Abstract
Purpose
To propose a new, multivariable risk-scoring model for predicting 30-day mortality in individuals underwent repair of abdominal aortic aneurysms (AAA).
Methods
Four hundred eighty-five consecutive patients who underwent AAA repair from January 2000 to December 2010 were included in the study. Univariate and multivariate analyses were performed to evaluate the risk factors, and a risk-scoring model was developed.
Results
Multivariate analysis identified three independent preoperative risk factors associated with mortality, and a risk-scoring model was created by assigning an equal value to each factor. The independent predictors were location of the AAA, rupture of AAA, and preoperative pulmonary dysfunction. The multivariable regression model demonstrated moderate discrimination (c statistic, 0.811) and calibration (Hosmer-Lemeshow test, P = 0.793). The observed mortality rate did not differ significantly from that predicted by our risk-scoring model.
Abdominal aortic aneurysm (AAA) is a degenerative disease that becomes more prevalent with age. Due to the increasing overall life expectancy in developed countries, growing numbers of elderly patients require AAA repair [1]. Most patients with a ruptured AAA die immediately, and even those who survive long enough to reach the hospital have an operative mortality rate of 30%–50% [2]. Elective AAA repair may prevent rupture in patients at risk, and it is associated with much lower operative mortality: approximately 5% for open surgery and 1%–2% for endovascular aneurysm repair (EVAR) [3]. In the management of AAA, predicting the mortality risk of patients prior to open or endovascular repair of a ruptured or intact aneurysm is difficult. Therefore, a risk-scoring model could be very useful, particularly for surgeons who rarely deal with this problem. There are many risk estimation models already available across a range of surgical specialties; these are often used to calculate risk-adjusted, surgeon-specific mortality data [45]. Although these models may help to inform surgeons and patients about the individual risks of intervention, most are much too complex to be practical, and some are outdated and no longer able to predict outcomes accurately in the era of endovascular procedures [56789].
The aim of our study was to evaluate retrospectively the clinical outcomes and risk factors associated with open and endovascular AAA repair, and to propose a new, simplified, multivariable risk-scoring model to enable easy prediction of 30-day mortality in individual patients.
This was a retrospective, observational study using data extracted from patients' medical records. The study protocol was approved by the hospital's Institutional Review Board. A total of 485 patients who underwent open or endovascular AAA repair at our institution from January 2000 to December 2010 were included in the study. The risk factors of interest included diabetes mellitus, hypertension, recent smoking, coronary artery disease, renal dysfunction, and pulmonary dysfunction. Other data, including clinical presentation, and operative and postoperative characteristics, were recorded prospectively in a database and analyzed retrospectively as part of this study. The primary outcome was 30-day mortality, defined as death within 30 days of an elective or emergency AAA repair procedure, regardless of the cause. Deaths occurring after discharge but within the 30-day interval were captured using the National Health Insurance system of the Republic of Korea, which records all deaths.
All results represent mean values. Categorical variables are presented as frequencies and percentages, and continuous variables as mean and standard deviation. The scoring system used for predicting 30-day mortality was based on a logistic model described elsewhere [10]. A logistic regression model was developed to predict 30-day mortality and validated using the bootstrap method. The first step in model development was to evaluate the univariate relationships between patient characteristics (baseline characteristics, risk factors, operative and postoperative variables) and 30-day mortality (Table 1). Risk factors showing a clinically significant (P < 0.1) relationship with 30-day mortality in univariate analyses were chosen as candidate variables for the scoring system; however, we excluded operative characteristics and postoperative complications because we sought to develop a model solely for preoperative use. Next, the predictive power of the predetermined factors was tested using a bootstrap resampling procedure, in which a logistic regression model with backward elimination of predictors was repeated for each of 1,000 bootstrap resamplings. A 50% relative frequency of selection of bootstrap resampling was the criterion for inclusion in the final logistic model. To evaluate the fit of this model, the c statistic (0.811) was used to assess discrimination, and the Hosmer-Lemeshow test (P = 0.793) to measure calibration.
All reported P-values were two-sided, and P-values < 0.05 were considered statistically significant. All data manipulation and statistical analyses were performed using SAS ver. 9.2 (SAS Institute Inc., Cary, NC, USA).
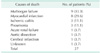
The clinical characteristics of the patients are summarized in Table 1. Of the 485 patients, 408 (84.1%) were men, and 77 (15.9%) were women, with a mean age of 69 years. Of the 485 AAA repairs, 160 (33.0%) were EVARs, and 325 (67.0%) were open surgical repairs. Elective AAA repair was performed in 420 (86.6%) of the patients and emergency repair in 65 patients (13.4%). Coronary artery disease was diagnosed in 72 patients (14.9%); 35 underwent coronary revascularization (22 percutaneous coronary interventions and 13 coronary artery bypass grafts), and 37 were treated conservatively. There were 27 mortalities (5.6%) within 30 days of the AAA repair, and the causes of death are listed in Table 2. The most common cause of death was multiorgan failure (9 patients, 33.3%) followed by myocardial infarction (8 patients, 29.6%).
The relationship between clinical characteristics and 30-day mortality post-repair, as determined by univariate analyses, is shown in Table 1. Patient age (odds ratio [OR], 1.07; 95% confidence interval [CI], 1.02–1.13; P = 0.010) was the only demographic variable significantly associated with 30-day mortality. Among features related to AAA anatomy and procedure timing, the followings were significant predictors of 30-day mortality: maximal diameter of the AAA (OR, 1.29; 95% CI, 1.07–1.56; P = 0.008), location of the AAA (supra-/juxta-renal) (OR, 4.22; 95% CI, 1.90–9.38; P < 0.001), rupture of AAA (OR, 6.98; 95% CI, 3.04–16.03; P < 0.001), and emergency repair (OR, 7.23; 95% CI, 3.22–16.23; P < 0.001). Among the preoperative clinical characteristics, the followings were statistically significant: pulmonary dysfunction (OR, 7.70; 95% CI, 2.51–23.64; P < 0.001) and serum hemoglobin (OR, 0.75; 95% CI, 0.62–0.90; P = 0.002). Preoperative renal dysfunction was biologically significant (OR, 2.41; 95% CI, 0.98–5.96; P = 0.056) without statistical significance. Univariate analysis of intra- and postoperative variables showed that intraoperative mean blood pressure (OR, 0.95; 95% CI, 0.91–0.99; P = 0.011), intraoperative transfusion (OR, 1.14; 95% CI, 1.07–1.21; P < 0.001), and postoperative cardiac events (OR, 10.20; 95% CI, 4.47–23.25; P < 0.001), postoperative renal failure (OR, 11.85; 95% CI, 4.98–28.21; P < 0.001), and postoperative ischemic colitis (OR, 5.85; 95% CI, 1.50–22.78; P = 0.011) were significantly associated with 30-day mortality after AAA repair.
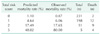
Factors showing a significant association with 30-day mortality (i.e., with P-values < 0.1 in univariate analyses) were included in the final multivariate models. The final model identified three independent predictors of 30-day mortality after AAA repair. The constant of the scoring system was defined as an increase in 30-day mortality in regression units associated with the location of the AAA (supra- or juxta-renal location: 1 point; OR, 5.02; 95% CI, 2.10–12.00; P < 0.001), rupture of AAA (ruptured AAA: 1 point; OR, 6.62; 95% CI, 2.71–16.19; P < 0.001), and preoperative pulmonary dysfunction (pulmonary dysfunction: 1 point; OR, 4.36; 95% CI, 1.79–10.64; P = 0.001) (Table 3). For each predictive factor, the distance from the base category in regression coefficient units was divided by this constant and rounded to the nearest integer to determine a point value. The final multivariate model was assessed for discrimination (c statistic, 0.811) and calibration (the Hosmer-Lemeshow test, P = 0.793).
The risk for each patient was calculated by adding the points assigned to each risk factor identified in the patient, thereby giving the total score for the patient. Table 4 shows the observed and predicted mortality rates corresponding to different total risk scores. When we compared the observed 30-day mortality rate with that predicted by our new risk score, we found that they did not differ significantly. The predicted and observed 30-day mortality rates were, respectively, 1.10% and 0.87% for patients with 0 points, 4.64% and 6.06% for patients with one point, 17.49% and 17.65% for patients with two points, and 48.02% and 80.00% for patients with 3 points, suggesting that this model was a good predictor of risk across all risk groups, except for patients with three points (Table 4). Additionally, this model was also a good predictor of risk, according to the treatment modalities (open or endovascular AAA repair) (Table 5).
Open repair of an infrarenal AAA is associated with considerably higher perioperative mortality than EVAR, which has increased the popularity of the endovascular approach in these aneurysms. However, most surgeons still perform open AAA repairs when the anatomy does not favor the use of EVAR, and occasionally EVAR may be converted to open repair during or after the repair due to technical failure on deployment, inappropriate stent-graft placement, vessel rupture, or graft thrombosis [91112]. Overall rates of open conversion of up to 6% have been reported in large EVAR series, and the incidence of early conversion (<30 days after stent-graft implantation) varies from 0.3% to 5.9% in the English-language literature [1112131415]. More recent studies have reported lower rates of early conversion to open surgery, which is probably due to improvements in endograft technology and endovascular technique, better patient selection, and a tendency to treat most complications via the endovascular approach. However, the average mortality rate associated with early conversion was still as high as 12.4% (0%–28.5%) in a total of 12,236 endovascular AAA repairs [11].
For any repair procedure, whether open or endovascular, the process of informed consent requires a thorough explanation of the risks and benefits to the patient, and the risks presented by vascular surgeons to patients undergoing AAA repair are based on anecdotal experience or on currently available risk estimation tools. In the past two decades, many studies have attempted to identify factors capable of predicting death in patients undergoing open repair of AAAs, whether intact or ruptured, and various risk assessment tools are currently used to predict perioperative mortality; each model has its strengths and weaknesses [56716171819202122232425]. The existing risk-scoring models vary greatly in the nature and quality of their results, and the methods used for reporting. Although several studies have modeled statistically the predictive variables in order to design scoring systems that can forecast outcomes, many of these did not use a sound methodology, and only a few having undergone robust testing, let alone prospective validation.
A new risk-scoring model should be able to predict the outcomes prior to the AAA repair, rather than based on operative and postoperative findings. Furthermore, given the increasing popularity of endovascular procedures, and the moderate incidence of early conversion-related mortality, it is reasonable that a new risk-scoring model should include patients undergoing both open and endovascular AAA repair. A new model should also be easy to use to enable rapid application by any grade of medical staff, and generate the most accurate risk score from the smallest number of variables, in an elective and urgent setting. To date, the quality and level of available evidence has been insufficient to make such a model a reality.
The goal of our model was to predict final outcomes based on preoperative findings, to do fairly straightforwardly, and to reflect the changes in preferred treatment modality. With this in mind, we incorporated the type of repair (open or endovascular) and the available preoperative patient characteristics into our model, and assigned an independent weight to each to calculate the overall risk. We found that supra-/juxta-renal location of the AAA, rupture of AAA, and preoperative pulmonary dysfunction were independent predictors of 30-day mortality. When we compared the observed 30-day mortality rates with those expected from our new risk score, we found that they did not differ significantly, which showed that our model had good predictive power across all risk groups, except for patients with three points.
Our model has several limitations, including the retrospective assessment of patients and inclusion of limited information; other factors, e.g., data that are not collected routinely, may also affect patient outcomes. Another limitation is the single center nature and a long period of data collection of this study that were factors likely to limit external validity of this model. Also, the numbers of patients who underwent endovascular repair (33.0%) were relatively small, and this may not have been sufficient to make accurate predictions. Furthermore, because of extremely small number of patients with three points, we cannot validate predictive power of our model for these patients. The model also requires validation, preferably using larger data sets from throughout the world.
In conclusion, we have developed a new risk estimation tool to predict postoperative mortality associated with open and endovascular AAA repair. With its high discriminative ability, this model is a step toward improving preoperative decision-making and the informed consent process in an era when endovascular procedures are increasingly common. Further studies are needed to validate this tool using larger and more varied samples.
Figures and Tables
Table 3
Multivariate analysis of factors associated with 30-day mortality after AAA repair, and summary of a new scoring system

References
1. Henebiens M, Vahl A, Koelemay MJ. Elective surgery of abdominal aortic aneurysms in octogenarians: a systematic review. J Vasc Surg. 2008; 47:676–681.
2. Wilmink TB, Quick CR, Hubbard CS, Day NE. The influence of screening on the incidence of ruptured abdominal aortic aneurysms. J Vasc Surg. 1999; 30:203–208.
3. Grant SW, Grayson AD, Purkayastha D, Wilson SD, McCollum C. participants in the Vascular Governance North West Programme. Logistic risk model for mortality following elective abdominal aortic aneurysm repair. Br J Surg. 2011; 98:652–658.
4. Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J. 2003; 24:881–882.
5. Robinson WP, Schanzer A, Li Y, Goodney PP, Nolan BW, Eslami MH, et al. Derivation and validation of a practical risk score for prediction of mortality after open repair of ruptured abdominal aortic aneurysms in a US regional cohort and comparison to existing scoring systems. J Vasc Surg. 2013; 57:354–361.
6. Samy AK, Murray G, MacBain G. Glasgow aneurysm score. Cardiovasc Surg. 1994; 2:41–44.
7. Patterson BO, Karthikesalingam A, Hinchliffe RJ, Loftus IM, Thompson MM, Holt PJ. The Glasgow Aneurysm Score does not predict mortality after open abdominal aortic aneurysm in the era of endovascular aneurysm repair. J Vasc Surg. 2011; 54:353–357.
8. Baas AF, Janssen KJ, Prinssen M, Buskens E, Blankensteijn JD. The Glasgow Aneurysm Score as a tool to predict 30-day and 2-year mortality in the patients from the Dutch Randomized Endovascular Aneurysm Management trial. J Vasc Surg. 2008; 47:277–281.
9. Ramanan B, Gupta PK, Sundaram A, Gupta H, Johanning JM, Lynch TG, et al. Development of a risk index for prediction of mortality after open aortic aneurysm repair. J Vasc Surg. 2013; 58:871–878.
10. Sullivan LM, Massaro JM, D'Agostino RB Sr. Presentation of multivariate data for clinical use: The Framingham Study risk score functions. Stat Med. 2004; 23:1631–1660.
11. Moulakakis KG, Dalainas I, Mylonas S, Giannakopoulos TG, Avgerinos ED, Liapis CD. Conversion to open repair after endografting for abdominal aortic aneurysm: a review of causes, incidence, results, and surgical techniques of reconstruction. J Endovasc Ther. 2010; 17:694–702.
12. Ferrero E, Ferri M, Viazzo A, Pecchio A, Berardi G, Piazza S, et al. Open conversion after endovascular aortic aneurysm repair: a single-center experience. Ann Vasc Surg. 2013; 27:856–864.
13. Hobo R, Buth J. EUROSTAR collaborators. Secondary interventions following endovascular abdominal aortic aneurysm repair using current endografts. A EUROSTAR report. J Vasc Surg. 2006; 43:896–902.
14. Ouriel K, Clair DG, Greenberg RK, Lyden SP, O'Hara PJ, Sarac TP, et al. Endovascular repair of abdominal aortic aneurysms: device-specific outcome. J Vasc Surg. 2003; 37:991–998.
15. Sampram ES, Karafa MT, Mascha EJ, Clair DG, Greenberg RK, Lyden SP, et al. Nature, frequency, and predictors of secondary procedures after endovascular repair of abdominal aortic aneurysm. J Vasc Surg. 2003; 37:930–937.
16. Prance SE, Wilson YG, Cosgrove CM, Walker AJ, Wilkins DC, Ashley S. Ruptured abdominal aortic aneurysms: selecting patients for surgery. Eur J Vasc Endovasc Surg. 1999; 17:129–132.
17. Neary WD, Crow P, Foy C, Prytherch D, Heather BP, Earnshaw JJ. Comparison of POSSUM scoring and the Hardman Index in selection of patients for repair of ruptured abdominal aortic aneurysm. Br J Surg. 2003; 90:421–425.
18. Boyle JR, Gibbs PJ, King D, Shearman CP, Raptis S, Phillips MJ. Predicting outcome in ruptured abdominal aortic aneurysm: a prospective study of 100 consecutive cases. Eur J Vasc Endovasc Surg. 2003; 26:607–611.
19. Tambyraja AL, Fraser SC, Murie JA, Chalmers RT. Validity of the Glasgow Aneurysm Score and the Hardman Index in predicting outcome after ruptured abdominal aortic aneurysm repair. Br J Surg. 2005; 92:570–573.
20. Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991; 78:355–360.
21. Prytherch DR, Ridler BM, Beard JD, Earnshaw JJ. Audit and Research Committee, The Vascular Surgical Society of Great Britian and Ireland. A model for national outcome audit in vascular surgery. Eur J Vasc Endovasc Surg. 2001; 21:477–483.
22. Steyerberg EW, Kievit J, de Mol Van Otterloo JC, van Bockel JH, Eijkemans MJ, Habbema JD. Perioperative mortality of elective abdominal aortic aneurysm surgery. A clinical prediction rule based on literature and individual patient data. Arch Intern Med. 1995; 155:1998–2004.
23. Brady AR, Fowkes FG, Greenhalgh RM, Powell JT, Ruckley CV, Thompson SG. Risk factors for postoperative death following elective surgical repair of abdominal aortic aneurysm: results from the UK Small Aneurysm Trial. On behalf of the UK Small Aneurysm Trial participants. Br J Surg. 2000; 87:742–749.
24. Kertai MD, Steyerberg EW, Boersma E, Bax JJ, Vergouwe Y, van Urk H, et al. Validation of two risk models for perioperative mortality in patients undergoing elective abdominal aortic aneurysm surgery. Vasc Endovascular Surg. 2003; 37:13–21.
25. Baek JK, Kwon H, Ko GY, Kim MJ, Han Y, Chung YS, et al. Impact of graft composition on the systemic inflammatory response after an elective repair of an abdominal aortic aneurysm. Ann Surg Treat Res. 2015; 88:21–27.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download