Abstract
Traumatic splenic vein aneurysm (SVA) is an extremely rare entity. Traditionally, treatment varied from noninvasive followup to aneurysm excision with splenectomy. However, there has been no prior report of traumatic SVA treated with endovascular stent graft for SVA via percutaneous transsplenic access. Therefore, we report the case of a 56-year-old man successfully treated with endovascular stent graft for traumatic SVA via percutaneous transsplenic access.
Splenic vein aneurysm (SVA) is extremely rare, and may be congenital, traumatic, or contracted through infection [1234]. Various treatments such as conservative, surgical, or endovascular treatments have been attempted. However, none of these have been clearly established yet [56]. In this case report, we present the first case of successful treatment with endovascular stent graft via percutaneous transsplenic access for a patient who sustained a traumatic SVA.
A 56-year-old man was brought to a level I trauma center after a motorcycle collision. Upon arrival at the Emergency Department, his blood pressure was 100/70 mmHg, and pulse rate was 83 beats/min and regular. The patient complained of chest wall pain, dyspnea, and epigastric pain.
A focused abdominal sonogram demonstrated a small amount of fluid collection in the perisplenic space. CT of the chest, abdomen, and pelvis with contrast demonstrated multiple bilateral rib fractures, hemo-pneumothorax, grade II liver laceration, grade II splenic laceration, and 22 × 18-mm-sized aneurysm-like dilated splenic vein with adjacent high attenuated fluid collection (Fig. 1). Because of the aneurysm-like dilated splenic vein with adjacent high attenuated fluid collection, the trauma team recommended angiographic evaluation of his splenic vascular injury status.
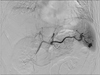
Arterial access was obtained via the right common femoral artery using standard technique. Selective splenic arteriography demonstrated injury to a branch supplying the lower pole of the spleen (Fig. 2). This vessel was selectively embolized using glue-lipiosol mixture (1:2 ratio by volume). Splenic arteriography failed to demonstrate any arteriovenous fistula or arterial pseudoaneurysm to account for the aneurysm-like dilated splenic vein visualized on CT.
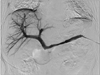
Then, percutaneous transsplenic access was done for venous injury evaluation. A 22-guage needle was used to puncture the skin and target the location of an intrasplenic vein branch. After the splenic vein branch was successfully punctured, a 0.018-inch guide wire was introduced into the splenic vein through the needle. The needle was exchanged by a 4-Fr coaxial dilator and a 5-Fr sheath, and the 0.018-inch guide wire was replaced with a 0.035-inch angled hydrophilic guide wire (Terumo, Tokyo, Japan). Subsequently, a 5-Fr catheter (Cook Inc., Bloomington, IN, USA) was introduced into the splenic vein via the 0.035-inch guide wire. A transcatheter venography procedure was performed using the catheter sheath, which demonstrated a SVA visualized on the conventional CT, with extravasation of contrast to the peritoneal cavity (Fig. 3). The catheter was exchanged by a long 9-Fr catheter. After administration of intravenous heparin (2,000 U), on the basis of CT and venography measurements, a 9-mm × 5-cm Viabahn stent (W. L. Gore and Associates, Flagstaff, AZ, USA) was deployed across the area of injury. Venography demonstrated a patent splenic vein without filling of the aneurysm or extravasation to the peritoneal cavity (Fig. 4). Following the endovascular treatment, the transsplenic tract was plugged with 8-mm × 14-cm Nester coil and glue-lipiosol mixture (1:2 ratio by volume).
After this procedure, the patient was treated for coexisting injuries. At 14 days after the procedure, the patient stabilized and there was no evidence of bleeding, so we started the patient on antiplatelet treatment of aspirin (100 mg every 12 hours) and clopidogrel (75 mg every 12 hours). The patient was then discharged on day 32 without any complications. The antiplatelet treatment was continued for three months without any complications.
Portal system aneurysms including SVA can be divided into 2 types: extrahepatic and intrahepatic. SVA is a true aneurysm and belongs to the extrahepatic portal venous system category [6]. In 1953, Lowenthal and Jacob (quoted from [7]) first described a case of SVA. Since then, about only 10 SVA cases have been reported.
Like most abdominal venous aneurysm, SVAs are found incidentally. Ultrasonography, color Doppler ultrasound, CT, magnetic resonance imaging, and even angiography were used to make the diagnosis of an SVA. In this case, we incidentally diagnosed the SVA with CT and angiography during trauma patient evaluation.
Because SVA is an extremely rare condition, the type and timing of treatment are controversial and unclear. Although SVA has a risk of bleeding and thrombosis, many authors preferred to follow-up by serial radiological studies without any surgical intervention [28]. In this case, an endovascular stent graft via percutaneous transsplenic access was performed to resolve the SVA with extravasation to the peritoneal cavity.
Percutaneous transsplenic access is a way of approaching the portal vein including splenic vein. However, because of the high vascularity of the spleen, interventional radiologists are particularly concerned with the risk of bleeding, which is a serious complication associated with the technique. At present, percutaneous transsplenic intervention is rarely performed by clinicians. To prevent or minimize bleeding from the splenic puncture tract, a recently published study suggested plugging the puncture tract with a glue-lipiodol mixture, which is especially useful in patients who require a larger catheter sheath [9]. In this case, not only glue-lipiodol mixture was used for plugging, but also an 8-mm × 14-cm Nester coil was used to prevent bleeding from the splenic puncture tract.
Endovascular stenting intervention for polytrauma patients creates the dilemma of whether to anticoagulate, and if so, to what extent. There is a paucity of literature on this topic, and there are no established guidelines, particularly in regards to venous setting. A recent review of stents placed in the setting of carotid injury showed promising results for patency after a regimen of antiplatelet therapy [10]. However, these data are difficult to extrapolate to the venous system or in cases such as this. In this case, the patient was initially maintained with anticoagulation by intravenous heparin because of presumed risk of bleeding from other injuries from trauma. The patient was transitioned to and maintained on aspirin and Plavix.
In conclusion, this is the first report of percutaneous transsplenic splenic venous stent for SVA and demonstrates the usefulness of percutaneous transsplenic splenic venous stent as a selective option to treat an SVA. Although the ultimate durability of this intervention remains unknown, findings at short-term follow-up have been encouraging.
Figures and Tables
Fig. 1
The initial CT demonstrated grade II liver laceration, splenic laceration and 22 × 18-mm-sized aneurysm-like dilated splenic vein (white arrow) with adjacent high attenuated fluid collection.
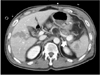
Fig. 2
Selective splenic arteriography demonstrated pseudoaneurysm (black arrow) to a branch supplying the lower pole of the spleen.
References
1. Hamed Ibrahim W, M Bassurrah H. Endovascular management of splenic arteriovenous fistula with giant venous aneurysmal dilatation. Ann Vasc Dis. 2012; 5:439–444.
2. Shimoda M, Kubota K, Sakuma A, Hogami T, Yamaguchi H, Tagaya N. Intra-abdominal hemorrhage due to rupture of a splenic vein aneurysm: a case report. J Gastrointest Surg. 2003; 7:683–686.
3. Soo MS, Khoury MB, Lupetin AR. Splenic vein aneurysm: MR appearance--a case report. Angiology. 1991; 42:590–593.
4. Bonington SC, Hodgson DI, Mehta S, Lynch N, Chalmers N. A congenital venous anomaly, with a portal-systemic shunt into a previously undescribed intrathoracic vein. Clin Radiol. 2002; 57:658–660.
5. Calligaro KD, Ahmad S, Dandora R, Dougherty MJ, Savarese RP, Doerr KJ, et al. Venous aneurysms: surgical indications and review of the literature. Surgery. 1995; 117:1–6.
6. Torres G, Hines GL, Monteleone F, Hon M, Diel J. Splenic vein aneurysm: is it a surgical indication? J Vasc Surg. 1999; 29:719–721.
7. Comert M, Erdem LO, Ozdolap S, Erdem CZ, Sarikaya S. Splenic vein aneurysm demonstrated by magnetic resonance angiography. Dig Dis Sci. 2005; 50:1344–1346.
8. Tolgonay G, Ozbek SS, Oniz H, Suzer E, Yurdakul LO. Regression of splenic vein aneurysm following resolution of splenomegaly. J Clin Ultrasound. 1998; 26:98–102.
9. Zhu K, Meng X, Zhou B, Qian J, Huang W, Deng M, et al. Percutaneous transsplenic portal vein catheterization: technical procedures, safety, and clinical applications. J Vasc Interv Radiol. 2013; 24:518–527.
10. Edwards NM, Fabian TC, Claridge JA, Timmons SD, Fischer PE, Croce MA. Antithrombotic therapy and endovascular stents are effective treatment for blunt carotid injuries: results from longterm followup. J Am Coll Surg. 2007; 204:1007–1013.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download