Abstract
Purpose
Single incision laparoscopic cholecystectomy (SILC) has some technical problems. Our group has performed needlescopic grasper assisted SILC (nSILC) to overcome these problems. In this study, we introduce our technique and evaluate the safety and feasibility of this technique compared with the conventional laparoscopic cholecystectomy (CLC).
Methods
The medical records of 485 patients who received nSILC and CLC were reviewed retrospectively. Surgical outcomes including operative time, hospital stay, postoperative pain and perioperative complication were compared between the 2 techniques.
Since the introduction of laparoscopic cholecystectomy in 1985 [1], continuous trials for less invasive approaches by reducing the number and size of the ports have been attempted by many researchers [2]. In this context single incision laparoscopic cholecystectomy (SILC) was introduced by Navarra et al. in 1997 [3]. However, this technique had spread slowly until 2008 due to technical problems and the requirement for highly developed surgical skill [4]. Although this technique has become more attractive with an improvement in skills and the development of new devices in recent years, it still has some problems such as repeated conflict between operating instruments, a lack of proprioception induced by the crossing of instruments, and consequently reduced visualization of key components of a cholecystectomy. These problems can increase the risk of bile duct injuries during SILC.
To prevent the bile duct injuries, "critical view of safety" (CVS) technique was first introduced in 1995 by Strasberg et al. and this technique has been adopted widely by surgeons around the world for performance of laparoscopic cholecystectomy. To attain CVS, the triangle of Calot must be dissected free of fat and fibrous tissue, and the base of the gallbladder be separated from the cystic plate. Consequently, two, and only 2, structures should be entering the gallbladder, and these can be seen circumferentially [5678].
Various techniques such as clipping and suture traction have been introduced by many groups to solve the problems of SILC, through the adequate traction of the gallbladder, and to attain CVS more safely. For the same reasons, needlescopic graspers (Minilap Grasper, Stryker, San Jose, CA, USA) have been used in our group and our group defined this technique as needlescopic grasper assisted SILC (nSILC). In this study, we introduce our experiences of nSILC technique and evaluate the safety and feasibility of this technique for the treatment of patients with benign gallbladder disease through a comparison with our experiences of conventional laparoscopic cholecystectomy (CLC).
From October 2011 to December 2012, 485 patients who underwent laparoscopic cholecystectomy for acute and chronic cholecystitis at Uijeongbu St. Mary's Hospital, The Catholic University of Korea were included in this study. CLC was performed in 252 patients and needlescopic assisted single nSILC was performed in 233 patients. Operation technique for cholecystectomy was selected based on the patients' choice after detailed description of the procedures. Among these patients, 102 patients received laparoscopic cholecystectomy due to acute inflammation including acute cholecystitis, gangrenous cholecystitis and gallbladder empyema. Acute cholecystitis was defined by the Tokyo guideline (TG13) as described in Table 1 [9]. Medical records were reviewed retrospectively after approval by the Institutional Review Board of Uijeongbu St. Mary's Hospital (approval number: UC15RISI0004).
All operations were performed by the same surgical team that had experiences of more than 100 cases of SILC and reached a plateau in their learning curve. The surgical techniques were standardized and described in our previous report [10]. Briefly, nSILCs were performed routinely through the SILS Port (Covidien, Dublin, Ireland) with a snake liver retractor to push up the hepatic hilum in the cephalad direction; and ENDOPATH electrosurgery probe plus system (Ethicon, Somerville, NJ, USA) composed of suction, irrigation unit, and hook electrode for meticulous dissection. For clear visualization of the triangle of Calot and obtaining CVS, lateral traction of the gallbladder was performed using an additional 2-mm needlescopic grasper, which punctured directly into the right abdomen (Figs. 1, 2). The key point of our technique is the clear visualization and identification of important structures through adequate traction of the gallbladder without crossing or conflict between operating instruments. In almost all cases, CVS could be achieved safely by this technique. After achieving CVS, cystic duct and artery were ligated using a 5-mm Hem-o-lock clip and transected using laparoscopic scissors. CLC was performed as a routine maneuver using 3-port placed at umbilical, epigastric, and right abdomen area.
The medical records of 485 patients were reviewed retrospectively to investigate the patients' demographics and operative outcomes such as operating time, CVS identification time, intraoperative complication, bile spillage, conversion to open surgery, postoperative complication, postoperative pain, and the length of hospital stay.
The postoperative pain was measured using visual analog scale for pain (VAS pain score system). To estimate the difficulty of operation, operation records, preoperative CT, and video files were reviewed. The degree of pericholecystic adhesion, wall thickening, and gallbladder distension was scored from 0 to 2 and the level of surgical difficulty was categorized into 4 grades according to the sum of score (grade I, 0–1; grade II, 2–3; grade III, 4–5; grade IV, 6).
The patients' demographics and surgical outcomes were compared between groups (nSILC group vs. CLC group). Additionally, subgroup analysis was performed to reduce the effects of surgical difficulty on the surgical outcomes and evaluate the safety and feasibility of nSILC in each surgical difficulty. The patients were subgrouped into easy group (surgical difficulty grades I and II) and difficult group (surgical difficulty grades III and IV), and operative outcomes of the nSILC and CLC groups were compared in each subgroup.
Chi-square tests (or Fisher exact test, when necessary) were performed to compare categorical variables and t-tests (or Mann-Whitney test, when necessary) for continuous variables. All analyses were performed with IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA). Results were considered to be significant when P-values were less than 0.05.
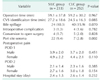
The demographics of patients included in this study are shown in Table 2. The patients who underwent nSILC were younger than those who underwent CLC (48.7 ± 14.7 vs. 53.7 ± 14.8, P < 0.001) and there were more female patients in the nSILC group (70% vs. 42%, P < 0.001).
The proportion of the surgery with surgical difficulty grade I was higher in the nSILC group (73% vs. 48%) and the patients with acute inflammation was higher in the CLC group (14% vs. 28%, P < 0.001). Fifty-four patients (23%) who underwent nSILC and 52 patients (21%) who underwent CLC received abdominal surgery previously and there was no significant difference. Most of these patients received lower abdominal surgery including appendectomy, hysterectomy, C-section and so on. There were no significant differences between groups in body mass index and admission route.
Perioperative surgical outcomes and complications in the nSILC and CLC groups are shown in Table 3. The mean operation time was similar in both groups (59.1 minutes vs, 59.2 minutes). The CVS identification time for patients who underwent nSILC was slightly longer in comparison with those who underwent CLC (27.2 minutes vs. 24.5 minutes); however, there was no statistical significance (P = 0.085). Bile spillage caused by gallbladder perforation during dissection occurred slightly more in the CLC group (10.3% vs. 15.9%); however, it was also not significant (P = 0.07).
During this period, intraoperative complications occurred in 4 patients (bile duct injury 2, vascular injury 2) who underwent CLC and 3 patients (bile duct injury 1, vascular injury 2) who underwent nSILC. The incidence rate of intraoperative complication was not significantly different between groups (1.3% vs. 1.6%, P = 0.782). In addition to intraoperative complication, the rate of conversion to open surgery was not significantly different between groups (1.7% vs. 2.0%, P = 0.828). However, wound complications including port site seroma and abscess were more frequently observed in the nSILC group (9.4% vs. 2.8 %, P = 0.002).
For postoperative pain, pain scale measured at the morning of postoperative days 1 and 2 showed no significant difference between groups. There was also no significant difference between groups in length of hospital stay after surgery.
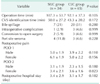
In easy group (surgical difficulty grades I and II), 199 patients underwent nSILC and 187 patients underwent CLC. Operative outcomes in patients underwent nSILC and CLC in group I are shown in Table 4. The mean CVS identification time was significantly longer in the nSILC group than CLC group (23.4 minutes vs. 17.9 minutes, P < 0.001) and wound complications occurred more frequently in the nSILC group than CLC group (9.0% vs. 2.1%, P = 0.003). However, there was no significant difference between groups in other surgical outcomes including operative time, bile spillage, intraoperative complication, conversion to open surgery, postoperative pain and length of hospital stay after surgery.
In difficult group (Surgical difficulty grades III and IV), 34 patients underwent nSILC and 65 patients underwent CLC. Operative outcomes in patients who underwent nSILC and CLC in group II are summarized in Table 5. There was no significant difference between groups in mean operation time, CVS identification time, perioperative complication, and postoperative pain.
With the technical improvement and development of new instruments, SILC has been commonly performed for benign gallbladder disease. SILC has the advantage of less invasiveness in comparison with CLC, which requires 3 or 4 incisions. However, this procedure is technically more difficult in comparison with CLC due to the limited motion of the working instruments, limited triangulation, and repeated confliction between working instruments [11]. These problems lead to inadequate traction of the gallbladder during dissection of Calot's triangle and obtaining CVS. For these reasons, concerns about biliary complication continue to be active subjects of debate, and previous studies that reported on the safety and feasibility of SILC were mostly confined to selective patients with exclusion criteria such as acute cholecystitis, obese patients, history of previous abdominal surgery, and so on [12].
Several authors have described different methods for adequate traction of the gallbladder in the lateral and cephalad direction [1314151617]. Some surgeons have used traction sutures with different methods in each group and others have used instruments such as the magnetic anchoring guidance system and Carter Thomson needle. Our group has used the needlescopic grasper and the snake liver retractor for adequate traction of the gallbladder and clear visualization of Calot's triangle. The needlescopic grasper, which is inserted through direct puncture on the right upper abdomen, makes it possible to preserve triangulation between instruments and minimize frequent conflict between instruments. Therefore, nSILC can be performed as a similar technique with CLC and similar cosmetic effect with pure SILC. The other point of our technique is the snake liver retractor which is inserted through one of the SILS port and used for clear visualization of the Calot's triangle by pushing hepatic hilum in the cephalad direction. This technique allows adequate traction of gallbladder, clear visualization, and technical similarity with CLC. Consequently, our technique makes it possible to expand the indication of SILC to cases with acute inflammation or obesity.
In this study, the surgical outcomes of nSILC were comparable with those of CLC. Although port site complications occurred more in nSILC group, there was no significant difference in operation time, occurrence rate of perioperative complication, and length of hospital stay. In subgroup analysis performed in each surgical difficulty, the surgical outcomes of nSILC were comparable with those of CLC not only in easy group but also in difficult group. These results mean that our technique (nSILC) using auxiliary needlescopic grasper can be applied safely not only in selective patients, but also in difficult cases.
Some previous studies have concluded that postoperative pain in patients who underwent SILC is less than in patients with CLC, whereas our results showed no difference in pain score at postoperative days 1 and 2 between groups.
In conclusion, the results of our study demonstrate that nSILC is a safe and feasible technique with similar outcome to that of CLC not only in selective patients but also in patients with acute attacks of cholecystitis and other difficult factors such as obesity, previous operation, and so on. Therefore, this technique can be an alternative to standard laparoscopic cholecystectomy and a training module for beginners of SILC due to its technical similarity to CLC. However, more high-powered randomized control studies are required to validate these results.
Figures and Tables
Fig. 1
External view of needlescopic grasper assisted single incision laparoscopic cholecystectomy procedure. Needlescopic grasper (black arrow) was used for traction through direct puncture on right upper abdomen. Snake liver retractor (white arrow) was used for cephalad traction of liver to obtain better visualization.

Fig. 2
Intra-abdominal view of needlescopic grasper (black arrow) assisted single incision laparoscopic cholecystectomy using snake liver retractor (white arrow). Clear visualization can be obtained by lateral and cephalad traction.

References
1. Solomon D, Bell RL, Duffy AJ, Roberts KE. Single-port cholecystectomy: small scar, short learning curve. Surg Endosc. 2010; 24:2954–2957.
2. Pan MX, Jiang ZS, Cheng Y, Xu XP, Zhang Z, Qin JS, et al. Single-incision vs three-port laparoscopic cholecystectomy: prospective randomized study. World J Gastroenterol. 2013; 19:394–398.
3. Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997; 84:695.
4. Wagner MJ, Kern H, Hapfelmeier A, Mehler J, Schoenberg MH. Single-port cholecystectomy versus multi-port cholecystectomy: a prospective cohort study with 222 patients. World J Surg. 2013; 37:991–998.
5. Strasberg SM, Brunt LM. Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg. 2010; 211:132–138.
6. Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C. One thousand laparoscopic cholecystectomies in a single surgical unit using the "critical view of safety" technique. J Gastrointest Surg. 2009; 13:498–503.
7. Heistermann HP, Tobusch A, Palmes D. Prevention of bile duct injuries after laparoscopic cholecystectomy. "The critical view of safety". Zentralbl Chir. 2006; 131:460–465.
8. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995; 180:101–125.
9. Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, et al. TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2013; 20:35–46.
10. Kim MJ, Kim TS, Kim KH, An CH, Kim JS. Safety and feasibility of needlescopic grasper-assisted single-incision laparoscopic cholecystectomy in patients with acute cholecystitis: comparison with three-port laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2014; 24:523–527.
11. Barband A, Fakhree MB, Kakaei F, Daryani A. Single-incision laparoscopic cholecystectomy using glove port in comparison with standard laparoscopic cholecystectomy SILC using glove port. Surg Laparosc Endosc Percutan Tech. 2012; 22:17–20.
12. Cheon SU, Moon JI, Choi IS. Risk factors for prolonged operative time in single-incision laparoscopic cholecystectomy. Ann Surg Treat Res. 2015; 89:247–253.
13. Srikanth G, Shetty N, Babu P. A technique for gall bladder fundal traction in single-incision laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2011; 21:e239–e241.
14. Horisberger K, Grossen E, Schöb O. How to meet the challenge of flexible exposure of the Calot triangle in SILS cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2012; 22:e63–e65.
15. Canes D, Desai MM, Aron M, Haber GP, Goel RK, Stein RJ, et al. Transumbilical single-port surgery: evolution and current status. Eur Urol. 2008; 54:1020–1029.
16. Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A. 1999; 9:361–364.
17. Raman JD, Scott DJ, Cadeddu JA. Role of magnetic anchors during laparoendoscopic single site surgery and NOTES. J Endourol. 2009; 23:781–786.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download