Abstract
Purpose
Local anesthetic wound infusion has been previously investigated in postoperative pain management. However, a limited number of studies have evaluated its use in laparoscopic colorectal surgery. This study aims to evaluate whether ropivacaine wound infusion is effective for postoperative pain management after laparoscopic surgery in patients with colorectal cancer.
Methods
This prospective study included 184 patients who underwent laparoscopic surgery for colorectal cancer between July 2012 and June 2013. The patients were grouped as the combined group (intravenous patient-controlled analgesia [IV-PCA] plus continuous wound infusion with ropivacaine, n = 92) and the PCA group (IV-PCA only, n = 92). Efficacy and safety were assessed in terms of numeric rating scale (NRS) pain score, opioid consumption, postoperative recovery, and complications.
Results
The total quantity of PCA fentanyl was significantly less in the combined group than in the PCA group (P < 0.001). The NRS score of the combined group was not higher than in the PCA group, despite less opioid consumption. There were no differences between groups for postoperative recovery and most complications, including wound complications. However, the rate of nausea and vomiting was significantly lower in the combined group (P = 0.022).
Postoperative pain is one of the major concerns of surgical patients. It may contribute to a variety of complications and delay recovery after surgery [123]. Various analgesic modalities have been used to reduce postoperative pain, however pain control remains a challenging area for most surgeons and anesthesiologists [24]. The main goal of analgesics is to provide adequate pain relief without side effects. Thus, multimodal approaches have become the standard treatment for surgical patients to achieve effective pain control and minimize toxicities [45].
A major source of pain after abdominal surgery is derived from the abdominal wall incision [67]. Local anesthetic wound infusion provides analgesia by blocking afferent nerves innervating the abdominal wall [57]. This technique can produce sustained analgesia with the continuous infusion of local anesthetics, such as ropivacaine or bupivacaine, through a catheter placed into the musculo-fascial layer [58]. Several studies have reported that local anesthetic wound infusion improves postoperative pain and reduces opioid-related complications in patients undergoing abdominal surgery [5910]. However, these studies were generally performed in patients undergoing open abdominal surgery. Currently, minimally invasive surgery has received increasing attention, and laparoscopic approaches to abdominal surgery have become more common. Despite this, few studies have heretofore evaluated the use of local anesthetic wound infusion for laparoscopic surgery, especially for colorectal conditions.
In this study, our objective was to evaluate whether continuous wound infusion with ropivacaine is effective for postoperative pain management after laparoscopic surgery for patients with colorectal cancer.
This is a prospective cohort study performed from July 2012 to June 2013 at a tertiary university based hospital. A total of 184 patients, who were 18–80 years old and who underwent laparoscopic surgery for colorectal cancer, were included. All patients had histologically confirmed primary adenocarcinoma and underwent radical surgery for primary lesions. Patients were excluded if they met the following criteria: American Society of Anesthesiologists (ASA) physical status classification of IV or higher, taking opioids due to chronic pain, conversion to open surgery, presence of a stoma, combined organ resection, inability to operate a PCA device, or inability to understand the numeric rating scale (NRS) that was used for pain assessments.
Before the surgery, we explained the clinical benefits and the risks of the continuous IV-PCA and continuous wound infusion with ropivacaine to patients. Patients were then grouped as the combined group (continuous IV-PCA and continuous wound infusion with ropivacaine) and the PCA group (continuous IV-PCA only). Taking into account our preliminary pilot data for the significant difference in NRS between each group, we calculated that 83 patients in each group were required to detect a 2 point difference in NRS score between the 2 groups with a power of 80% and 5% level of significance. We enrolled 184 patients (92 patients in each group) to allow for 10% dropout. This study was approved by the Samsung Medical Center Institutional Review Board (2012-05-031-004), and each patient provided written informed consent.
A 12-mm camera port was placed on the umbilicus, and an additional 3 to 4 trocars (one or two 12-mm and one or two 5-mm trocars) were placed on each quadrant of the abdomen. For specimen extraction, an umbilical wound was extended to 3.5–6 cm in length. At the end of the laparoscopic surgery, the peritoneum and musculo-fascial layer were closed. The combined group received continuous wound infusion with ropivacaine using the ON-Q PainBuster System (I-Flow Corp., Lake Forest, CA, USA). A multi-hole Soaker catheter (ON-Q PainBuster System) was inserted into the subcutaneous layer and placed on the musculo-fascial layer along the midline wound. The subcutaneous layer and skin were then closed, and the catheter was connected to a single balloon pump (ON-Q PainBuster System) filled with 270 mL of 0.5% ropivacaine solution. This solution was continuously infused at a rate of 5 mL/hr.
In addition, IV-PCA was administered to both the combined group and PCA group. The IV-PCA device was filled with 1,500 mcg of fentanyl in 100 mL of normal saline. IV-PCA was continuously infused at a rate of 15 mcg/hr and set to deliver a bolus dose of 15 mcg with a 15-minute lockout time. IV-PCA was removed when patients disconnected the intravenous line for fluid, exhausted PCA, or had PCA-related side effects. After the surgery, 50 mg of pethidine was given intravenously up to 3 times per day as a rescue opioid for patients who requested additional medication for better pain relief.
Patient characteristics and operation data of the 2 groups were analyzed. Opioid consumption was compared between the 2 groups by determining the quantity of IV-PCA fentanyl and the number of rescue opioid administrations. Postoperative pain at rest was estimated daily until discharge using the NRS from 0 (no pain) to 10 (worst pain). Patient satisfaction with pain control was assessed by a questionnaire, which was completed at hospital discharge. The primary outcome of this study was pain score, and the secondary outcomes were opioid consumption and opioid-related side effects.
Statistical analysis was performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Patient characteristics were compared between groups using the t-test, chi-square test, and linear by linear association. Continuous variables for pain control were analyzed with the Student t-test, and categorical data were analyzed with the chi-square test and linear by linear association. P-values were derived from two-tailed tests and P < 0.05 was considered statistically significant.
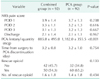
A total of 184 patients were enrolled in this study, 92 in each group. Patient characteristics were compared between the 2 groups (Table 1). There were no significant differences between the combined and PCA groups for age, gender, ASA physical status classification, and body mass index. The length of skin incision was 4.9 ± 1.1 cm in the combined group and 4.8 ± 1.3 cm in the PCA group; the difference between groups was not statistically significant (P = 0.336). The type of surgical procedure and tumor pathologic stage were also similar for the 2 groups.
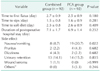
Pain intensity was estimated daily using the NRS. The NRS pain score declined gradually with time in both groups (Table 2).
Opioid consumption was assessed by determining the total quantity of PCA fentanyl received and the use of rescue opioids. The total quantity of PCA fentanyl was significantly less in the combined group than in the PCA group (P < 0.001). The time from operation until discontinuation of the PCA was 3.2 days in both groups. The percentage of patients requiring rescue opioids was lower in the combined group than in the PCA group, but the difference between groups did not achieve statistical significance (P = 0.133) (Table 2).
Patient satisfaction with pain control was assessed by a questionnaire. The percentage of patients satisfied with their pain relief was 75.9% in the combined group and 62.9% in the PCA group. In addition, 88.6% of patients in the combined group indicated that they would like to receive the ON-Q PainBuster System again.
Bowel function recovery was compared in both groups. There were no significant differences between groups for the time to first flatus, time to sips, or time to soft diet (Table 3).
Side effects were noted in 28 and 42 patients in the combined and PCA groups, respectively. Nausea and vomiting occurred in 8 patients in the combined group and 19 patients in the PCA group (P = 0.022). One patient in the PCA group discontinued IV-PCA due to nausea and vomiting. The rate of wound complications was not increased in patients receiving ropivacaine wound infusion. The incidence of other side effects, such as pruritus, dizziness, and urinary retention did not differ between the 2 groups (Table 3).
In this study, we assessed the efficacy of continuous wound infusion with ropivacaine for postoperative pain management after laparoscopic surgery in patients with colorectal cancer. The total quantity of PCA fentanyl was significantly less in the combined group than in the PCA group. The rate of nausea and vomiting, the most common opioid-related side effect, was also significantly lower in the combined group. The NRS scores were not different in the combined group and the PCA group. It is possible that PCA enables patients to control the delivery of analgesic themselves until a tolerable state for pain.
The most common form of postoperative analgesia, IV-PCA, provides effective pain control, allows self-control by the patient, and is easy to use. However, many patients with IV-PCA experience substantial opioid-related side effects [11121314]. Teng et al. [15] reported that patients receiving IV-PCA experienced nausea, vomiting, pruritus, urinary retention, and sedation. Nausea and vomiting, which occurred in 18% of patients, were the most common side effects. The substantial rate of opioidrelated side effects has led to the search for an effective use of local anesthetics in the postoperative period.
Previous reports have noted the efficacy of various local anesthetic-based methods of postoperative analgesia, including simple subcutaneous wound infiltration, transversus abdominis plane blocks, and intraperitoneal injection of local anesthetic [1617]. These methods improve postoperative pain, but administration of local anesthetics on a one-time basis is accompanied by the major limitation of a short duration of action [9]. Accordingly, continuous wound infusion with ropivacaine or bupivacaine has been advocated, as it can provide safe, simple, and sustained postoperative analgesia. Chan et al. [10] showed that continuous wound infusion with ropivacaine reduced morphine consumption and pain scores in patients who underwent open hepatic surgery. In addition, a previous study involving colorectal surgery noted similar results [18]. In contrast, Polglase et al. [1] reported that ropivacaine wound infusion provided no clinical advantage for patients undergoing open colorectal surgery.
Laparoscopic surgery has been considered as the technique with less postoperative pain compared to open surgery. However, several studies have reported that postoperative pain intensity was not much different between laparoscopic surgery and open surgery [1920]. Therefore, the pain after laparoscopic surgery should be considered important, as in the case of open surgery. Currently, laparoscopic surgery for colorectal cancer patients has become more common, but little has been published about the efficacy of ropivacaine wound infusion after this type of surgery. Only one previous trial assessed the efficacy of continuous wound infusion with ropivacaine for patients undergoing laparoscopic colorectal surgery [21]. In that randomized controlled trial of 45 patients, ropivacaine wound infusion improved early respiratory function but did not provide any other advantages. However, the small number of patients and variety of diseases were limitations of the trial.
Our study has some limitations. This study was a prospective cohort study, rather than a randomized controlled trial. Additionally, ropivacaine wound infusion costs approximately United States dollar 250 at Samsung Medical Center. There was no financial support for our research, so patients had to pay on their own. Thus, we could not perform randomization of patients into the 2 groups; however, there were no significant differences between the groups in any of the analyzed patient or surgical characteristics. One of the major limitations was the negative result for the primary endpoint although positive findings for secondary endpoints were observed. In addition, we used the NRS to assess postoperative pain, which is not a very sensitive parameter and might confound the results. Thus, we attempted to reduce the confounding effect by using the mean value of the pain score measured 3 times a day. Other potential confounders included that patients controlled PCA requirements, body mass index was not considered when comparing the amount of PCA used, and coanalgesia such as opioid rescue was used to control pain. A major strength of the study was that we included a large number of relatively homogeneous patients, which contrasts with the methodology of most previous studies. Currently, minimally invasive surgery and fast-track protocols are widely used, and the laparoscopic approach for colorectal cancer surgery has become increasingly common. Thus, this study is more clinically useful than previous studies evaluating patients undergoing open laparotomy. We expect that this technique can be beneficial for many surgical patients, especially those who are older, have significant comorbidities, or are particularly susceptible to pain.
In conclusion, this study showed clinical efficacy of ropivacaine wound infusion for postoperative pain management in colorectal cancer patients undergoing laparoscopic surgery. Continuous wound infusion with ropivacaine significantly reduced postoperative opioid requirements and the incidence of nausea/vomiting. These results may thereby help surgeons manage postoperative pain and reduce opioid-related adverse effects in laparoscopic surgical patients.
Figures and Tables
References
1. Polglase AL, McMurrick PJ, Simpson PJ, Wale RJ, Carne PW, Johnson W, et al. Continuous wound infusion of local anesthetic for the control of pain after elective abdominal colorectal surgery. Dis Colon Rectum. 2007; 50:2158–2167.
2. Vintar N, Pozlep G, Rawal N, Godec M, Rakovec S. Incisional self-administration of bupivacaine or ropivacaine provides effective analgesia after inguinal hernia repair. Can J Anaesth. 2002; 49:481–486.
3. Su Y, Zhang Z, Zhang Q, Zhang Y, Liu Z. Analgesic efficacy of bilateral superficial and deep cervical plexus block in patients with secondary hyperparathyroidism due to chronic renal failure. Ann Surg Treat Res. 2015; 89:325–329.
4. Karthikesalingam A, Walsh SR, Markar SR, Sadat U, Tang TY, Malata CM. Continuous wound infusion of local anaesthetic agents following colorectal surgery: systematic review and meta-analysis. World J Gastroenterol. 2008; 14:5301–5305.
5. Wang LW, Wong SW, Crowe PJ, Khor KE, Jastrzab G, Parasyn AD, et al. Wound infusion with local anaesthesia after laparotomy: a randomized controlled trial. ANZ J Surg. 2010; 80:794–801.
6. Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010; (12):CD007705.
7. McDonnell JG, O'Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007; 104:193–197.
8. Beaussier M, El'Ayoubi H, Schiffer E, Rollin M, Parc Y, Mazoit JX, et al. Continuous preperitoneal infusion of ropivacaine provides effective analgesia and accelerates recovery after colorectal surgery: a randomized, double-blind, placebo-controlled study. Anesthesiology. 2007; 107:461–468.
9. Ventham NT, O'Neill S, Johns N, Brady RR, Fearon KC. Evaluation of novel local anesthetic wound infiltration techniques for postoperative pain following colorectal resection surgery: a meta-analysis. Dis Colon Rectum. 2014; 57:237–250.
10. Chan SK, Lai PB, Li PT, Wong J, Karmakar MK, Lee KF, et al. The analgesic efficacy of continuous wound instillation with ropivacaine after open hepatic surgery. Anaesthesia. 2010; 65:1180–1186.
11. Grass JA. Patient-controlled analgesia. Anesth Analg. 2005; 101:5 Suppl. S44–S61.
12. Palmer PP, Royal MA, Miller RD. Novel delivery systems for postoperative analgesia. Best Pract Res Clin Anaesthesiol. 2014; 28:81–90.
13. Palmer PP, Miller RD. Current and developing methods of patient-controlled analgesia. Anesthesiol Clin. 2010; 28:587–599.
14. Wheeler M, Oderda GM, Ashburn MA, Lipman AG. Adverse events associated with postoperative opioid analgesia: a systematic review. J Pain. 2002; 3:159–180.
15. Teng YH, Hu JS, Tsai SK, Liew C, Lui PW. Efficacy and adverse effects of patient-controlled epidural or intravenous analgesia after major surgery. Chang Gung Med J. 2004; 27:877–886.
16. Chyung JW, Shin DG, Kwon Y, Cho DH, Lee KB, Park SS, et al. Tumescent local anesthetic technique for inguinal hernia repairs. Ann Surg Treat Res. 2014; 87:325–330.
17. Kang KH, Kim BS, Kang H. The benefits of preincision ropivacaine infiltration for reducing postoperative pain after robotic bilateral axillo-breast approach thyroidectomy: a prospective, randomized, double-blind, placebo-controlled study. Ann Surg Treat Res. 2015; 88:193–199.
18. Fustran N, Dalmau A, Ferreres E, Camprubí I, Sanzol R, Redondo S, et al. Postoperative analgesia with continuous wound infusion of local anaesthesia vs saline: a double-blind randomized, controlled trial in colorectal surgery. Colorectal Dis. 2015; 17:342–350.
19. Lloyd GM, Kirby R, Hemingway DM, Keane FB, Miller AS, Neary P. The RAPID protocol enhances patient recovery after both laparoscopic and open colorectal resections. Surg Endosc. 2010; 24:1434–1439.
20. Vignali A, Di Palo S, Orsenigo E, Ghirardelli L, Radaelli G, Staudacher C. Effect of prednisolone on local and systemic response in laparoscopic vs. open colon surgery: a randomized, double-blind, placebo-controlled trial. Dis Colon Rectum. 2009; 52:1080–1088.
21. Moore SE, Reid KC, Draganic BD, Smith SR. Randomized clinical trial of ropivacaine wound infusion following laparoscopic colorectal surgery. Tech Coloproctol. 2012; 16:431–436.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download