Abstract
Purpose
To assess the relationship between the kinetics of the serum CA15-3 level and the five-year disease-free survival rate of breast cancer patients.
Methods
The subjects of this study, 297 women who were diagnosed with breast cancer, were the subset of patients operated on at Kosin University Gospel Hospital from January 2008 to December 2010. We evaluated the change of serum CA15-3 levels during outpatient follow-up period. The changing patterns of serum CA15-3 level were divided into 5 categories; surge without decline, surge with incidental decline, decline without surge, decline with incidental surge, and no change. Clinicopathologic factors were evaluated for each group.
Results
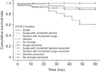
The number of patients in surge without decline, surge with incidental decline, decline without surge, decline with incidental surge, and no changes groups were 30 (10.1%), 85 (28.6%), 80 (26.9%), 73 (24.6%), and 29 (9.7%), respectively. The clinicopathologic characteristics were not significantly different among these groups. The log rank test found that 5-year disease-free survival rate according to the kinetics of serum CA15-3 levels were significant (P = 0.004) particularly for the surge without decline group.
In recent years, the prognostic value of changes in serum level of CA15-3 for breast cancer has gained much attention [1234567]. For many cancers, serum tumor markers play important roles in early diagnosis, determining prognosis, predicting response to specific therapies, the early detection of recurrence after curative surgery, and the monitoring of therapy for patients with advanced disease [89101112]. The most widely used serum tumor markers of breast cancer are CA15-3 and CEA [1211]. CA15-3 is a glycoprotein that is secreted by breast cancer cells. CA15-3 can be measured by reactivity with two monoclonal antibodies, DF3 (raised against a membrane-enriched fraction of human breast carcinoma) and 115D8 (raised against antigens of human milk fat globule membrane) [1113]. While the level of CA15-3 is rarely elevated for patients with early stage or localized cancer, the majority of patients with metastatic breast carcinoma have shown elevated serum levels of CA15-3 [11141516]. In the absence of measurable lesion(s), however, an increasing CA15-3 level may be used to indicate treatment failure [28]. More attention should be given to the interpretation of rising CA15-3 levels during the first 4–6 weeks of a new therapy because spurious early rises might occur [7817181920]. The transient elevation of CA15-3 that is affected by chemotherapy and is followed by a decrease of CA15-3 (CA15-3 surge with decline) might result in inappropriate early discontinuation or change of chemotherapy [8111921]. We also evaluated the serum CA15-3 kinetics and 5-year disease-free survival of postoperative breast cancer patients to determine the prognostic value of the changing pattern in CA15-3.
This study includes 297 patients who received operation at Kosin University Gospel Hospital from June 2008 to June 2010. The authors obtained patient medical records such as clinicopathologic factors and clinical data with serial levels of the serum CA15-3 during the follow-up period. This study employed the criteria that were used in Reporting Recommendations for Tumor Marker Prognostic Studies. Patients in the data set were categorized into 5 groups by the changing pattern of CA15-3 during the follow-up period. In group 1 (surge without decline), serum tumor marker increased continuously during the followup period. In group 2 (surge with incidental decline), incidental decline of serum tumor marker was followed by subsequent continuous surge. Patients in group 3 (decline without surge) showed continuous serum tumor marker decrease during the follow-up period. In group 4 (decline with incidental surge), incidental surge of the CA15-3 level was followed by subsequent continuous decline. Lastly, patients in group 5 (no changes) showed less than 10% change in the level of serum CA15-3. This study defines the surge of CA15-3 as an increment of CA15-3 by 10% or higher from preoperative baseline. When CA15-3 decreases by 10% or higher from the preoperative level, it is defined as the decline of CA15-3. To measure the TNM stage, this study used the criteria that were developed at the sixth American Joint Committee on Cancer. ER and PR positivities were defined as tumors with 1% or less of nuclear-stained cells. The first day of follow-up was considered as the day when pathological diagnosis was performed for the first time. Clinical follow-up was carried out every 6 or 12 months, which includes physical examination, laboratory tests of CA15-3, chest radiography, breast and liver ultrasonography, and bone scan. Five-year disease-free survival rate (5Y DFS) was measured as the time period from surgery to the occurrence of an event such as locoregional recurrence, distant metastasis, or death without recurrence. Locoregional recurrence was defined as pathologically confirmed relapse that is found on the chest wall, supra- and infraclavicular fossa, axillary area, or internal mammary region. Distant metastasis was confirmed by using radionuclear imaging modality, and pathology assessment if needed. This study was approved by the Kosin Medical Center Institutional Review Board.
The authors measured serum CA15-3 at the preoperative period as well as at follow-up. CA15-3 level was compared between preoperative baseline and the level at the 6 months follow-up. This study measured the difference of the level between the two points and changes were reported in percentage (i.e., less than 10% or 10% or greater). Serum CA15-3 levels were determined using an automatic electrochemistry luminescence immunoassay system (ROCHE E170; Roche, Mannheim, Germany). The cutoff value of CA15-3 level was the increment (or decrement) of 25 U/mL, and the value of tumor marker was measured by computing the deviation from the cutoff. Tumor marker has positive value if serum level is above the cutoff and negative value when serum level is below the cutoff. The kinetics of serum CA15-3 levels were computed from the slope of an exponential regression curve that connects the semilogarithmic values of CA15-3 (Ln CA15-3 = log CA15-3/log e). Microsoft Excel software 2007 (Microsoft Inc., Redmond, WA, USA) was used to calculate the equation of the curve: y = a.exp (px; p = slope of the curve; x = number of months between follow-up periods; a = the corresponding CA15-3 value). For the surge group, two CA15-3 slopes were calculated per patient using the initial elevated serum CA15-3 level, the peak level, and the decreased level during each period. The mean score of the two slopes was then obtained.
Survival curves were estimated by Kaplan-Meier method. Statistical tests were performed using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). The survival function considered the time period from the onset of disease to the recurrence of disease. Survival data were censored out on December 31, 2014, which was the date when the survival data were correlated with the death registry for the last time or 5 years from the onset of the disease. Kaplan-Meier estimates are presented as the survival function. Log rank test was performed to test the significance of differences in survival rates. Associations between specific histopathological features and survival estimates and curves were established using the Kaplan-Meier method. The differences that were observed in survival functions among patient subgroups were tested by twosided log-rank test. All survival rates were presented with their standard errors. Pearson correlation was used to determine the association of pairs of explanatory variables. Differences in qualitative variables were evaluated by chi-square test, where necessary. All P-values were two-sided and a P-value of less than 0.05 was considered statistically significant.
Histopathological features such as hormone receptor status by immunohistochemical examination (Dako, Copenhagen, Denmark) were analyzed by the Institute of Pathology at the University of Kosin. Expressions of p53, estrogen receptor (ER), Ki-67, and human epidermal growth factor receptor 2 (HER2) were determined immunohistochemically on paraffin sections using antibodies against ER (Dako), Ki-67 (Dako), HER2 (Dako), and p53 (Dako). Histologic grading was performed using the criteria of Bloom and Richardson. Lymphatic vascular invasion was defined as the presence of tumor emboli in peritumoral lymphatic spaces, capillaries or postcapillary venules. ER status and PR status were taken as positive if more than 10% of tumor cells showed staining. HER2-positivity was indicated by a 2+ or 3+ score from the immunohistochemical examination, and the results were confirmed using a fluorescence in situ hybridization test for HER2. The cutoff point of 14% was used for Ki-67 staining. The molecular subtypes were classified into 4 groups; Luminal A (ER+ and/or PR+, HER2-, Ki-67<14%); Luminal B (ER+ and/or PR+, HER2+ and/or Ki-67 ≥14%); HER2 positive (ER- and PR-, HER2+); and triple-negative (ER- and PR-, HER2-). The classification follows the molecular subtype consensus of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011.
The median value of serial serum CA15-3 samplings of each patient was 8.
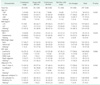
The patients' clinicopathologic characteristics are described in Table 1. There were no significant differences among the 5 groups in terms of age, breast cancer subtype, method of surgery, American Joint Committee on Cancer (AJCC) stage, body mass index, adjuvant chemotherapy method and radiation therapy. No significant differences were found among the five groups in terms of adjuvant chemotherapeutic agents, adjuvant endocrine treatments, and anti–HER2-directed trastuzumab therapy.
The main clinicopathologic characteristics of the patients in our series are summarized in Table 1. Mean age was 50 years. T1 stage was reported for 88 patients (57.0%). N0 stage was reported for 153 patients (47.0%). All patients underwent surgery: conservative surgery was carried out for 93 patients (31.3%) and mastectomy was performed on 188 patients (63.3%). Radiotherapy was delivered to 148 patients (49.8%). Adjuvant chemotherapy was administered to 252 patients (84.8%): 152 patients (51.2%) received combination chemotherapy with cyclophosphamide, methotrexate, and fluorouracil; 66 patients (22.2%) received anthracycline-based therapy; and 34 patients (11.4%) received taxane-based therapy. Endocrine therapy was administered to 241 patients out of 297 patients (81.1%). Tissue HER2 status was positive for 40 patients (13.5%) and negative for 180 patients (60.6%). And the kinetics of serum CA15-3 were not significantly associated with the AJCC stage pathologically (Table 1).
Among 297 breast cancer patients whose serum tumor markers were serially collected during the follow-up periods, the number of patients in group 1 (surge without incidental decline) was 30 patients (10.1%), and 85 patients (28.6%) for group 2 (surge with incidental decline). Group 3 (decline with incidental surge), group 4 (decline without incidental surge), and group 5 (no change) were assigned 80 patients (26.9%), 73 patients (24.6%), and 29 patients (9.8%), respectively. 5Y DFS of the groups were 73.3% (group 1), 91.8% (group 2), 89% (group 3), 90% (group 4), and 100% (group 5) (P = 0.004) (Fig. 1, Table 2). The pairwise comparison with log rank test indicates that the 5Y DFS of group 1 is significantly different from other groups (P = 0.001, P = 0.012, P = 0.031, and P = 0.001, respectively). But no significant differences were found in the other pairs in the comparison (Table 3).
The utility of measuring CA15-3 levels for breast cancer patients remains controversial. European Group on Tumor Markers has recommended the CEA and CA15-3 levels be used for assessing prognosis, the early detection of disease progression, and treatment monitoring in breast cancer. The American Society of Clinical Oncology and the National Comprehensive Cancer Network guidelines do not currently recommend the use of serum CA15-3 and CEA for breast cancer screening and directing treatment [122]. These controversies may be partly due to the conflicting conclusions of research [1923242526]. The low positive rate of serum tumor markers is also suspected as a possible reason. But several studies found that continuous CA15-3 elevation usually occurred in patients with disease progression [8]. The authors evaluated the clinical implications of the CA15-3 slope to breast cancer patients. This study found the CA15-3 surge phenomenon by examining the slopes of regressive exponential curves that were derived from serial CA15-3 levels. The surge group (group 1) had a significantly low 5Y DFS than other groups (73.3% vs. 89.6%, P < 0.05). The results suggest that the kinetics of CA15-3 levels can be used particularly for 'surge' cases to predict the prognosis, especially in terms of recurrence. CA15-3 slopes can also be easily calculated at the bedside by using serial results of CA15-3 level. Meanwhile, this study has several limitations. First, uniform consensus on the definition of the surge of tumor marker is not well established. Since the half-life of CA15-3 is unknown, it remains controversial how to define the optimal interval for tumor marker follow-up [18192728]. Second, the patients were clinicopathologically heterogeneous in terms of disease stage, and they were treated with different chemotherapeutic agents. These contribute to the difficulty in interpretation of the results to generate solid conclusions.
In spite of these limitations, however, the findings of this study support the authors' argument on the use of the 'surge' phenomenon of CA15-3 levels as an independent prognostic factor as well as a risk factor for breast cancer recurrence.
Figures and Tables
Table 2
Univariate analysis of prognostic factors for survival rate according to clinicopathological characteristics

5Y DFS, 5 year disease-free survival rate; BMI, body mass index; BCS, breast conserving surgery; ER, estrogen receptor; PR, progesterone receptor; IHC, immunohistochemistry; HER2, human epidermal growth factor receptor 2; TNBC, triple negative breast cancer; Non A, Non T, not containing adriamycin, not containing taxane; T without A, taxane without adriamycin; AI, aromatase inhibitor.
a)Missing data.
References
1. Shao Y, Sun X, He Y, Liu C, Liu H. Elevated levels of serum tumor markers CEA and CA15-3 are prognostic parameters for different molecular subtypes of breast cancer. PLoS One. 2015; 10:e0133830.
2. Wu SG, He ZY, Zhou J, Sun JY, Li FY, Lin Q, et al. Serum levels of CEA and CA15-3 in different molecular subtypes and prognostic value in Chinese breast cancer. Breast. 2014; 23:88–93.
3. Wang G, Qin Y, Zhang J, Zhao J, Liang Y, Zhang Z, et al. Nipple discharge of CA15-3, CA125, CEA and TSGF as a new biomarker panel for breast cancer. Int J Mol Sci. 2014; 15:9546–9565.
4. Zhang SJ, Hu Y, Qian HL, Jiao SC, Liu ZF, Tao HT, et al. Expression and significance of ER, PR, VEGF, CA15-3, CA125 and CEA in judging the prognosis of breast cancer. Asian Pac J Cancer Prev. 2013; 14:3937–3940.
5. Thriveni K, Deshmane V, Ramaswamy G, Krishnamoorthy L. Diagnostic significance of CA15-3 with combination of HER-2/neu values at 85th percentiles in breast cancer. Indian J Clin Biochem. 2013; 28:136–140.
6. Tarhan MO, Gonel A, Kucukzeybek Y, Erten C, Cuhadar S, Yigit SC, et al. Prognostic significance of circulating tumor cells and serum CA15-3 levels in metastatic breast cancer, single center experience, preliminary results. Asian Pac J Cancer Prev. 2013; 14:1725–1729.
7. Nisman B, Maimon O, Allweis T, Kadouri L, Maly B, Hamburger T, et al. The prognostic significance of LIAISON(R) CA15-3 assay in primary breast cancer. Anticancer Res. 2013; 33:293–299.
8. Kim HS, Park YH, Park MJ, Chang MH, Jun HJ, Kim KH, et al. Clinical significance of a serum CA15-3 surge and the usefulness of CA15-3 kinetics in monitoring chemotherapy response in patients with metastatic breast cancer. Breast Cancer Res Treat. 2009; 118:89–97.
9. Hiramoto Y, Tamada R, Sugimachi K, Nomura Y. The clinical value of a cancer antigen CA15-3 as a tumor associated antigen in breast carcinoma. Rinsho Byori. 1986; 34:1049–1052.
10. Tomlinson IP, Whyman A, Barrett JA, Kremer JK. Tumour marker CA15-3: possible uses in the routine management of breast cancer. Eur J Cancer. 1995; 31A:899–902.
11. Di Gioia D, Heinemann V, Nagel D, Untch M, Kahlert S, Bauerfeind I, et al. Kinetics of CEA and CA15-3 correlate with treatment response in patients undergoing chemotherapy for metastatic breast cancer (MBC). Tumour Biol. 2011; 32:777–785.
12. Lauro S, Trasatti L, Bordin F, Lanzetta G, Bria E, Gelibter A, et al. Comparison of CEA, MCA, CA 15-3 and CA 27-29 in follow-up and monitoring therapeutic response in breast cancer patients. Anticancer Res. 1999; 19(4C):3511–3515.
13. Kikuchi K, Uematsu Y, Takada Y, Kurihara E, Suito T, Fujisaki M, et al. Evaluation of tumor marker CA15-3 in breast cancer. Gan To Kagaku Ryoho. 1987; 14:3095–3100.
14. Lufter D, Richter A, Gunther S, Flath B, Akrivakis C, Geppert R, et al. A comparison of bone-related biomarkers and CA27.29 to assess response to treatment of osseous metastatic breast cancer. Anticancer Res. 2000; 20(6D):5099–5105.
15. Tondini C, Hayes DF, Gelman R, Henderson IC, Kufe DW. Comparison of CA15-3 and carcinoembryonic antigen in monitoring the clinical course of patients with metastatic breast cancer. Cancer Res. 1988; 48:4107–4112.
16. Loprinzi CL, Tormey DC, Rasmussen P, Falkson G, Davis TE, Falkson HC, et al. Prospective evaluation of carcinoembryonic antigen levels and alternating chemotherapeutic regimens in metastatic breast cancer. J Clin Oncol. 1986; 4:46–56.
17. Agha-Hosseini F, Mirzaii-Dizgah I, Rahimi A. Correlation of serum and salivary CA15-3 levels in patients with breast cancer. Med Oral Patol Oral Cir Bucal. 2009; 14:e521–e524.
18. Ali HQ, Mahdi NK, Al-Jowher MH. The value of CA15-3 in diagnosis, prognosis and treatment response in women with breast cancer. J Pak Med Assoc. 2013; 63:1138–1141.
19. Berruti A, Tampellini M, Torta M, Buniva T, Gorzegno G, Dogliotti L. Prognostic value in predicting overall survival of two mucinous markers: CA 15-3 and CA 125 in breast cancer patients at first relapse of disease. Eur J Cancer. 1994; 30A:2082–2084.
20. Kobayashi S, Iwase H, Karamatsu S, Matsuo K, Masaoka A, Miyagawa T. The clinical value of serum CA15-3 assay postoperatively in breast cancer patients. Jpn J Surg. 1989; 19:278–282.
21. Devine PL, Duroux MA, Quin RJ, McGuckin MA, Joy GJ, Ward BG, et al. CA15-3, CASA, MSA, and TPS as diagnostic serum markers in breast cancer. Breast Cancer Res Treat. 1995; 34:245–251.
22. Pons-Anicet DM, Krebs BP, Mira R, Namer M. Value of CA 15:3 in the follow-up of breast cancer patients. Br J Cancer. 1987; 55:567–569.
23. Bliss P, Fisken J, Roulsten J, Leonard RC. An assessment of the clinical usefulness of two serum markers, CA15 3 and HMFG 2 in localized and metastatic breast cancer. Dis Markers. 1993; 11:45–48.
24. Brooks M. Breast cancer screening and biomarkers. Methods Mol Biol. 2009; 472:307–321.
25. Daly L, Ferguson J, Cram GP Jr, Hars V, George SL, McCarty KS Jr, et al. Comparison of a novel assay for breast cancer mucin to CA15-3 and carcinoembryonic antigen. J Clin Oncol. 1992; 10:1057–1065.
26. Darwish IA, Wani TA, Khalil NY, Blake DA. Novel automated flow-based immunosensor for real-time measurement of the breast cancer biomarker CA15-3 in serum. Talanta. 2012; 97:499–504.
27. Hayes DF, Zurawski VR Jr, Kufe DW. Comparison of circulating CA15-3 and carcinoembryonic antigen levels in patients with breast cancer. J Clin Oncol. 1986; 4:1542–1550.
28. Keyhani M, Nasizadeh S, Dehghannejad A. Serum CA15-3 measurement in breast cancer patients before and after mastectomy. Arch Iranian Med. 2005; 8:263–266.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download