Abstract
Purpose
The objective of this study was to review the clinical outcome and prognosis of patients with sporadic and hereditary medullary thyroid cancer (MTC) who were treated at a single tertiary hospital in Korea.
Methods
We retrospectively reviewed the case files of 85 patients treated from August 1982 to February 2012.
Results
In all, 65 patients (76.5%) had sporadic MTC and 20 patients (23.5%) had hereditary MTC. Patients in the sporadic group were older than in the hereditary group (P < 0.001). However, the hereditary group had more tumor multiplicity (P < 0.001) and bilaterality (P < 0.001). Neither survival rate was significantly different between the sporadic and hereditary groups (P = 0.775 and P = 0.866). By multivariate analysis, distant metastasis was a significant prognostic factor for overall and progression-free survival.
Medullary thyroid carcinoma (MTC) is a rare endocrine tumor that accounts for 5%–8% of all thyroid carcinomas but represents up to 13.4% of thyroid cancer-related deaths. MTC derives from calcitonin-producing parafollicular C cells of the thyroid gland [12] and occurs as a sporadic tumor in about 75%–80% of those treated and as a hereditary tumor in others (20%–25%) [3]. Hereditary MTC is termed multiple endocrine neoplasia syndrome (MEN 2A and 2B) [4]. The 10-year disease-specific survival rate of MTC is about 75%. The tumor metastasizes early to both paratracheal and lateral cervical lymph nodes, and distant metastases occur in the liver, lungs, bones, and less frequently in brain and skin. Systemic chemotherapy and external radiotherapy are of limited efficacy [56].
A high serum calcitonin (Ct) level is a highly sensitive and specific tumor marker for postsurgical follow-up of MTC patients after total thyroidectomy. However, in more advanced tumors, which may dedifferentiated by decreased Ct production, CEA may be a more valuable tumor marker [7]. Other important prognostic factors for adverse outcome include advanced age at diagnosis, extent of primary tumor, and nodal metastasis and distant metastases [8].
Germ-line point mutations in the RET proto-oncogene are responsible for tumor growth and for the heritage setting of MEN 2A and 2B [910]. RET proto-oncogene mutations of activation strength enable risk stratification and may be used to individualize treatment plans [8]. To enable early diagnosis and treatment, all family members of patients confirmed to have MTC should undergo genetic screening.
This study evaluated the long-term outcomes of surgically treated patients with histopathologically confirmed MTC at a single institution of Korea and compared outcomes in patients with hereditary and sporadic MTC. The results of RET proto-oncogene mutation analysis suggest another valid screening method for MTC.
We retrospectively reviewed the medical records of consecutive patients undergoing surgical intervention for MTC. The patients were found to have suspicious thyroid nodules after palpable neck mass evaluation, medical examination without any symptom, and detection of RET proto-oncogene mutation with thyroid nodules during screening evaluation as a relative of MTC patients. Data were retrieved through a thyroid cancer database at Severance Hospital and follow-up information was obtained through medical record review. The study protocol was approved by Severance Hospital Review Board. We analyzed clinical histories, biochemical evaluations, and histopathology, surgical, and other therapeutic data as well as long-term outcomes. Medical histories and RET proto-oncogene mutation analyses were reviewed to determine if the disease was sporadic or hereditary. Hereditary MTC was identified on the basis of findings of RET proto-oncogene mutation and MEN2 syndrome. For identification of relevant RET proto-oncogene mutations, blood was collected in ethylenediaminetetraacetic acid from all subjects. Genomic DNA was purified from peripheral blood lymphocytes. The RET proto-oncogene gene exons 10, 11, 13, 14, 15, and 16 were analyzed in all index cases using polymerase chain reaction and sequencing. Whenever the diagnosed RET proto-oncogene point mutation created or deleted the recognition site of a restriction enzyme, we performed restriction analysis of the mutated exon to confirm the presence of RET proto-oncogene mutation.
Patients were regarded as having MEN 2A if at least one family member had hyperparathyroidism or pheochromocytoma and the specific RET proto-oncogene mutation. MEN 2A syndrome can be classified as four variants: (1) Classical MEN2A is the most common MEN2A variant in which all patients develop MTC, and lower numbers develop pheochromocytoma or hyperparathyroidism; (2) MEN2A and cutaneous lichen amyloidosis is a rare disorder; (3) MEM2A and Hirschsprung disease (HD) is the third variant; (4) familial medullary thyroid carcinoma (FMTC) is the fourth variant that is characterized by the presence of an RET proto-oncogene germline mutation in families with MTC (or single individuals with MTC and no family history of MTC) who develop neither pheochromocytoma nor hyperparathyroidism [4]. Likewise, MEN 2B is considered if one or more family member had morphological characteristics of the disease with pheochromocytoma and RET proto-oncogene mutation. Sporadic cases were defined as patients without pheochromocytoma or hyperparathyroidism and no family history of MTC. The diagnosis of MTC was based on high serum Ct levels either with positive biopsy or fine needle aspiration, thyroid nodules and cervical lymphadenopathy, or distant metastases. Diagnosis was confirmed by surgical histological results. After surgical treatment, we performed regular postoperative workups that consisted of at least 6 monthly reviews with physical examination, measurement of serum Ct and CEA levels, and radiological examination (neck ultrasonography, CT, and PET-CT scan). The cohort patients were followed until death or the closing date of the study.
Disease recurrence of local area was defined as new evidence of MTC by radiologically and pathologically proven techniques after successful tumor resection. And, the patients were regarded to be in biochemical disease (BCD) if Ct levels increased to the normal range and there was no imaging evidence of residual disease at the last follow-up. The normal reference value of Ct in our institution is <10 pg/mL. Clinical disease (CD) was divided as stable disease (SD) and progressive disease (PD). At the last follow-up, if there was disease remaining without much change from pretreatment conditions—it was defined as SD. And if the disease showed more than a slight increase in size or extent on or after treatment—it was defined as PD. Progression-free survival was counted from the time of the initial surgery to the first evidence of recurrence or disease progression.
We used simple summary statistics to describe the demographic and clinical data, and chi-square and Student t-tests for categorical and continuous variable comparisons. Survival was estimated by using the Kaplan-Meier method and survival curves were compared with the log-rank test using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). P-values less than 0.05 were considered statistically significant.
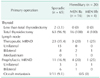
Between January 1982 and February 2012, 141 patients underwent thyroid surgery for treatment of MTC at our institution. Of these, except in the case of lost follow-up and not conducting RET proto-oncogene mutation analysis, 85 patients were available for this study. The mean age of the 85 patients studied was 46.2 years (range, 12 to 80 years). There were 32 male and 53 female patients. We considered 65 patients (76.5%) to have sporadic MTC. In the remaining 20 patients, MTC was a manifestation of either MEN 2A (16 patients) or MEN 2B (4 patients) syndromes. The mean age of patients in the sporadic group was higher than in the hereditary group (50.1 years vs. 29.9 years, P < 0.001). The male to female ratio of the 2 groups was not significantly different (1/1.6 vs. 1/2.14, P = 0.499). The RET proto-oncogene mutation was diagnosed in 6 patients (9.2%) in the sporadic group and in all patients in the hereditary group. Mean tumor size was similar in both groups. (1.68 cm vs. 2.15 cm, P = 0.223). Tumor multiplicity and tumor bilaterality were higher in the hereditary group than in the sporadic group (73.7% vs. 15.4%, P < 0.001, and 78.9% vs. 13.8%, P < 0.001). Extracapsular invasion was similar in both groups (41.5% vs. 40.0%, P > 0.05). Mean serum Ct level at presentation were 1,056.44 ± 2,454.13 pg/mL in sporadic group and 712.22 ± 1,536.37 pg/mL in hereditary group (P = 0.493). Mean CEA levels at presentation were similar in sporadic group (110.71 ± 530.39 ng/mL) and in hereditary group (290.63 ±869.40 ng/mL) (P = 0.303). By the American Joint Committee on cancer 7th edition TNM staging system, staging distributions for the sporadic and hereditary groups were similar (P = 0.580) (Table 1).
Surgical procedures were not uniform. Nearly all patients (97.4%, 83 of 85) underwent total thyroidectomy at initial surgery. However, 2 patients had less than total thyroidectomy (One patient had thyroid lobectomy for a large benign tumor and concurrently pathologically proven occult MTC. The other patient had thyroid lobectomy for papillary thyroid microcarcinoma but permanent pathology report was changed to MTC) and we planned to do no additional completion thyroidectomy with the consent of patients.
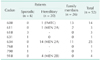
A total of 84 patients received central compartment lymph node dissection except 1 patient who underwent thyroid lobectomy for a large benign tumor and concurrently proven occult MTC. In all, 27 patients (31.8%) had modified radical neck dissection (MRND) to remove metastatic lymph nodes. Another 16 underwent MRND for prophylactic cure of lateral neck node metastases; however, 1 patient (9.1%, 1 of 11) in the sporadic group had occult lateral lymph node metastases (Table 2).
Mean follow-up period was 76.3 ± 57.0 months (range, 8–251 months). During follow-up, 13 patients (15.4%) had recurrences (9 in the sporadic group and 4 in the hereditary group, P = 0.367). Seven patients (8.2%) had local recurrence only, 1 patient (1.2%) had distant metastasis and another 5 patients (5.9%) had local and distant recurrence. Recurrences were treated by reoperation (84.6%), chemotherapy (38.5%), radiotherapy (30.8%), and close observation (1 patient developed multiple distant metastases and died from intracranial hemorrhage originating from brain metastasis [7.7%]). Some patients with recurrences were treated with a combination of methods.
In the last follow-up status, 79 patients survived with or without disease. A total of 14 patients (11 in sporadic group and 3 in hereditary group) showed BCD and 6 patients (2 patients were SD and 4 patients were PD) showed CD. Fifty-nine patients showed no disease. And total of 6 patients (7.1%) had died—4 deaths (5.1%) were in sporadic group and 2 deaths (10.0%) were in hereditary group.
Mean serum Ct level of patients with disease were 326.36 ± 314.88 pg/mL in sporadic group and 497.48±408.47 pg/mL in hereditary group (P = 0.424). And for patients groups without disease, the mean serum Ct level were 2.13 ± 1.52 pg/mL in sporadic group and 4.59 ± 2.12 pg/mL in hereditary group (P < 0.000) (Table 3).
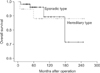
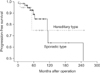
The 5-, 10-, and 20-year overall survival rates for the whole cohort were 94.3%, 89.6%, and 78.1%, respectively. And the 5-, 10-, and 20-year overall survival rates were, respectively, 96.3%, 90.7%, and 72.2% in the sporadic group and 88.8%, 88.8%, and 88.8% in the hereditary group. The Kaplan-Meier curves of overall survival of the sporadic and hereditary groups are shown in Fig. 1. The 5-, 10-, and 20-year progression-free survival rates for the whole cohort were 82.5%, 66.1%, and 22.3%, respectively. And the 5-, 10-, and 20-year progression-free survival rates in the sporadic group were, respectively, 85.6%, 62.4%, and 34.2% and in the hereditary group were 75.1% (Fig. 2). There were no significant differences between the groups in overall and progression-free survival (P = 0.775 and P = 0.866, respectively).
By multivariate analyses, only distant metastasis was a significant predictor of overall survival. Tumor size, lymph node metastasis, and distant metastases remained statistically significant predictors of disease-free survival. The hazard ratios associated with the predictor variables in the multivariate analysis are summarized in Table 4.
Of the 141 patients who underwent thyroid operations in the study institution from January 1982 to February 2012, 20 were lost to follow-up and another 36 refused genetic analysis. Twenty-six (30.6%) of the remaining 85 patients who had genetic analyses were found to have RET proto-oncogene mutation. Six patients with sporadic MTC and 20 patients with hereditary MTC had RET proto-oncogene mutations. For the RET proto-oncogene genetic screening analysis for family members, 58 of the index patients participated in the genetic analysis. Of these, 26 (44.8%, 26 of 58) had RET proto-oncogene mutations. In the sporadic group (6 patients), mutations were found at codons 618, 631, 768, and 790. In the 15 MEN 2A patients, mutations were documented at codons 611 and 634. All 4 patients with MEN 2B had mutations found at codon 918. Codon 600 mutations were found in one familial MTC patient (Fig. 3, Table 5). Among the 26 family members, 6 relatives with 634 mutations underwent thyroidectomy for treatment of MTC. And the last members were recommended for regular follow-up with neck ultrasonography in our institution or other hospital.
MTC, a rare thyroid malignancy, that represents less than 10% of all thyroid cancers, has a different clinicopathologic behavior than such malignancies as papillary and follicular cancer. It secretes Ct and may occur either as a hereditary or a nonhereditary entity. MTC occurs about 75%–80% of the time as a non-hereditary (sporadic) tumor and 20%–25% as a hereditary tumor [23]. In this study, 65 patients (76.5%) had the sporadic form of the disease and 20 patients (23.5%) had a hereditary type. Usually in sporadic MTC, the tumor is unifocal and diagnosed in the fifth or sixth decade of life. In the hereditary type, most patients are asymptomatic at discovery and diagnosed by genetic or biochemical screening tests during the early stages of the disease. The clinical manifestations of sporadic MTC include a thyroid nodule or mass, cervical lymphadenopathy or other cervical symptoms, metastatic disease, and rarely diarrhea, flushing, or Cushing syndrome due to chronic ectopic adrenocorticotropic hormone production. Hereditary MTC usually has both multifocal and bilateral disease [11]. In this study, hereditary group showed apparently higher rates of tumor multiplicity and bilaterality compared with sporadic group and younger age than those in the sporadic group. In TNM stage classification, about half of the patients belonged to early stage, and TNM stage analyses were not statistically different between the 2 groups. We believe that frequent screening with newer techniques such as neck ultrasound examinations and preoperative fine needle aspiration biopsies is leading to earlier diagnosis of MTC. Biochemical and genetic screening would also help detect persons with early stage sporadic MTC. Furthermore these advances could also affect the outcome of persons with hereditary MTC.
The initial treatment of both hereditary and sporadic forms of MTC is total thyroidectomy and removal of all neoplastic tissue present in the neck. Many studies have reported that survival of MTC patients is dependent upon the adequacy of the initial surgical procedure [1213]. At diagnosis, MTC commonly is accompanied by cervical lymphadenopathy. In this study, the prevalence of lymphadenopathy was 36.9% in the sporadic group and 25.0% in the hereditary group. Others have reported prevalence of 20% to 72% [1415]. During the early years of this study, the hospital's surgical approach was not standardized. However, since the early 1990s, total thyroidectomy and prophylactic or curative central compartment lymph node dissection has been used. We performed prophylactic MRND in 16 patients, however only 1 (9.1%) had proven lateral neck node metastases. Patients without suspected lateral lymph node metastases in image studies and with high serum Ct levels underwent prophylactic MRND. Some studies favor prophylactic lateral neck dissection in patients with large tumors (>1 cm) and in genetic carriers detected through prospective family screening or by high preoperative serum Ct levels [13]. We were unable to study the efficacy of prophylactic lateral neck dissection in this study, which should be considered in future studies.
When possible, re-operation is the main treatment for local and regional MTC recurrence. For management of distant metastases, surgery may be indicated when a single or few metastases are located in the brain, lung, or liver [2]. Of the patients in this study, some had reoperation of local and regional recurrent lesions; others had systemic chemotherapy and radiotherapy. Distant metastases are the main cause of death of MTC patients. Survival after the discovery of distant metastases is 51% at 1 year, 26% at 5 years, and 10% at 10 years [51617]. In our study, survival rates after the discovery of distant metastases was similar (76.8% at 1 year; 40% at 5 years).
The long-term overall survival and progression-free survival rates in our cohort were similar to other recent studies: overall survival rates of 94.3%, 89.6%, and 78.1% at 5, 10, and 20 years, respectively, and progression-free survival rates of 82.5%, 66.1%, and 22.3% for the same periods [17181920]. Long-term survival of the two types of MTC patients was not significantly different. Numerous parameters have been proposed as prognostic factors for the outcome for patients with MTC. Age at diagnosis, TNM stage and completeness of initial surgery are significant factors related to outcome [51417]. Although many studies note a less favorable prognosis of sporadic MTC compared with hereditary MTC due to disease presentation at an advanced stage [16172122], others, after controlling for disease stage, found that type of MTC was not an independent prognostic factor [51823]. In our cohort, tumor size, extracapsular invasion, lymph node metastasis, and distant metastases through disease course remained significant independent indicators of progression-free survival. For overall and progression-free survival, the presence of distant metastases was especially important, but the type of MTC was not significant for long-term survival.
Germline RET proto-oncogene mutations are observed in 98% of MEN 2A, in 95% of MEN 2B, and in 88% of FMTC patients. These are crucial for the onset and progression of MTC in patients with the hereditary form of the disease [924]. The American Thyroid Association has developed an MTC risk stratification index based on genotype of RET proto-oncogene mutations and this system is used to individualize the aggressiveness of treatment. Therefore, once a germline RET proto-oncogene mutation has been identified in a family, RET proto-oncogene mutation analysis should be done for all first-degree relatives of known mutation carriers [8]. About 4%–10% of patients with sporadic type MTC have germline mutations of the RET proto-oncogene [2526]. While the somatic RET proto-oncogene mutation rate has been reported to vary from 12% to 100% in many studies, the frequency and prognostic correlation of RET proto-oncogene somatic mutations in sporadic MTC remains controversial [27282930]. Our institution actively recommends RET proto-oncogene analysis of persons with sporadic MTC; however, before suggesting the genetic analysis, we must consider the problems of expense and the reluctance of Koreans to have genetic screening.
In this study, the most common mutations of index patients were found in codons 634 and the codon 600 mutation was most common in genetic screening analysis of relatives of index patients. With the use of active genetic counseling and genetic mutation analysis, we identified persons with occult hereditary MTC and recommended prophylactic or curative thyroidectomy adjusted to their risk stratification.
This study evaluated genetic mutation status and long-term follow-up in MTC patients at a single institution in Korea. We also analyzed RET proto-oncogene mutation status of their relatives as found by genetic screening. The incidence of MTC at our institution over about 30 years was 0.85% (among 16,500 patients who underwent thyroid surgery for thyroid carcinoma during this period). Introduction of RET proto-oncogene mutation analysis could lead to improved outcomes in patients detected by screening. Some patients in our institution were diagnosed by genetic screening as having RET proto-oncogene mutation and were subsequently treated for MTC. There was a 1-year-old patient that had a codon 918 mutation detected by genetic screening and underwent prophylactic thyroidectomy. His final pathology result was only c-cell hyperplasia and he has had no disease during ten years of follow-up. Unfortunately, we were unable to evaluate any relationship between the genotype and phenotype when treating these inherited malignancies. Due to a low incidence rate of MTC in Korea, there has been no systematic study of MTC in Korea. Therefore, multicenter studies would be required to verify any genotype-phenotype correlation. Nevertheless, patients with RET proto-oncogene mutation in sporadic type MTC should be closely followed and advised about associated endocrine abnormalities and disease risk for family members.
This study analyzed patients with MTC who had long-term follow-up. Most patients had favorable remission rates and long-term outcomes. Long-term survival was similar for persons with sporadic and hereditary MTC. Distant metastases appeared to be the strongest predictor of overall and disease-free survival followed by tumor size and lymph node metastasis. Earlier diagnosis, complete surgical resection of tumor foci and appropriate genetic counseling with genetic screening are essential to improve the outcome of persons with MTC.
Figures and Tables
Fig. 3
RET proto-oncogene genetic screening and counseling. *Patients underwent thyroid operation from January 1982 to February 2012.

Table 1
Comparison of clinicopathologic characteristics of sporadic and hereditary medullary thyroid carcinoma in 85 Korean patients

Table 3
Follow-up outcomes for medullary thyroid carcinoma

Values are presented as number (%) or mean ± standard deviation.
BCD, biochemical disease (detected calcitonin but no clinical disease); CD (SD), clinical disease (stable disease); CD (PD), clinical disease (progressive disease); MTC, medullary thyroid cancer.
a)With disease: biochemical disease, clinical disease.
ACKNOWLEDGEMENTS
This study was supported by a faculty research grant of Yonsei University College of Medicine for 2009 (6-2009-0131).
References
1. Bachelot A, Lombardo F, Baudin E, Bidart JM, Schlumberger M. Inheritable forms of medullary thyroid carcinoma. Biochimie. 2002; 84:61–66.
2. Pacini F, Castagna MG, Cipri C, Schlumberger M. Medullary thyroid carcinoma. Clin Oncol (R Coll Radiol). 2010; 22:475–485.
3. Farndon JR, Leight GS, Dilley WG, Baylin SB, Smallridge RC, Harrison TS, et al. Familial medullary thyroid carcinoma without associated endocrinopathies: a distinct clinical entity. Br J Surg. 1986; 73:278–281.
4. Wells SA Jr, Asa SL, Dralle H, Elisei R, Evans DB, Gagel RF, et al. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 2015; 25:567–610.
5. Kebebew E, Ituarte PH, Siperstein AE, Duh QY, Clark OH. Medullary thyroid carcinoma: clinical characteristics, treatment, prognostic factors, and a comparison of staging systems. Cancer. 2000; 88:1139–1148.
6. Fromigue J, De Baere T, Baudin E, Dromain C, Leboulleux S, Schlumberger M. Chemoembolization for liver metastases from medullary thyroid carcinoma. J Clin Endocrinol Metab. 2006; 91:2496–2499.
7. Busnardo B, Girelli ME, Simioni N, Nacamulli D, Busetto E. Nonparallel patterns of calcitonin and carcinoembryonic antigen levels in the follow-up of medullary thyroid carcinoma. Cancer. 1984; 53:278–285.
8. Kloos RT, Eng C, Evans DB, Francis GL, Gagel RF, et al. American Thyroid Association Guidelines Task Force. Medullary thyroid cancer: management guidelines of the American Thyroid Association. Thyroid. 2009; 19:565–612.
9. Eng C, Clayton D, Schuffenecker I, Lenoir G, Cote G, Gagel RF, et al. The relationship between specific RET proto-oncogene mutations and disease phenotype in multiple endocrine neoplasia type 2. International RET mutation consortium analysis. JAMA. 1996; 276:1575–1579.
10. Mathew CG, Chin KS, Easton DF, Thorpe K, Carter C, Liou GI, et al. A linked genetic marker for multiple endocrine neoplasia type 2A on chromosome 10. Nature. 1987; 328:527–528.
11. Heshmati HM, Gharib H, van Heerden JA, Sizemore GW. Advances and controversies in the diagnosis and management of medullary thyroid carcinoma. Am J Med. 1997; 103:60–69.
12. Gharib H, McConahey WM, Tiegs RD, Bergstralh EJ, Goellner JR, Grant CS, et al. Medullary thyroid carcinoma: clinicopathologic features and long-term follow-up of 65 patients treated during 1946 through 1970. Mayo Clin Proc. 1992; 67:934–940.
13. Leboulleux S, Baudin E, Travagli JP, Schlumberger M. Medullary thyroid carcinoma. Clin Endocrinol (Oxf). 2004; 61:299–310.
14. Brierley J, Tsang R, Simpson WJ, Gospodarowicz M, Sutcliffe S, Panzarella T. Medullary thyroid cancer: analyses of survival and prognostic factors and the role of radiation therapy in local control. Thyroid. 1996; 6:305–310.
15. Gülben K, Berberoglu U, Boyabatli M. Prognostic factors for sporadic medullary thyroid carcinoma. World J Surg. 2006; 30:84–90.
16. Dottorini ME, Assi A, Sironi M, Sangalli G, Spreafico G, Colombo L. Multivariate analysis of patients with medullary thyroid carcinoma. Prognostic significance and impact on treatment of clinical and pathologic variables. Cancer. 1996; 77:1556–1565.
17. Modigliani E, Cohen R, Campos JM, Conte-Devolx B, Maes B, Boneu A, et al. Prognostic factors for survival and for biochemical cure in medullary thyroid carcinoma: results in 899 patients. The GETC Study Group. Groupe d'etude des tumeurs a calcitonine. Clin Endocrinol (Oxf). 1998; 48:265–273.
18. Grozinsky-Glasberg S, Benbassat CA, Tsvetov G, Feinmesser R, Peretz H, Shimon I, et al. Medullary thyroid cancer: a retrospective analysis of a cohort treated at a single tertiary care center between 1970 and 2005. Thyroid. 2007; 17:549–556.
19. Clark JR, Fridman TR, Odell MJ, Brierley J, Walfish PG, Freeman JL. Prognostic variables and calcitonin in medullary thyroid cancer. Laryngoscope. 2005; 115:1445–1450.
20. Kebebew E, Greenspan FS, Clark OH, Woeber KA, Grunwell J. Extent of disease and practice patterns for medullary thyroid cancer. J Am Coll Surg. 2005; 200:890–896.
21. Bergholm U, Bergstrom R, Ekbom A. Long-term follow-up of patients with medullary carcinoma of the thyroid. Cancer. 1997; 79:132–138.
22. Saad MF, Ordonez NG, Rashid RK, Guido JJ, Hill CS Jr, Hickey RC, et al. Medullary carcinoma of the thyroid. A study of the clinical features and prognostic factors in 161 patients. Medicine (Baltimore). 1984; 63:319–342.
23. Raue F, Kotzerke J, Reinwein D, Schröder S, Roher HD, Deckart H, et al. Prognostic factors in medullary thyroid carcinoma: evaluation of 741 patients from the German Medullary Thyroid Carcinoma Register. Clin Investig. 1993; 71:7–12.
24. Figlioli G, Landi S, Romei C, Elisei R, Gemignani F. Medullary thyroid carcinoma (MTC) and RET proto-oncogene: mutation spectrum in the familial cases and a meta-analysis of studies on the sporadic form. Mutat Res. 2013; 752:36–44.
25. Bugalho MJ, Domingues R, Santos JR, Catarino AL, Sobrinho L. Mutation analysis of the RET proto-oncogene and early thyroidectomy: results of a Portuguese cancer centre. Surgery. 2007; 141:90–95.
26. Elisei R, Romei C, Cosci B, Agate L, Bottici V, Molinaro E, et al. RET genetic screening in patients with medullary thyroid cancer and their relatives: experience with 807 individuals at one center. J Clin Endocrinol Metab. 2007; 92:4725–4729.
27. Romei C, Elisei R, Pinchera A, Ceccherini I, Molinaro E, Mancusi F, et al. Somatic mutations of the ret protooncogene in sporadic medullary thyroid carcinoma are not restricted to exon 16 and are associated with tumor recurrence. J Clin Endocrinol Metab. 1996; 81:1619–1622.
28. Jhiang SM, Fithian L, Weghorst CM, Clark OH, Falko JM, O'Dorisio TM, et al. RET mutation screening in MEN2 patients and discovery of a novel mutation in a sporadic medullary thyroid carcinoma. Thyroid. 1996; 6:115–121.
29. Marsh DJ, Theodosopoulos G, Martin-Schulte K, Richardson AL, Philips J, Röher HD, et al. Genome-wide copy number imbalances identified in familial and sporadic medullary thyroid carcinoma. J Clin Endocrinol Metab. 2003; 88:1866–1872.
30. Dvorakova S, Vaclavikova E, Sykorova V, Vcelak J, Novak Z, Duskova J, et al. Somatic mutations in the RET proto-oncogene in sporadic medullary thyroid carcinomas. Mol Cell Endocrinol. 2008; 284:21–27.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download