Abstract
Purpose
Single incision laparoscopic cholecystectomy (SILC) is generally performed with the use of inverse triangulation. In this study, we performed 3-channel or 4-channel SILC without the use of inverse triangulation. We evaluated the adequacy and feasibility of SILC using our surgical method.
Methods
We retrospectively reviewed our series of 309 SILCs performed between March 2014 and February 2015.
Results
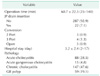
Among 309 SILCs, male were 148 and female were 161 patients, mean age was 48.7 ± 15.3 years old and mean body mass index was 24.8 ± 3.8 kg/m2. Forty patients had previously undergone abdominal surgery including 6 cases of upper abdominal surgery. SILC after percutaneous transhepatic gallbladder (GB) drainage was completed in 8.7% of cases. There were 10 cases of emergency SILC. SILC was performed for noncomplicated GB including symptomatic GB stone and polyp in 66.7% of cases, acute cholecystitis in 33.3%. Overall, 96.8% of procedures were successfully completed without additional port. The reason for addition of an extra port or open conversion included technical difficulties due to severe adhesion and bleeding. The mean operating time was 60.7 ± 22.3 minutes. The overall complication rate was 4.8%: 9 patients of wound seroma, 1 case of bile leakage from GB bed, 4 cases of intra-abdominal abscess or fluid collection, and 1 case of incisional hernia were developed. There was no case of common bile duct injury.
Laparoscopic surgery has become popular in the past decades, owing to less postoperative pain, fast recovery, and better cosmetic outcomes [1]. In particular, conventional laparoscopic cholecystectomy (CLC) has become the gold standard technique for treating benign gallbladder (GB) disease [2]. The drive toward reducing number of ports and incisions has led to the development of single incision laparoscopic surgery (SILS) techniques. Transumbilical single-incision laparoscopic cholecystectomy (SILC) was first described by Navarra et al. [3] in 1997. Many centers have introduced various procedures and instruments to overcome the complexity and the technical challenges of SILC due to the restricted degrees of freedom of movement, the number of ports that can be used, and the proximity of the instruments to each other during the procedure. However, there is currently no validated standardized SILC with regard to surgical techniques and device. Meillat et al. [4] used SILS port (Covidien, Mansfield, MA, USA), 10 mm 0° or 30° laparoscope and standard laparoscopic graspers. Beninato et al. [5] used GelPOINT device (Applied Medical, Rancho Santa Margarita, CA, USA) and conventional laparoscopic instruments. Son et al. [6] introduced hand-made ports using ALEXIS wound retractor (Applied Medical) and sterile surgical glove. These study groups performed SILC with the use of crossed-over instruments (inverse triangulation): traction of GB by surgeon's right hand and dissection of Calot's triangle and main procedure by left hand.
We performed 3-channel or 4-channel SILC using Gloveport 431 (Meditech Inframed, Seoul, Korea) without the use of inverse triangulation: traction of GB by surgeon's left hand and dissection of Calot's triangle and main procedure by right hand.
In this study, we intend to present our one year experiences of SILC, and to describe surgical technique, instruments used, and outcomes of Hallym University Sacred Heart Hospital.
We retrospectively reviewed our series of 309 SILC performed between March 2014 and February 2015. In our hospital, about 350 laparoscopic cholecystectomies have been performed per year.
Initially, the patients who have percutaneous transhepatic gallbladder drainage (PTGBD), cardiologic or pulmonologic problems, history of upper abdominal surgery and complications of acute cholecystitis were excluded. But we did not exclude patients with high body mass index (BMI). After 50 cases, as our experience had deepened, the inclusion criteria of SILC changed gradually, evolved to include all patients who would generally be considered for CLC, but we excluded the patients with high suspicion of malignancy. The operative time was defined as the interval from initial skin incision to skin closure.
We performed SILC using four-channel Gloveport 431 without the use of inverse triangulation. Data for demographic variables, clinical presentation, intraoperative data, postoperative course and pathology were obtained.
Skin incision began with a 25-mm vertical transumbilical incision. Then Gloveport 431 was introduced. After making pneumoperitoneum, the patients were placed in a reverse Trendelenburg position at an angle of 20°–30° with the right side up. We arranged the rigid telescope and endoscopic instruments. We used a rigid 10-mm 30° laparoscope (Stryker, San Jose, CA, USA), conventional dissector and one or two long articulated graspers (Covidien) for traction. In the first 2 cases, the GB was exposed by suspension using a lean back method to get good critical view of safety [7]. In case of noncomplicated GB, 3 channels among 4 channels were used and in case of complicated cholecystitis, all of 4 channel were used (Figs. 1, 2). The camera was positioned through channel A. The GB was retracted laterally with a grasper using the surgeon's left hand through channel B and the anterior peritoneum surrounding the cystic duct was dissected by a conventional dissector using the surgeon's right hand through channel C. This was followed by the posterior dissection using the surgeon's right hand dissector. After isolating the cystic duct and artery, we ligated them using 5-mm or 10-mm metal clips and 10 mm Hem-O-Lok (Weck Closure Systems, a division of Teleflex Inc., Wayne, PA, USA) and then divided them. Following the dissection of the GB from the GB bed, the GB was removed through the pouch (Fig. 3). Then, we performed an irrigation using a suctionhook bovie (Endopath Probe Plus II Pistol Grip Handle, Ethicon EndoSurgery Inc., Cincinnati, OH, USA). A careful fascial incision closure was performed with an interrupted absorbable suture, and the umbilicus was restored to its physiological position using absorbable intracutaneous stitches.
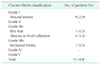
In the current study, we performed a retrospective analysis of demographic characteristics of the patients. These characteristics include age, gender, BMI, a past history of abdominal operation, the American Society of Anesthesiologists scores, preoperative PTGBD insertion, operation time, drainage insertion, length of hospital stay, histopathologic findings, conversion to open or conventional laparoscopic surgery (CLS) and postoperative complications. All the complications were recorded according to the Clavien-Dindo classification [8].
A total of 309 patients (161 women and 148 men) with a mean age of 48.7 ± 15.3 years (range, 15–88 years) underwent SILC without the use of inverse triangulation during the study period. The mean BMI was 24.8 ± 3.8 kg/m2 (range 14.8–42.4 kg/m2). Forty patients had a history of previous abdominal surgery. Among the 40 patients, 6 (15%) underwent upper abdominal surgery. Twenty-seven patients (8.7%) were treated with PTGBD procedure before SILC (Table 1).
The mean operation time was 60.7 ± 22.3 minutes (range, 25–140 minutes), and the mean hospital stay was 3.2 ± 2.4 days (range, 2–17 days). SILC were performed for noncomplicated GB including stone and polyp in 206 patients (66.7%), acute cholecystitis in 88 patients (28.5%) and acute gangrenous cholecystitis in 15 patients (4.8%). There were 10 cases of Emergency SILC. Overall, 299 patients (96.8%) were successfully completed without additional port. Conversions to CLC that required additional ports were 7 cases (2.3%). There were 3 cases (0.9%) of subcostal laparotomy. The reason for addition of an extra port included technical difficulties due to acute inflammation and inadequate exposure. Conversion to open cholecystectomy was due to severe adhesion and bleeding. In 22 patients (7.1%), Jackson-Pratt drain was placed in the subhepatic area (Table 2).
The overall complications were observed in a total of 15 patients (4.8%) (Table 3). Grade I wound seroma developed in 9 patients (2.9%). Five patients (1.6%) presented grade IIIa complications: 1 case of bile leakage from GB bed that was controlled well by endoscopic retrograde biliary drainage stent insertion, and 4 cases of intra-abdominal abscess or fluid collections that were managed by Pigtail insertion. And there was one case of incisional hernia (grade IIIb). There were no mortalities or common bile duct injuries.
The effort toward reducing the number of ports needed for CLS has led to the development of SILS [910]. One current goal of SILC is to perform laparoscopic procedures successfully and safely. Our study did not aim to prove that SILC is better than CLC, but we aimed to show that it is feasible and safe and thus may be used as an alternative technique.
Since Navarra et al. [3] reported SILC in 1997, various multilumen ports that allow simultaneous multiple instrument insertion including the SILS port, ASC Triport (Advanced Surgical Concept, Wicklow, Ireland) and the GelPOINT device, angled or flexible scopes, articulated instruments and instruments of variable length have been introduced [4511]. Son et al. [6] used a hand-made port for SILC using the ALEXIS wound retractor (Applied Medical) and sterile surgical gloves. In the previous study using these devices, SILC procedures did not allow for normal triangulation. They used an inverse triangulation technique; surgeons used their right hand for traction and left hand for main surgery including dissection. This is the major technical difficulty of SILC.
To enhance the visualization of the critical view of safety during SILC, Tay et al. [12] used extracorporeal hanging suture, which is used to pierce the GB fundus at the seromuscular plane. You et al. [7] introduced lean back technique, which is used to suture between the parietal peritoneum at right diaphragm and GB fundus intracorporeally. And Sung et al. [13] used a snake retractor.
A universal goal of any new technique should be its reproducibility by other surgeons. This will enhance its applicability by large numbers of surgeons and to large numbers of patients requiring cholecystectomy. In this study, we performed 3- or 4-channel SILC using Gloveport 431 that has several advantages without the use of inverse triangulation: traction of GB by surgeon's left hand and main procedure including dissection of Calot's triangle by right hand. Gloveport 431 is a flexible SILS system, easy to use and can be simply accommodated to the abdominal wall. Because it allows combined motions in linear, radial, and translational planes, the instruments can be used apart, relatively easily crossed or rotated as required in any situation. Also, Gloveport 431 has a pouch, which is a built-in wound protecting specimen retrieval system (Fig. 3).
Initially, the inclusion criteria of SILC was limited to surgical patients with symptomatic GB stones or polyp. After performing 50 cases of SILC, as our experience broadened, we applied SILC to all patients who would typically be considered for CLC. In case of minimal signs of inflammation of GB or GB polyp, we used 3-channel among 4-channel SILC. In cases where the patient had large distended GB, thickened GB wall, or adhesions around Calot's triangle, and the anatomy of the critical view of safety was difficult to discern, the 4-channel approach was taken. We preferred transumbilical incision. Some authors suggest that the distance between umbilical port and the GB increases with height and obesity [14]. Consequently, it is more difficult to place the scope and grasper near to the operative field, leading to more struggle and longer operations [4]. In this study, SILC was very difficult when the distance between umbilicus and rib costal margin was more than 17 cm. In such cases we made a vertical incision on the supra-umbilical area.
In our series, we performed SILC using one long articulated grasper (Roticulator, Covidien) by surgeon's left hand, rigid 10-mm 30° telescope by assistant, and conventional laparoscopic dissector or Hem-O-Lok clip applier by surgeon's right hand during 3-channel SILC (Fig. 1). In case of 4-channel SILC, we used one long articulated grasper by surgeon's left hand and conventional laparoscopic dissector or Hem-O-Lok clip applier by surgeon's right hand. The assistant controlled the 10-mm 30° rigid telescope and another long articulated grasper, which was located below the rigid telescope (Fig. 2). Of importance, conventional laparoscopic dissector, scissor, and Hem-O-Lok clip applier were inserted through channel C by the right side of the rigid telescope.
Our study demonstrated that the operating time of SILC was more than 98.2 minutes at the beginning of surgery (first 10 cases). We were able to achieve a mean operating time below 65 minutes after 50 cases of SILC. In the present study, the mean operating time was 60.7 ± 22.3 minutes, which is within the reported range of recently published works [15]. In metaanalysis study, the median operating time was 80.75 minutes (range, 40–186 minutes) [16]. Antoniou et al. [17] reported that the mean operating time was 70.2 minutes in a systemic review that involved 29 studies. However, most of the studies included were the early experiences of surgeons performing SILC. Our study showed 25 patients (8.1%) experienced a prolonged surgical procedure of more than 100 minutes. Eight cases among them developed in the early stages of SILC, before the 40th case. Son et al. [6] reported that the mean operating time was 53.1 ± 25.4 minutes (range, 10–320 minutes) in 307 SILCs including patients with acute cholecystitis, high BMI, and previous upper abdominal surgery. But whether the time for preparing glove ports was included in their study was not described [6]. Generally, it is obvious that SILC will take a longer time, compared to CLC, because of the restricted degrees of freedom of movement and frequent collision of instruments [18]. However, Hernandez et al. [19] and Tay et al. [12] found that mean operative time of SILC was not significantly longer than CLC. Our study showed that mean operative time continues to decrease as experience increases. The mean operating time of 1st–100th cases, 101st–200th, and 201st–300th were 70.1, 59.3, and 52.6 minutes, respectively. We could find there was a trend toward reduced operative times with more experience in our series. So, we think the mean operative time of SILC can be overcome as surgical experiences increase.
Requiring an additional port was reported as 9.3%–14.5% of patients. Conversion to open cholecystectomy was reported as 0.4%–0.9% [417]. In our study, BMI were more than 30 kg/m2 in 28 cases of patients (9.1%), there were 103 cases (33.3 %) of acute cholecystitis including gangrenous type, and 40 cases (12.9%) had previous abdominal surgery including 6 upper abdominal surgeries. There were 7 cases (2.3%) that required additional port to aid dissection of Calot's triangle due to dense adhesion, and 3 cases (0.9%) of open conversion due to dense adhesion and bleeding. We think that low threshold of procedure conversion at an early operation stage is critical to patient safety. Considering the number of patients with high BMI, acute cholecystitis, and history of upper abdominal surgery, our result of additional port or open conversion is consistent with reported data. With regard to learning curve, the minimum number of accomplished procedures needed to pass through the learning curve of SILC was 20 in most studies [15]. In this study, the first 5 cases requiring additional port developed in the early stages of SILC, before the 40th case. The next case was 224th case. First open conversion was 197th case. Considering operative time and additional port, we believe SILC learning curve would be about 40–50 cases.
Hall et al. [16] reported a meta-analysis data including 7 randomized trials and 11 case-matched control series (compared with SLC), the overall median complication rate was 7.37% (range, 0%–28.6%), and the overall rate of biliary duct complications was 0.39%. Consistent with this report, our overall complication rate was 4.8%. We have had no case of bile duct injury yet. However, the widespread application of SILC may have led to the rise in the incidence of bile duct injury. So, larger series of cases are required to reach significance.
Port site hernia has been a concern after performing SILC in the literature [2021]. Goel and Lomanto [22] concluded in their review that port site hernia in SILS can be minimized with good suture closure of the fascial defect. We closed all umbilical fascial defects with absorbable interrupted sutures. We had one incisional hernia (0.3%) in this study after 5 to 17 months of follow-up. We repaired incisional hernia using dual mesh. However, given the relatively short-term follow-up of this study, more long-term data are needed for accurate determination of the relative recurrence rate of incisional hernia when compared with CLC.
The apparent benefits of transumbilical SILC are cosmesis and patient satisfaction [1623]. In the current era where a high premium is placed on cosmesis, patient request for improved cosmesis will impel surgeons toward the application of SILC. So, it is likely that SILC will see an increased demand. However, alone, the cosmetic advantage does not justify the performance of SILC on a routine basis. We think that patient safety should be emphasized. To further investigate these benefits, randomized trials are needed to assess patient outcomes.
In conclusion, we provide an alternative access system using Gloveport 431 to allow for SILC. According to our experiences, SILC using Gloveport 431 without the use of inverse triangulation has been demonstrated to be feasible, effective, and safe for the patient. We believe that this Gloveport 431 system is one way to lessen the technical difficulties of performing SILC and therefore broaden its applicability to other procedures.
Figures and Tables
Fig. 1
(A) Port placement for 3-channel single incision laparoscopic cholecystectomy (SILC) using a Gloveport 431 (Meditech Inframed, Seoul, Korea). Camera (a), long articulated grasper for gallbladder traction by operator left hand (b), Hem-O-Lok clip applier (Weck Closure Systems, PA, USA) by operator right hand (c), not used (d). (B). Placement of instruments during 3-channel SILC: Note that Hem-O-Lok applier in operator right hand and long articulated grasper in left hand. (C) Visualization of the cystic duct after applying Hem-O-Lok and cystic artery.

Fig. 2
(A) Port placement for 4-channel single incision laparoscopic cholecystectomy (SILC) using a Gloveport 431 (Meditech Inframed, Seoul, Korea). Camera (a), long articulated grasper for gallbladder (GB) fundus traction by assistant hand (b), dissector by operator right hand (c), long articulated grasper for GB neck traction by operator left hand (d). (B) Placement of instruments during 4-channel SILC: Note that long articulated grasper for GB fundus traction by assistant hand below camera, dissector in operator right hand and long articulated grasper in operator lefthand. (C) Visualization of GB neck traction and dissection.

Fig. 3
Gloveport 431 (Meditech Inframed, Seoul, Korea) has a pouch which is built-in wound protecting specimen retrieval system.

References
1. Mesas Burgos C, Ghaffarpour N, Almstrom M. Single-site incision laparoscopic cholecystectomy in children: a single-center initial experience. J Pediatr Surg. 2011; 46:2421–2425.
2. Kaiser AM, Corman ML. History of laparoscopy. Surg Oncol Clin N Am. 2001; 10:483–492.
3. Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997; 84:695.
4. Meillat H, Birnbaum DJ, Fara R, Mancini J, Berdah S, Bege T. Do height and weight affect the feasibility of single-incision laparoscopic cholecystectomy? Surg Endosc. 2015; 29:3594–3599.
5. Beninato T, Kleiman DA, Soni A, Nissan DA, Filicori F, Servais EL, et al. Expanding the indications for single-incision laparoscopic cholecystectomy to all patients with biliary disease: is it safe? Surg Laparosc Endosc Percutan Tech. 2015; 25:10–14.
6. Son JI, Choi IS, Moon JI, Ra YM, Lee SE, Choi WJ, et al. Single incision laparoscopic cholecystectomy using Konyang Standard Method. Ann Surg Treat Res. 2014; 86:177–183.
7. You KC, Yoo T, Park SG, Kang HJ, Pak KH, Kim JY, et al. How to do single-port laparoscopic cholecystectomy using LEAN BACK technique. ANZ J Surg. 2015; 85:284–285.
8. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196.
9. Tacchino R, Greco F, Matera D. Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc. 2009; 23:896–899.
10. Shussman N, Schlager A, Elazary R, Khalaileh A, Keidar A, Talamini M, et al. Single-incision laparoscopic cholecystectomy: lessons learned for success. Surg Endosc. 2011; 25:404–407.
11. Langwieler TE, Nimmesgern T, Back M. Single-port access in laparoscopic cholecystectomy. Surg Endosc. 2009; 23:1138–1141.
12. Tay CW, Shen L, Hartman M, Iyer SG, Madhavan K, Chang SK. SILC for SILC: single institution learning curve for single-incision laparoscopic cholecystectomy. Minim Invasive Surg. 2013; 2013:381628.
13. Sung NS, Choi IS, Moon JI, Ra YM, Lee SE, Choi WJ. Four-channel single incision laparoscopic cholecystectomy using a snake retractor: comparison between 3-and 4-channel SILC 4-channel single incision cholecystectomy. Ann Surg Treat Res. 2014; 87:81–86.
14. Hussien M, Appadurai IR, Delicata RJ, Carey PD. Laparoscopic cholecystectomy in the grossly obese: 4 years experience and review of literature. HPB (Oxford). 2002; 4:157–161.
15. Chuang SH, Yang WJ, Chang CM, Lin CS, Yeh MC. Is routine single-incision laparoscopic cholecystectomy feasible? A retrospective observational study. Am J Surg. 2015; 210:315–321.
16. Hall TC, Dennison AR, Bilku DK, Metcalfe MS, Garcea G. Single-incision laparoscopic cholecystectomy: a systematic review. Arch Surg. 2012; 147:657–666.
17. Antoniou SA, Pointner R, Granderath FA. Single-incision laparoscopic cholecystectomy: a systematic review. Surg Endosc. 2011; 25:367–377.
18. Song RY, Jung K. Early experiences of single incision laparoscopic surgery in pediatrics in a single center. J Korean Assoc Pediatr Surg. 2013; 19:90–97.
19. Hernandez J, Ross S, Morton C, McFarlin K, Dahal S, Golkar F, et al. The learning curve of laparoendoscopic single-site (LESS) cholecystectomy: definable, short, and safe. J Am Coll Surg. 2010; 211:652–657.
20. Krajinovic K, Ickrath P, Germer CT, Reibetanz J. Trocar-site hernia after singleport cholecystectomy: not an exceptional complication? J Laparoendosc Adv Surg Tech A. 2011; 21:919–921.
21. Trastulli S, Cirocchi R, Desiderio J, Guarino S, Santoro A, Parisi A, et al. Systematic review and meta-analysis of randomized clinical trials comparing single-incision versus conventional laparoscopic cholecystectomy. Br J Surg. 2013; 100:191–208.
22. Goel R, Lomanto D. Controversies in single-port laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2012; 22:380–382.
23. Burjonrappa SC, Nerkar H. Teaching single-incision laparoscopic appendectomy in pediatric patients. JSLS. 2012; 16:619–622.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download