Abstract
Purpose
Methods
Results
Conclusion
Figures and Tables
Fig. 1
View of posterior radical antegrade modular pancreatosplenectomy after the completion of the resection stage. The range of lymph node dissection included the lymphoid tissues upwards to the diaphragmatic crus, downwards to the left renal vein and the left lateral portion of the aorta on the posterior side.

Fig. 2
A Kaplan-Meier survival curve of radical antegrade modular pancreatosplenectomy (RAMP) and distal pancreatectomy in all pancreas ductal adenocarcinoma (PDAC) cases (n = 43) and in PDAC cases without nodal invasion (n = 23); disease-free survival (A, C) and overall survival rate (B, D).
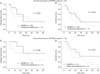
Table 1
Patient demographics and perioperative outcomes

Values are presented as mean ± standard deviation or number (%).
RAMPS, radical antegrade modular pancreatosplenectomy; DP, distal pancreatectomy; ASA, American Society of Anesthesiologists; POD, postoperative day; ICU, intensive care unit; POPF, postoperative pancreatic fistul.
a)Estimated by visual analog scale. b)System of grading complications by DeOliveira et al. [10]. In this system, grade I complications require antipyretics, diuretics or basic monitoring without pharmacologic treatment, surgical, endoscopic, and radiological interventions. Grade II complications require pharmacologic treatment with blood transfusion, total parenteral nutrition or drugs such as intravenous medications. Grade III complications require surgical, endoscopic, or radiologic intervention. Grade IV complications are life-threatening complications including organ dysfunction or central nervous system complications requiring ICU management. Grade V complications result in death. c)In the system of grading complications by DeOliveira et al. [10], grades 1 and 2 are considered as minor and grades 3 to 5 are defined as major complications.
Table 2
Oncologic outcome and survival analysis

Values are presented as number (%) or mean ± standard deviation.
RAMPS, radical antegrade modular pancreatosplenectomy; DP, distal pancreatectomy.
a)Two patients who had neuroendocrine carcinoma and two who had metastatic renal cell carcinoma were excluded in this analysis. b)Two patients who had neuroendocrine carcinoma were excluded in this analysis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download