Abstract
Purpose
I investigated the diagnostic accuracy of balloon expulsion test (BET) with various techniques to find out the most appropriate method, and tried to confirm its clinical utility in diagnosing functional defecation disorders (FDD) in constipated patients.
Methods
Eighty-seven patients constituted the study population. FDD was defined when patients had at least two positive findings in defecography, manometry, and electromyography. BET was done 4 times in each patient with 2 different positions and 2 different volumes. The positions were seated position (SP) and left lateral decubitus position (LDP). The volumes were fixed volume (FV) of 60 mL and individualized volume with which patient felt a constant desire to defecate (CDV). The results of BETs with 4 different settings (LDP-FV, LDP-CDV, SP-FV, and SP-CDV) were statistically compared and analyzed.
Results
Of 87 patients, 23 patients (26.4%) had at least two positive findings in 3 tests and thus were diagnosed to have FDD. On receiver operating characteristic curve analysis, area under curve was highest in BET with SP-FV. With a cutoff value of 30 seconds, the specificity of BET with SP-FV was 86.0%, sensitivity was 73.9%, negative predictive value was 89.8%, positive predictive value was 65.4%, and accuracy rate was 82.8% for diagnosing FDD.
Chronic constipation is a symptom-based disorder of unsatisfactory defecation, which has mostly functional etiology. Rome III Committee defined functional constipation as the occurrence of two or more of the following symptoms: (1) straining during at least 25% of defecations, (2) lumpy or hard stools in at least 25% of defecations, (3) sensation of incomplete evacuation for at least 25% of defecations, (4) sensation of anorectal obstruction/blockage for at least 25% of defecations, (5) manual maneuvers to facilitate at least 25% of defecations (e.g., digital evacuation, support of the pelvic floor), (6) fewer than three defecations per week. They also defined functional defecation disorders (FDD) as a subtype of functional constipation, which include dyssynergic defecation and inadequate defecatory propulsion. According to Rome III criteria, FDD should have objective findings of at least two of following in addition to above symptoms: (1) Impaired evacuation, based on balloon expulsion test (BET) or imaging, (2) Inappropriate contraction of the pelvic floor muscles assessed by manometry, imaging, or electromyography (EMG), (3) Inadequate propulsive forces assessed by manometry or imaging [1].
BET is a simple procedure to identify functional pelvic outlet obstruction. Although other physiologic tests such as defecography, manometry, and EMG are preferred to diagnose such obstruction because of the ability to define structural abnormality or the alleged accuracy in differentiating subtypes of impaired evacuation, BET has its own merits that it is technically easy to perform and do not require expensive instruments. Thus, as shown in Rome III criteria of FDD, it has been recommended to include BET in diagnostic workup for chronic constipation and use it as a screening tool for FDD. However, its technical methodology has not been well established and its clinical utility has not been clearly defined compared to other physiologic tests. Several techniques have been used without standardization in the type of balloon, instilled material, filling volume, and expelling position.
In this study, I investigated the diagnostic accuracy of BET with various techniques to find out the most appropriate method of BET, especially related to filling volume and expelling position, and I attempted to confirm the clinical utility of BET for diagnosing FDD in patients with chronic constipation.
Among patients with chronic constipation who visited the anorectal physiology unit in Konkuk University Medical Center from March 2013 to March 2015, those who agreed to the purpose of this study were included, but those with drug-induced or organic lesion-associated constipation were excluded. Eighty-seven (mean age, 57.3 years; range, 20 to 88 years; 46 females, 41 males) patients constituted the final study population. They completed work-up of their symptoms with BET, defecography, manometry and EMG. Chronic constipation was defined according to the Rome III criteria of functional constipation. FDD were defined as the occurrence of at least two positive findings in defecography, manometry, and EMG. All the process of this study was approved by the Institutional Review Board at Konkuk University Medical Center (KUH 1020060).
BET was done 4 times in each patient with 2 different positions and 2 different volumes. The positions were left lateral decubitus position (LDP) on a bed and seated position (SP) on a commode. The volumes were fixed volume (FV) of 60 mL and individualized volume with which patient felt constant desire to defecate (CDV). Thus, there were 4 kinds of technical setting; LDP-FV, LDP-CDV, SP-FV, and SP-CDV in order of performance. A 5 cm-sized party balloon tied to the tip of a plastic catheter of 5 mm in external diameter was inserted into the rectum. Tepid water was instilled to fill the balloon for FV or CDV with a syringe via a 3 way stopcock attached to the opposite tip of the catheter. Instillation for CDV was stopped at 300 mL maximally. After inflating the balloon, patients were asked to expel the balloon. The time required to expell the balloon was checked. It was stopped when the time was over 3 minutes.
Defecographic examination was done by a radiologic technician. With patient in LDP, liquid barium of 50 mL was inserted into the rectum using a catheter syringe. For female patients, the vaginal wall was coated with an appropriate amount of water-soluble contrast. After barium paste was inserted until patient felt constant desire to defecate, the patient was asked to sit down on a specially-designed commode and pose in their usual SP for defecation. Dynamic image of fluoroscopy was obtained while the patient was trying to evacuate the rectum. The result was read as positive when there was poor emptying of the rectum with poor opening of the anal canal and/or persistent posterior angulation of the rectum. Poor emptying with structural changes such as rectocele or intussusception, but without poor opening or persistent angulation were read as negative [2]. All these findings were evaluated with dynamic image.
Manometry was performed using a water-perfused catheter with 8 channels attached to a hydraulic capillary infusion system (Medtronics, Minneapolis, MN, USA). The catheter was 4.5 mm in diameter with side-holes of 0.8 mm in diameter. Side-holes of each channel were spirally aligned with 7 mm intervals along the longitudinal axis. Examination was performed in LDP. After calibrating the system, the catheter was inserted into the anal canal until the most distal side-hole was located at the anal verge. While the catheter was in position, pressures of the rectum and the anal canal were measured simultaneously at squeeze and push (simulated evacuation) with intervening resting period. Anal channels were distinguished from rectal channels by pressure change during squeeze. Manometric finding was interpreted with patterns of pressure change in the rectum and anal canal during push (Fig. 1). It was regarded as positive when there was one of the following dyssynergic patterns with manometric defecation index (MDI) of less than 1.0; adequate increase in rectal pressure with paradoxical increase in anal pressure (type I), inadequate increase in rectal pressure with paradoxical increase in anal pressure (type II), adequate increase in rectal pressure with incomplete reduction in anal pressure (type III), or inadequate increase in rectal pressure with incomplete reduction in anal pressure (type IV). MDI was defined by dividing maximal rectal pressure into minimal anal pressure during push [3].
EMG was done with patient in SP. An anal electrode of plug type was inserted into the anal canal and another electrode of surface type was attached to the abdominal wall. After patient accommodated to the sensation of having a plug in the anal canal, EMG was recorded by a biofeedback system (HMT2000, HMT Inc., Seoul, Korea) at rest, squeeze, and push. EMG finding was regarded as positive when paradoxical contraction or non-relaxation of electrical activity was present while patient was attempting to push the plug out (Fig. 2).
Statistical analysis was completed with SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) and dBSTAT ver. 5.0 (dBSTAT Inc., Seoul, Korea). Agreements among three physiologic tests (defecography, manometry and EMG) were assessed by Cohen κ coefficient. The receiver operating characteristic (ROC) curve analysis was used to analyze the results of BET with 4 different settings. Areas under curves (AUC) were calculated and compared. Statistical significance was defined by a P-value of less than 0.05.
Of 87 patients, defecographic positive findings were present in 26 patients (29.9%). Impaired rectal evacuation was present in 30 patients, in whom 4 patients did not show poor opening of the anal canal or persistent posterior angulation of the rectum, but showed findings of rectocele or rectal intussusception.
Manometric finding was positive in 31 patients (35.6%). Among them, dyssynergic pattern of type I was in 13 patients, type II was in 7, type III was in 4, and type IV was in 7 patients. All the patients with these dyssynergic patterns were with MDI of less than 1.0.
EMG finding was positive in 30 patients (34.5%). Among them, 22 patients showed paradoxical contraction, and 8 patients showed non-relaxation pattern.
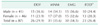
Distributions of positive findings according to gender were shown in Table 1. In total, 23 patients (26.4%) had at least two or more positive findings in three tests and thus were diagnosed to have FDD. Agreements among the three tests were poor or fair. Cohen κ coefficients were 0.1942 between defecography and manometry, 0.1069 between defecography and EMG, and 0.3157 between manometry and EMG (Table 2).
Analyzing the results of BET, AUC in ROC curves were 0.763, 0.751, 0.846, and 0.808 in order of LDP-FV, LDP-CDV, SP-FV, and SP-CDV (Fig. 3). AUC was highest in SP-FV setting. With cutoff value of 30 seconds determined from ROC curve, the specificity of BET with SP-FV was 86.0%, sensitivity was 73.9%, negative predictive value was 89.8%, positive predictive value was 65.4%, and accuracy rate was 82.8% for diagnosing FDD. Mean CDV was 192.8 mL (range, 140–300 mL).
This study shows that BET has a diagnostic accuracy sufficient to exclude FDD in patients with chronic constipation, especially when it is performed in the SP-FV (60 mL) setting. With a cutoff value of 30 seconds, the specificity of BET with SP-FV was 86.0%%, sensitivity was 73.9%, negative predictive value was 89.8%, positive predictive value was 65.4%, and accuracy rate was 82.8% for diagnosing FDD. These results are similar with a previous study that reported that the specificity was 89%, negative predictive value was 97% with BET in the SP-CDV setting and suggested BET is a useful screening procedure to identify constipated patients who do not have FDD [4].
The prevalence of FDD among patients with functional constipation has been reported variably from 8% to 74% in available studies, in which one or two physiologic tests were used to define FDD [4]. In my study, the prevalence was 26.4%. I defined FDD based on three tests (defecography, manometry and EMG), of which agreements with each other were poor or fair. Patients with at least two or more positive findings in 3 tests were considered to have FDD. For defecographic finding, poor rectal emptying with structural changes such as rectocele or rectal intussusception but without poor opening of the anal canal or persistent posterior angulation of the rectum was excluded from positivity. Manometric finding was regarded as positive when MDI was less than 1.0, although it was originally defined as such when less than 1.2 [3]. For EMG finding, only paradoxical contraction or non-relaxation pattern during simulated evacuation was regarded as positive. Any degree of relaxation, even if it is less than 20%, was considered as normal response. I believe all these criteria were so strict that FDD was not overestimated in prevalence. These would contribute to enhancing the significance of the predictive value of BET in this study.
For the management of functional constipation, the first step should be differentiating subtypes of constipation; colonic slow transit constipation and FDD, because there are some differences in therapeutic implication between them. Slow transit constipation requires colonic transit time study for the diagnosis, which takes sometimes more than 7 days to be done. Thus, initial studies are usually focused on finding FDD. When the Rome III Committee defined FDD, they suggested BET or imaging study as diagnostic tools to identify impaired rectal evacuation as a prerequisite condition for it.
BET is a simple procedure and can be performed easily without any expensive instruments. Albeit simple and inexpensive, BET was reported to have high specificity and negative predictive value as a diagnostic tool for functional outlet obstruction [4]. This means that patients with negative result do not need other onerous physiological tests to exclude FDD. With this background, it was recommended as a screening tool in patients with chronic constipation to determine who requires further specific tests. However, these observations are contrary to other studies that reported that some patients with FDD could expel the balloon or some healthy controls could not expel the balloon [56]. The prevalence of positive result in BET has also been reported variably, ranging from 23% to 67% among constipated patients [6]. One of the main reasons for such variable results is a variety of methodologies in performing the test. With different technical methods among the studies, a comparative interpretation of the reported results is problematic. Methodological standardization is mandatory to confirm the clinical utility of BET.
Although a water-filled rubber balloon was usually used as a simulated stool to expel, 18 mm spheres [7] or silicon-filled artificial stools were also used [8]. Air was instilled to fill the balloon, instead of water in some studies [6]. However, I believe that a rubber balloon is preferable to other materials because it is readily available, and water is more effective than air because it can generate weight to simulate stool. With a water-filled rubber balloon, it was filled with FV (50 or 60 mL) of water in most studies. However, it was filled with individualized CDV of water depending on the rectal sensitivity of each patient in some studies [4]. CDV is theoretically more advantageous than FV to initiate balloon expulsion, because a constant sensation of desire to defecate is necessary to start the defecatory process. In this regard, BET with FV, which is insufficient to create such sensation, could mimic an abnormal condition for expelling the balloon due to the absence of rectal perception. It may lead to the overdiagnosis of FDD. However, practical utilities of FV and CDV in BET have rarely been compared before this study.
Position of the patient during balloon expulsion was also variable among the studies. In the original description, BET was evaluated in LDP [9]. It might be due to the technical convenience to perform BET in association with anorectal manometry. Conceivably, however, LDP is not physiologically appropriate for defecatory maneuvering and gravity cannot aid in expelling the balloon in this position. This may lead to the overdiagnosis of FDD. SP is physiologically more conducive for balloon expulsion. Thus, most of the recent studies have performed BET with SP. Nevertheless, for patients with high clinical suspicion for FDD but normal BET with SP, it has been recommended to perform BET with LDP, particularly in patients with increased perineal descent, because intraabdominal pressure exerted by descending viscera could overcome pelvic floor dysfunction [10].
In this study, it was shown that BET with SP was more accurate than with LDP, and BET with FV was more accurate than with CDV. I suggest the SP-FV setting as the most appropriate method for BET. The reason why FV brings more accurate results than CDV is not obvious. It is contrary to the theoretical advantage of CDV. However, there are some tentative explanations. First, while BET with FV has a chance of overdiagnosing FDD, BET with CDV has another chance of missing FDD associated with rectal hyposensitivity. Patients with such a condition need abnormally large volume to feel the desire to defecate. Some of them can expel the balloon more easily in BET with CDV than with FV, simply because the rectum is sensitized by the volume. This may lead to missing the diagnosis of FDD. Second, as previously reported [910], some patients may feel more difficulty in expelling the balloon with larger volumes. This can be a cause of the overdiagnosis of FDD in BET with CDV. Third, FDD was defined based on the physiological tests, including manometry and EMG, which were measured with empty rectum in this study. It means that FDD had a chance of being diagnosed on the physiological background of empty rectum. In this regard, BET with FV may reflect FDD more accurately than with CDV, because it resembles the condition of empty rectum more closely than with CDV.
The normal range of balloon expulsion time has not been defined clearly. Some studies used 1 minute [1112], and others used 2 [13] or even 5 minutes [714] as the upper limit for normal range. Normal value of BET was previously reported with healthy adults [15]. According to the report, expulsion should take less than 30 seconds for men younger than 40 years of age and less than 1 minute above 40 years. For women, expulsion should occur within 1 minute regardless of age. In my study, the time was 30 seconds. It was determined as cutoff value in ROC analysis of SP-FV setting. This value is somewhat small, compared to not only the normal value mentioned above, but also the upper limit for normal range adopted by other studies. BET was repeatedly performed 4 times with an interval of a few minutes in this study. Patients might become adapted to expelling maneuver with each reiteration. Such adaptation would shorten the expelling time. BET in SP-FV setting was carried out for the third time. But there was a resting time of about 5 minutes before the third due to position change and move to commode, although it might not be enough to recover original state. For clarification about this issue, further study randomized in sequence of testing with more subjects is necessary.
In conclusion, I suggest SP-FV setting as the most appropriate method for BET. In this setting, BET has a diagnostic accuracy sufficient to identify constipated patients who do not have FDD. With a cutoff value of 30 seconds, the specificity was 86.0%, sensitivity was 73.9%, negative predictive value was 89.8%, positive predictive value was 65.4%, and accuracy rate was 82.8% for diagnosing FDD. Patients with negative results in BET with SP-FV may not need other onerous physiological tests to exclude FDD.
Figures and Tables
Fig. 1
Manometric positive finding. Upper four channels are in the rectum. Lower 4 channels are in the anal canal. Their locations can be distinguished by squeeze action. In this finding, rectal pressure increased adequately, but anal pressure also increased paradoxically by push action.

Fig. 2
Electromyographic positive finding. It consists of dual recordings. Upper graph records activity from anal electrode. It shows paradoxical contraction. Lower graph records activity from abdominal wall electrode. It shows normal contraction which means that push action is done properly.

Fig. 3
Receiver operating characteristic curves of balloon expulsion tests with different techniques. Areas under curves are 0.763, 0.751, 0.846, and 0.808 in order of LDP-FV, LDP-CDV, SP-FV, and SP-CDV. LDP-FV, lateral decubitus position and fixed volume; LDP-CDV, lateral decubitus position and constant desire to defecate volume; SP-FV, seated position and fixed volume; SP-CDV, seated position and constant desire to defecate volume.

References
1. Rome Foundation. Rome III disorders and criteria [Internet]. Raleigh (NC): Rome Foundation Inc.;c2015. cited 2015 May 10. Available from: http://www.romecriteria.org/criteria.
2. Seong MK, Kim TW. Significance of defecographic parameters in diagnosing pelvic floor dyssynergia. J Korean Surg Soc. 2013; 84:225–230.
3. Rao SS. Dyssynergic defecation. Gastroenterol Clin North Am. 2001; 30:97–114.
4. Minguez M, Herreros B, Sanchiz V, Hernandez V, Almela P, Anon R, et al. Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology. 2004; 126:57–62.
5. Rao SS, Mudipalli RS, Stessman M, Zimmerman B. Investigation of the utility of colorectal function tests and Rome II criteria in dyssynergic defecation (Anismus). Neurogastroenterol Motil. 2004; 16:589–596.
6. Rao SS, Ozturk R, Laine L. Clinical utility of diagnostic tests for constipation in adults: a systematic review. Am J Gastroenterol. 2005; 100:1605–1615.
7. Bannister JJ, Timms JM, Barfield LJ, Donnelly TC, Read NW. Physiological studies in young women with chronic constipation. Int J Colorectal Dis. 1986; 1:175–182.
8. Pelsang RE, Rao SS, Welcher K. FECOM: a new artificial stool for evaluating defecation. Am J Gastroenterol. 1999; 94:183–186.
9. Barnes PR, Lennard-Jones JE. Balloon expulsion from the rectum in constipation of different types. Gut. 1985; 26:1049–1052.
10. Ratuapli S, Bharucha AE, Harvey D, Zinsmeister AR. Comparison of rectal balloon expulsion test in seated and left lateral positions. Neurogastroenterol Motil. 2013; 25:e813–e820.
11. Rao SS, Singh S. Clinical utility of colonic and anorectal manometry in chronic constipation. J Clin Gastroenterol. 2010; 44:597–609.
12. Belkind-Gerson J, Goldstein AM, Kuo B. Balloon expulsion test as a screen for outlet obstruction in children with chronic constipation. J Pediatr Gastroenterol Nutr. 2013; 56:23–26.
13. Chiarioni G, Kim SM, Vantini I, Whitehead WE. Validation of the balloon evacuation test: reproducibility and agreement with findings from anorectal manometry and electromyography. Clin Gastroenterol Hepatol. 2014; 12:2049–2054.
14. Diamant NE, Kamm MA, Wald A, Whitehead WE. AGA technical review on anorectal testing techniques. Gastroenterology. 1999; 116:735–760.
15. Dedeli O, Turan I, Ozturk R, Bor S. Normative values of the balloon expulsion test in healthy adults. Turk J Gastroenterol. 2007; 18:177–181.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download