parathyroidectomy (CP). We compared clinicopathological features; preoperative calcium, parathyroid hormone (PTH), phosphorus, vitamin D, 24-hour urine calcium, and alkaline phosphatase levels; postoperative calcium and PTH levels; pathologic diagnosis; multiplicity; and results of a localization study between the 2 groups.
Results
There was no significant difference in the rates of development of postoperative persistent hyperparathyroidism (1/122 FP patients and 1/10 CP patients) between the 2 groups due to a technical reason (FP 0.8% vs. CP 10.0%, P = 0.146). Multiglandular disease (MGD) was uncommon in all cases (6 of 132, 4.5%). All MGD cases were diagnosed using a preoperative localization study. Sestamibi scan and ultrasonography sensitivity were 94.2% and 90.2%, respectively.
Conclusion
We suggest that FP is appropriate in PHPT, except in cases of MGD if detected before the operation using preoperative imaging. Knowledge of hereditary PHPT and improved preoperative localization studies, such as high-resolution ultrasonography, contributed to the decision to perform FP rather than CP in all cases of unilateral results of the localizing study.
Primary hyperparathyroidism (PHPT) is the third most common endocrine disorder in the United States, with an annual incidence of 100,000 new cases [1]. In the advanced industrialized world, PHPT is detected through a screening test. Accordingly, asymptomatic hypercalcemia is more prominent than symptomatic PHPT [2]. Previously, bilateral neck exploration was considered the gold standard for the treatment of PHPT. However, with the advent of the sestamibi (MIBI) scan and radio-guided parathyroidectomy in the late 1990s, many groups advocated for a single-gland operation [3456]. Fortunately, most PHPT cases are due to single adenomas. Although focused parathyroidectomy (FP) has been the preferred treatment of PHPT, advocates of conventional parathyroidectomy (CP) have continued to debate the efficacy of CP relative to that of FP. Although in most cases a single adenoma is found, double adenomas and multiglandular disease (MGD) have been reported at rates of 4% and 14%, respectively [7]. Recently, the leading group advocating unilateral parathyroidectomy has abandoned unilateral exploration and reversed its position on CP due to the high recurrence rate (FP 5% vs. CP 0.6% at 10 years) [8].
However, the incidence of PHPT has differed according to race, with the highest rates among blacks, followed by whites, and the lowest rates among Asians (prevalence of 321 vs. 201 vs. 103 per 100,000, respectively) [9]. It has also been reported that multiple parathyroid lesions were rare in Asians when PHPT was diagnosed [91011].
In addition, we have also recognized two discrete forms, such as asynchronous and synchronous MGD [12]. Preoperative localization studies have been more successful due to the advent of sensitive imaging techniques, thus allowing predetermination of single or multiple gland involvement [13141516171819].
Consequently, we hypothesized that FP may be an operation method that offersh a high success rate in PHPT. The aim of this study was to determine whether CP or FP is appropriate and to compare follow-up data in PHPT.
This study was approved by the Yonsei University Institutional Review Board (approval number: 4-2014-0015). The need for informed consent was waived because of the retrospective nature of the study. We retrospectively analyzed 225 operations for PHPT at Yonsei University Health System between 2000 and 2012. Ninety-three cases met the exclusion criteria, and 30 cases were excluded owing to multiple endocrine neoplasm, familial isolated hyperparathyroidism, pending chronic renal failure, parathyroid cyst, or parathyroid carcinoma. Furthermore, 51 cases were excluded owing to concomitant thyroid disease requiring thyroidectomy, and 12 cases were excluded owing to an incomplete preoperative study (Fig. 1). All patients underwent preoperative ultrasonography (USG) and a MIBI scan, and all pathology-based diagnoses were confirmed histopathologically after the operation. We did not use intraoperative parathyroid hormone (PTH) monitoring. Instead, we assessed postoperative PTH levels within 2 hours after the operation. A total of 132 patients were divided into 2 groups according to the operation method: those who underwent FP (n = 122) and those who underwent CP (n = 10). The FP group included minimally invasive radio-guided parathyroidectomy and endoscopic parathyroidectomy. We compared the clinicopathological features, including symptoms and signs; preoperative calcium, PTH, phosphorus, vitamin D, 24-hour urine calcium, and ALP levels; postoperative calcium and PTH levels; pathologic diagnosis; multiplicity; and results of the localization study. Recurrence was defined as elevated calcium and PTH occurring after 6 months postoperatively. Persistence was defined as elevated calcium and PTH within 6 months postoperatively [20].
Data are expressed as mean ± standard deviation. The Fisher exact test or Pearson chi-square test was used to compare clinicopathological findings in FP and CP groups. Statistical analysis was performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA), and differences were considered significant when P-values were less than 0.05.
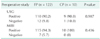
There were no differences in symptomatic characteristics between FP and CP groups (Table 1). About 60%–65% of cases were asymptomatic. Age was significantly higher in the CP group compared to that in the FP group, but there were no differences in demographic and laboratory characteristics between FP and CP groups for sex, follow-up period, presence of symptoms, preoperative serum calcium, preoperative PTH, preoperative serum phosphate and ALP levels, and preoperative bone mineral density. Operation time was shorter in the FP than that in the CP group. Our study contained a variable follow-up period, with some patients followed for almost 12 years. The mean follow-up time was about 46 months in the FP group and 59 months in the CP group (Table 2).
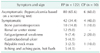
There was one failed preoperative localization using both USG and MIBI in the FP group. However, this failed localization was followed by a successful additional magnetic resonance study. Our study showed that sensitivity in detecting parathyroid lesions was 94.3% using MIBI scans and 90.2% using USG. Of the 122 patients in the FP group, only 103 patients were positive using both USG and the MIBI scan; 7 patients were positive only in the USG study, and 12 patients were positive only in the MIBI study. Therefore, almost all parathyroid lesions were localized using a combination of USG and the MIBI scan (Table 3).
There was no significant difference between the 2 groups for postoperative calcium, PTH level, or size and weight of the parathyroid specimen. A large percentage (95.5%) of all patients with PHPT had a single parathyroid lesion. MGD was uncommon in all cases (6 of 132, 4.5%). In all cases of multiple parathyroid lesions identified in the preoperative localization study, we preferred CP due to the possibility of MGD or double adenoma. However, of the 10 CP patients, four underwent CP owing to another USG-detected ambiguous parathyroid lesion that was confirmed using a frozen biopsy. In these cases, disease in only a single parathyroid gland was reported at the final pathology.
There was no significant difference in the rate of failed surgery between the 2 groups (FP 0.8% vs. CP 10.0%, P = 0.146). Postoperative persistent hyperparathyroidism developed in one FP patient and one CP patient due to technical failure. All MGD cases were diagnosed using the preoperative localization study. There was no significant difference in the sizes or weights of specimens between the 2 groups. However, the rate of hyperplasia was higher in the CP group than in the FP group (50% vs. 12.3%, P = 0.02) (Table 4).
In the 2 cases of persistent hyperparathyroidism, the postoperative PTH level exceeded the upper limit of the normal range.
A 65-year-old male (sCa 12.2 mg/dL, PTH 88.2 pg/mL) underwent right superior and left superior parathyroidectomy. Postoperatively, sCa (10.6 mg/dL) and PTH (75.2 pg/mL) were still elevated. One right superior parathyroid hyperplasia and one left superior lymph node in one CP patient were reported at the final pathology. The patient denied the proposed additional re-operation.
A 63-year-old female (sCa 11.1 mg/dL, PTH 300 pg/mL) underwent right inferior parathyroidectomy. Postoperatively, sCa (9.4 mg/dL) and PTH (151 pg/mL) were checked. One parathyroid tissue in one FP patient was reported at the final pathology. Ten months after initial operation, she was cured after resection of right inferior parathyroid adenoma.
In the 2 failed surgery cases, an additional localization study such as methionine PET-CT, selective venous sampling, or USG-guided indigo carmine tattooing was used for reoperation. After the preceding additional localization study, 2 patients had re-exploration after a previous procedure failed to locate and remove an abnormally functioning parathyroid gland. After removal of the abnormal gland, all patients became normocalcemic, and the PTH level decreased below the upper limit of the normal range.
Before advances in preoperative localization studies and intraoperative PTH analysis, bilateral exploration was considered the gold standard treatment of PHPT because of the possibility of MGD. However, with improved understanding of the disease pattern in PHPT, unilateral approaches have emerged with high cure rates. Nonetheless, Duh et al. [7] reported that unilateral exploration was associated with a risk of missing a contralateral double adenoma with or without a localization study. Despite the possibility of MGD, many groups have advocated for using a single-gland operation such as radio-guided or FP [345621]. Before the first application of minimally invasive FP in 2001, we performed 32 radio-guided parathyroidectomies beginning in 1999. Our previous initial study showed that minimally invasive radio-guided parathyroidectomy and minimally invasive FP achieved a high success rate compared with bilateral or unilateral exploration [22]. Among the 122 patients with FP who were enrolled in this study, only 9 underwent radio-guided parathyroidectomy. Accordingly, Radio-guided parathyroidectomy could not have influenced our results. This study had somewhat descriptive nature, making it difficult to identify significant differences between FP and CP. As more data have become available, there has been a gradual evolution of the operation method used to avoid recurrence. About 10 years ago, we confirmed that FP is sufficient to treat PHPT due to the advent of sensitive imaging techniques such as high-resolution USG that are used for preoperative localization studies [22].
Furthermore, the group of Norman et al. [8]—the leading group advocating unilateral parathyroidectomy—have recently abandoned this position and reversed their position toward CP. They showed that the recurrence rate after unilateral parathyroidectomy was significantly higher than that after bilateral operation. Nevertheless, it is possible that the authors might have missed false negative parathyroid lesions in the parathyroid scan, because they only used MIBI scan. Consequently, surgical controversies are more complicated in PHPT, and there was a need to confirm treatment of PHPT using long-term follow-up data. It is notable that MGD was uncommon in our study and that cure rates were as high as 98.5%, with an especially high rate of 99.2% in the FP group (Table 5).
In addition, some groups have reported that microscopically hyperplastic glands of normal size are of no clinical significance and that the removal of such glands is unnecessary [23]. After experienced surgeons inspected ambiguous parathyroid lesions in patients with MGD and double adenoma, they decided whether a frozen biopsy should be performed. Even though we used frozen biopsies to confirm pathology, some of the pathologic reports did not provide enough information to obtain a precise determination of whether the parathyroid lesion included pathological change. Although histologic differences between adenomas and hyperplastic glands have been proposed, the diagnosis of single-gland disease versus four-gland hyperplasia has traditionally been made using a combination of gross surgical and histologic findings. On the other hand, a Wisconsin group suggested that parathyroid gland weight helps to predict the likelihood of an additional hyperfunctioning parathyroid gland [24]. In this regard, high-resolution USG is very useful and can supplement MIBI scans, which do not precisely measure parathyroid size. Elaraj et al. [25] suggested additional imaging using neck USG is helpful for selecting minimally invasive parathyroidectomy in most patients with PHPT who have negative MIBI scan results. We decided to perform FP in both of the following situations: when USG and MIBI scan findings were discordant in unilateral location, and when there was single positive lesion on both the USG and MIBI scan. However, when USG and MIBI scan findings were discordant in bilateral location, we decided to perform CP. Our results showed that USG is useful when MIBI scans are negative and that it may also be useful when tattooing a parathyroid lesion in failed surgery.
Nonetheless, reoperation for recurrent PHPT was associated with higher failure rates and complications, especially in CP cases. The occurrence of asynchronous MGD has been reported after an initially successful operation. Worsey et al. [12] reported an average recurrent-free period of 3.8 years after a successful operation with 15 years of follow-up. Because of the possibility of asynchronous MGD, using FP to avoid unnecessary dissection is more beneficial than CP in recurrent cases. Patients who are not cured after such an approach are able to undergo a simple, noncomplex, second operation that is performed in naïve tissues [8].
Our study has limitations. First, the follow-up period for this series was different for each patient (6–160 months). In addition, the incidence of PHPT in Korea is lower than in America and Europe. Moreover, we did not use intraoperative PTH monitoring; instead, we checked postoperative PTH within 2 hours postoperatively. In spite of these limitations, we have previously reported that there was a gradual evolution of the operation method used to avoid recurrence at our institution over about 24 years [22].
Ning et al. reported that elevated PTH after successful parathyroidectomy for PHPT is not associated with recurrent hyperparathyroidism [2627]. Many studies have reported that intraoperative PTH monitoring is useful in successful parathyroidectomy for PHPT [2829]. In some cases, intraoperative PTH monitoring is thought to confuse the decision-making process [2730]. Furthermore, undetected hyperplastic glands of normal size in the preoperative imaging study are of no clinical significance, and the removal of such glands is unnecessary [23].
In conclusion, FP is appropriate in cases of a single lesion confirmed preoperatively. Consequently, we suggest FP is more appropriate than CP for PHPT, except for cases in which MGD is detected in the preoperative imaging study. Improved preoperative localization studies such as high-resolution USG and additional knowledge regarding hereditary PHPT may help to determine whether FP or CP should be performed for all cases in which the localization study has unilateral results.
Figures and Tables
Fig. 1
Characteristics of the cases excluded. PHPT, primary hyperparathyroidism; CRF, chronic renal failure; MEN, multiple endocrine neoplasia; HPT, hyperparathyroidism; MIBI, sestamibi; USG, ultrasonography.
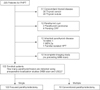
Table 2
Preoperative demographics and clinical data between focused parathyroidectomy and conventional parathyroidectomy groups

Values are presented as mean ± standard deviation or number (%).
Reference values for our institution: calcium, 8.6–10.6 mg/dL; PTH, 15–65 pg/mL; phosphorus, 2.3–4.5 mg/dL; vitamin D (25(OH)D), >30 ng/mL; ALP, 120–360 IU/L; 24-hr urine calcium, 50–200 mg/day.
FP, focused parathyroidectomy; CP, conventional parathyroidectomy; PTH, parathyroid hormone; BMD, bone mineral density (T-score from L-spine).
Table 3
Comparison of preoperative localization studies between focused parathyroidectomy and conventional parathyroidectomy groups
References
1. Adler JT, Sippel RS, Chen H. New trends in parathyroid surgery. Curr Probl Surg. 2010; 47:958–1017.
2. Macfarlane DP, Yu N, Donnan PT, Leese GP. Should 'mild primary hyperparathyroidism' be reclassified as 'insidious': is it time to reconsider? Clin Endocrinol (Oxf). 2011; 75:730–737.
3. Chen H, Sokoll LJ, Udelsman R. Outpatient minimally invasive parathyroidectomy: a combination of sestamibi-SPECT localization, cervical block anesthesia, and intraoperative parathyroid hormone assay. Surgery. 1999; 126:1016–1021.
4. Flynn MB, Bumpous JM, Schill K, McMasters KM. Minimally invasive radioguided parathyroidectomy. J Am Coll Surg. 2000; 191:24–31.
5. Nagar S, Reid D, Czako P, Long G, Shanley C. Outcomes analysis of intraoperative adjuncts during minimally invasive parathyroidectomy for primary hyperparathyroidism. Am J Surg. 2012; 203:177–181.
6. Norman J, Politz D. Prospective study in 3,000 consecutive parathyroid operations demonstrates 18 objective factors that influence the decision for unilateral versus bilateral surgical approach. J Am Coll Surg. 2010; 211:244–249.
7. Duh QY, Uden P, Clark OH. Unilateral neck exploration for primary hyperparathyroidism: analysis of a controversy using a mathematical model. World J Surg. 1992; 16:654–661.
8. Norman J, Lopez J, Politz D. Abandoning unilateral parathyroidectomy: why we reversed our position after 15,000 parathyroid operations. J Am Coll Surg. 2012; 214:260–269.
9. Yeh MW, Ituarte PH, Zhou HC, Nishimoto S, Liu IL, Harari A, et al. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab. 2013; 98:1122–1129.
10. Lee SH, Hong SJ. Minimally invasive parathyroidectomy without an Intraoperative i-PTH test for patients with primary hyperparathyroidism. J Korean Surg Soc. 2008; 75:9–14.
11. Lo CY, Lang BH, Chan WF, Kung AW, Lam KS. A prospective evaluation of preoperative localization by technetium-99m sestamibi scintigraphy and ultrasonography in primary hyperparathyroidism. Am J Surg. 2007; 193:155–159.
12. Worsey MJ, Carty SE, Watson CG. Success of unilateral neck exploration for sporadic primary hyperparathyroidism. Surgery. 1993; 114:1024–1029.
13. Mihai R, Simon D, Hellman P. Imaging for primary hyperparathyroidism--an evidence-based analysis. Langenbecks Arch Surg. 2009; 394:765–784.
14. Agcaoglu O, Aliyev S, Heiden K, Neumann D, Milas M, Mitchell J, et al. A new classification of positive sestamibi and ultrasound scans in parathyroid localization. World J Surg. 2012; 36:2516–2521.
15. Akram K, Parker JA, Donohoe K, Kolodny G. Role of single photon emission computed tomography/computed tomography in localization of ectopic parathyroid adenoma: a pictorial case series and review of the current literature. Clin Nucl Med. 2009; 34:500–502.
16. Rodgers SE, Hunter GJ, Hamberg LM, Schellingerhout D, Doherty DB, Ayers GD, et al. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006; 140:932–940.
17. Alexandrides TK, Kouloubi K, Vagenakis AG, Yarmenitis S, Spyridonidis T, Vassilakos P, et al. The value of scintigraphy and ultrasonography in the preoperative localization of parathyroid glands in patients with primary hyperparathyroidism and concomitant thyroid disease. Hormones (Athens). 2006; 5:42–51.
18. Gill MT, Dean M, Karr J, Aultman DF, Nathan CO. Intraoperative parathyroid hormone assay: a necessary tool for multi-glandular disease. Otolaryngol Head Neck Surg. 2011; 144:691–697.
19. Yip L, Pryma DA, Yim JH, Virji MA, Carty SE, Ogilvie JB. Can a lightbulb sestamibi SPECT accurately predict single-gland disease in sporadic primary hyperparathyroidism? World J Surg. 2008; 32:784–792.
20. Wirowski D, Goretzki PE, Schwarz K, Lammers BJ, Dotzenrath C, Roher HD. Failed surgery in primary hyperparathyroidism: what has changed with time. Exp Clin Endocrinol Diabetes. 2013; 121:323–328.
21. Udelsman R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg. 2002; 235:665–670.
22. Yoon JH, Chang HS, Park CS. Surgical strategy in the management of primary hyperparathyroidism. J Korean Surg Soc. 2004; 66:372–378.
23. Harrison TS, Duarte B, Reitz RE, Princenthal R, Seaton JF, Badder EM, et al. Primary hyperparathyroidism: four-to eight-year postoperative follow-up demonstrating persistent functional insignificance of microscopic parathyroid hyperplasia and decreased autonomy of parathyroid hormone release. Ann Surg. 1981; 194:429–437.
24. Mazeh H, Chen H, Leverson G, Sippel RS. Creation of a "Wisconsin index" nomogram to predict the likelihood of additional hyperfunctioning parathyroid glands during parathyroidectomy. Ann Surg. 2013; 257:138–141.
25. Elaraj DM, Sippel RS, Lindsay S, Sansano I, Duh QY, Clark OH, et al. Are additional localization studies and referral indicated for patients with primary hyperparathyroidism who have negative sestamibi scan results? Arch Surg. 2010; 145:578–581.
26. Ning L, Sippel R, Schaefer S, Chen H. What is the clinical significance of an elevated parathyroid hormone level after curative surgery for primary hyperparathyroidism? Ann Surg. 2009; 249:469–472.
27. Carneiro DM, Solorzano CC, Nader MC, Ramirez M, Irvin GL 3rd. Comparison of intraoperative iPTH assay (QPTH) criteria in guiding parathyroidectomy: which criterion is the most accurate? Surgery. 2003; 134:973–979.
28. Day KM, Elsayed M, Monchik JM. No need to abandon focused unilateral exploration for primary hyperparathyroidism with intraoperative monitoring of intact parathyroid hormone. J Am Coll Surg. 2015; 221:518–523.
29. Kim HG, Kim WY, Woo SU, Lee JB, Lee YM. Minimally invasive parathyroidectomy with or without intraoperative parathyroid hormone for primary hyperparathyroidism. Ann Surg Treat Res. 2015; 89:111–116.
30. Miura D, Wada N, Arici C, Morita E, Duh QY, Clark OH. Does intraoperative quick parathyroid hormone assay improve the results of parathyroidectomy? World J Surg. 2002; 26:926–930.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download