Abstract
Purpose
Laparoscopic cholecystectomy (LC) has become a standard treatment of symptomatic gallstone disease. But, some patients suffer from retained common bile duct stones after LC. The aim of this study is to analyze the predicting factors associated with subsequent postoperative endoscopic retrograde cholangiopancreatography (ERCP) after LC.
Methods
We retrospectively reviewed a database of every LC performed between July 2006 and September 2012. We classify 28 patients who underwent ERCP within 6 months after LC for symptomatic gallstone disease as the ERCP group and 56 patients who underwent LC for symptomatic gallstone disease during same period paired by sex, age, underlying disease, operation history, and body mass index as the control group. To identify risk factor performing postoperative ERCP after LC, we compared admission route, preoperative biochemical liver function test, number of gall stones, gallstone size, adhesion around GB, wall thickening of GB, and existence of acute cholecystitis between the 2 groups.
Results
Admission route, preoperative AST, ALT, and ALP, stone size, longer operation time, and acute cholecystitis were identified as risk factors of postoperative ERCP in univariate analyses. But, longer operation time (P = 0.004) and acute cholecystitis (P = 0.048) were identified as independent risk factors of postoperative ERCP in multivariate analyses.
Laparoscopic cholecystectomy (LC) has replaced open surgery as the gold standard treatment for symptomatic gallbladder (GB) disease since its clinical introduction approximately 25 years ago. It is the most common abdominal operation performed by general surgeons, with an estimated 750,000 cases in the United States each year [1].
Most cholecystectomies are performed due to the sequelae of GB stones, with the vast majority of patients experiencing complete symptom relief after cholecystectomy. However, approximately 5% of patients who have undergone cholecystectomy continue to have symptoms and are sometimes designated as suffering from postcholecystectomy syndrome (PCS) [23456]. The majority of patients who develop PCS actually suffer from nonbiliary disorders [4]. But, some patients have symptoms from etiologies such as biliary strictures, retained common bile duct (CBD) stones, and remnant cystic duct lithiasis.
A number of studies have reported outcomes of CBD stone retention rates after LC [789]. The reported incidence of asymptomatic CBD stones in those undergoing cholecystectomy is around 15% [1011], with complications occurring in 0.5%–2.3% of cases [1213], suggesting spontaneous passage or silent persistence of many CBD stones. Similarly, 20%–40% of patients who have bile duct filling defects at intraoperative cholangiography have either a negative surgical bile duct exploration or a negative postoperative endoscopic retrograde cholangiopancreatography (ERCP) [141516].
Because of the lack of a sensitive noninvasive imaging modality and also because the incidence and natural history of asymptomatic CBD stones has not been determined in patients selected for LC, patient selection for postcholecystectomy ERCP has been flawed. ERCP may be an unnecessary procedure in cases where there are no stones in the CBD and is associated with significant morbidity, such as acute pancreatitis, and even mortality.
To analyze the risk factors associated with subsequent postoperative ERCP after LC, we performed a retrospective case-control study of patients who underwent LC, comparing preoperative clinical parameters of patients who subsequently received ERCP with those who did not.
We retrospectively reviewed a database of 1,455 LCs performed between July 2006 and September 2012 in Kyung Hee University Hospital at Gangdong. We identified 28 patients who underwent ERCP within 6 months after LC for symptomatic GB stone disease as the ERCP group. Controls for each case were randomly selected (Excel, Microsoft Corp., Redmond, WA, USA) from the other patients who underwent LC for symptomatic GB disease during the same period paired by sex, age, underlying disease, operation history and body mass index (BMI). Diagnosis was made based on the association of several clinical and laboratory findings and was confirmed by abdominal ultrasonography or abdominopelvic computed tomography. GB removed incidentally as part of another procedure, GB cancers, and GB with no stones found at operation record or histology were excluded. Patients diagnosed preoperatively as CBD stones, cholangitis or gallstone pancreatitis were also excluded.
To evaluate whether there is a risk factor in patients who underwent ERCP within 6 months after LC, we compared admission route, preoperative biochemical liver function test, number of stones, gallstone size, adhesion around GB, wall thickening of GB, and existence of acute cholecystitis between the 2 groups. All biochemistry tests were done were within 1 week preoperatively. Gallstone size was defined as that of the largest stone measured. Information on the number of stones, adhesion around GB, and wall thickening of GB were collected from operation record. Acute or chronic cholecystitis was diagnosed according to the pathology reports.
Pearson chi-square test for categorical variables and linear-by-linear association method for continuous variables were employed in univariate analyses to evaluate the association of multiple clinical parameters between the ERCP group and control group. Multiple regression analysis was performed to examine for correlation between clinical parameters and postoperative ERCP. IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA) was employed for statistical analyses. A probability value below 0.05 was regarded as statistically significant.
Cholecystectomy was performed laparoscopically in all 84 patients of 2 groups. In the ERCP group, the patients underwent ERCP mostly due to postoperative abdominal pain and LFT elevation, except for 3 patients. Of these 3 patients, one underwent ERCP due to CBD stone incidentally found in the follow-up CT and 2 patients underwent ERCP due to detection of bile in the surgical drain. Only 10 patients (35.7%) were positive for CBD stones in the postoperative ERCP. Six cases showed some sludge without definite filling defect in cholangiogram and 2 cases showed cystic stump leak. Ten patients showed negative ERCP findings.
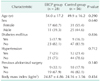
Twenty eight patients had a subsequent postoperative ERCP (ERCP group). Mean age of the patients was 54.0±17.2 years. There were more females (17 of 28, 60.7%) than males. Mean age of the 56 patients who did not had a postoperative ERCP (control group) was 49.9±16.2 years, with females predominating (31 of 56, 55.4%). There was no statistically significant difference of medical comorbidities, abdominal surgery history, and BMI between the 2 groups. The characteristics of patients of 2 groups are summarized in Table 1.
More patients were admitted to hospital through ER in the ERCP group than the control group (P = 0.030) (Table 2). Statistically significant differences were evident in preoperative AST, ALT, and ALP levels between the 2 groups. Preoperative levels of AST, ALT, and ALP were higher in the ERCP group than the control group. The level of total bilirubin was not statistically difference between the 2 groups.
The number of stones, stone size, adhesion around GB, GB wall thickening, length of operation, and inflammatory presentation were compared between the 2 groups (Table 3). Stone size was significantly smaller (P = 0.019) and operation time was significantly longer (P = 0.007) in the ERCP group than the control group. Acute cholecystitis was found more in the ERCP group than the control group (P = 0.001). There was no statistically difference of adhesion around GB, GB wall thickening, and number of stones between the 2 groups.
Univariate analysis identified admission route (P = 0.030), preoperative elevated AST, (P = 0.007), elevated ALT (P = 0.034), elevated ALP (P = 0.007), smaller stone size (P = 0.019), longer operation time (P = 0.007), and acute cholecystitis (P = 0.001) as risk factors of postoperative ERCP. However, multivariate analysis identified only longer OP time (P = 0.004) and acute cholecystitis (P = 0.048) as independent risk factors of postoperative ERCP (Table 4).
The incidence of retained CBD stones within 6 months following elective or emergency cholecystectomy for calculous cholecystitis was 0.68% (10 of 1,455). But we only took into account the patients that returned to our hospital with signs and symptoms suggestive of retained stones. The actual percentage could be higher. A prior study [17] reported a median time of 4 years for presentation of retained CBD stones after LC. The authors reported that the distribution was skewed with a quarter of patients presenting in the first 12 months, half by 4 years, with several patients presenting over 10 years post-LC [17].
As shown in Table 1, preoperative ALT seemed a sensitive marker for prediction of retained CBD stones after cholecystectomy. But, in the multivariate analysis, preoperative ALT was not statistically significant. ALT is generally not regarded as an important marker for hepatobiliary obstruction, although some studies highlighted the importance of ALT in making a diagnosis of retained CBD stones [1218]. One of these studies reported that 86% of patients with raised preoperative ALT levels were admitted as retained stones [12].
ALP and total bilirubin are generally regarded as important markers for biliary obstruction. Patients with elevated ALP, total bilirubin, serum amylase, and dilation of CBD before LC are strongly recommended to undergo preoperative ERCP [19]. Presently, elevated ALP was more prevalent in those patients who underwent ERCP in the univariate analysis. However, multivariate analysis revealed no statistically significant difference of ALP and total bilirubin level between the two groups. CBD stones apparent in the intraoperative cholangiography during LC were associated independently with increasing age and an elevated serum ALP, although neither were accurate indicators for treatment [20]. The spontaneous passage rate was similar for patients with elevated or normal ALP values. In a recently performed study of the usefulness of risk stratification in guiding appropriate biliary tract imaging, risk stratification including LFT helped to accurately predict CBD stones and facilitated appropriate and cost-effective use of ERCP [21].
The higher risk of pancreatitis with smaller gallstone size have been described [2223], but studies looking specifically at gallstone size in relation to the chance of postcholecystectomy retained CBD stones are rare. In one report, patients who had gallstones smaller than 7 mm were almost 10 times more likely to present with retained CBD stones than those who had larger stones present [24]. The narrow caliber and spiral valve of the cystic duct would make for more favorable transmission of smaller stones. But, gallstone size was not an independent factor of undergoing postoperative ERCP in our study. The difference between studies may involve the maximum size of the gallstones. If the size of the smallest gallstones were compared instead, the results may have been different. But, we recorded only the number and maximum size of gallstones. We plan to record the smallest size of gallstones henceforth.
We compared several operation findings between the 2 groups. The operation time was longer and the pathology report presented more acute cholecystitis in the ERCP group than the control group. LC for acute cholecystitis is generally more difficult than chronic cholecystitis or other symptomatic GB disease. The operation time is generally longer in the LC for acute cholecystitis too. As the operation time becomes more protracted, the probability of gallstone transmission to the CBD through the cystic duct will rise. The incidence of retained CBD stones is significantly higher in those requiring open cholecystectomy and is a reflection of their more complex disease [2526]. However, we are not aware of any study looking specifically at operation time or acute cholecystitis in relation to the prevalence of postcholecystectomy ERCP or retained CBD stones. A patient with longer operation time or history of acute cholecystitis should be most rigorously targeted for postoperative ERCP when the patient shows signs of cholangitis (fever, abdominal pain, or elevated LFT) after LC. However, only 35.7% of the patients who underwent postoperative ERCP were positive for CBD stones. This indicates that early postoperative ERCP should not be performed solely based on elevated LFT or other signs of cholangitis after LC. Every institution is in need of criteria predicting and determining the necessity of postoperative ERCP for the patients who receive LC.
There was no statistically significant difference of adhesion around GB and wall thickening of GB between the 2 groups.
In conclusion, this study demonstrated that longer operation time and acute cholecystitis could be possibly associated with prevalence of undergoing postoperative ERCP in patients with LC for symptomatic GB stone disease.
Figures and Tables
References
1. Russo MW, Wei JT, Thiny MT, Gangarosa LM, Brown A, Ringel Y, et al. Digestive and liver diseases statistics, 2004. Gastroenterology. 2004; 126:1448–1453.
2. Goenka MK, Kochhar R, Nagi B, Bhasin DK, Chowdhury A, Singh K. Endoscopic retrograde cholangiopancreatography in postcholecystectomy syndrome. J Assoc Physicians India. 1996; 44:119–122.
3. Mergener K, Clavien PA, Branch MS, Baillie J. A stone in a grossly dilated cystic duct stump: a rare cause of postcholecystectomy pain. Am J Gastroenterol. 1999; 94:229–231.
4. Rogy MA, Fugger R, Herbst F, Schulz F. Reoperation after cholecystectomy. The role of the cystic duct stump. HPB Surg. 1991; 4:129–134.
5. Stefanini P, Carboni M, Patrassi N, Loriga P, De Bernardinis G, Negro P. Factors influencing the long term results of cholecystectomy. Surg Gynecol Obstet. 1974; 139:734–738.
6. Zhou PH, Liu FL, Yao LQ, Qin XY. Endoscopic diagnosis and treatment of post-cholecystectomy syndrome. Hepatobiliary Pancreat Dis Int. 2003; 2:117–120.
7. Barkun JS, Fried GM, Barkun AN, Sigman HH, Hinchey EJ, Garzon J, et al. Cholecystectomy without operative cholangiography. Implications for common bile duct injury and retained common bile duct stones. Ann Surg. 1993; 218:371–377.
8. Braghetto I, Debandi A, Korn O, Bastias J. Long-term follow-up after laparoscopic cholecystectomy without routine intraoperative cholangiography. Surg Laparosc Endosc. 1998; 8:349–352.
9. Fogli L, Boschi S, Patrizi P, Berta RD, Al Sahlani U, Capizzi D, et al. Laparoscopic cholecystectomy without intraoperative cholangiography: audit of long-term results. J Laparoendosc Adv Surg Tech A. 2009; 19:191–193.
10. Franceschi D, Brandt C, Margolin D, Szopa B, Ponsky J, Priebe P, et al. The management of common bile duct stones in patients undergoing laparoscopic cholecystectomy. Am Surg. 1993; 59:525–532.
11. Petelin JB. Laparoscopic common bile duct exploration. Surg Endosc. 2003; 17:1705–1715.
12. Anwar S, Rahim R, Agwunobi A, Bancewicz J. The role of ERCP in management of retained bile duct stones after laparoscopic cholecystectomy. N Z Med J. 2004; 117:U1102.
13. Walsh RM, Ponsky JL, Dumot J. Retained gallbladder/cystic duct remnant calculi as a cause of postcholecystectomy pain. Surg Endosc. 2002; 16:981–984.
14. Bonatsos G, Leandros E, Polydorou A, Romanos A, Dourakis N, Birbas C, et al. ERCP in association with laparoscopic cholecystectomy. A strategy to minimize the number of unnecessary ERCPs. Surg Endosc. 1996; 10:37–40.
15. Ng T, Amaral JF. Timing of endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy in the treatment of choledocholithiasis. J Laparoendosc Adv Surg Tech A. 1999; 9:31–37.
16. Pencev D, Brady PG, Pinkas H, Boulay J. The role of ERCP in patients after laparoscopic cholecystectomy. Am J Gastroenterol. 1994; 89:1523–1527.
17. Cox MR, Budge JP, Eslick GD. Timing and nature of presentation of unsuspected retained common bile duct stones after laparoscopic cholecystectomy: a retrospective study. Surg Endosc. 2015; 29:2033–2038.
18. Patwardhan RV, Smith OJ, Farmelant MH. Serum transaminase levels and cholescintigraphic abnormalities in acute biliary tract obstruction. Arch Intern Med. 1987; 147:1249–1253.
19. Shiozawa S, Kim DH, Usui T, Tsuchiya A, Masuda T, Inose S, et al. Indication of endoscopic retrograde cholangiography by noninvasive predictive factors of common bile duct stones before laparoscopic cholecystectomy: a prospective clinical study. Surg Laparosc Endosc Percutan Tech. 2011; 21:28–32.
20. Collins C, Maguire D, Ireland A, Fitzgerald E, O'Sullivan GC. A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg. 2004; 239:28–33.
21. Shapey IM, Jaunoo SS, Arachchilage KM, Tan LC. Biliary tract imaging for retained calculi after laparoscopic cholecystectomy: is risk stratification useful? Surg Laparosc Endosc Percutan Tech. 2012; 22:459–462.
22. Diehl AK, Holleman DR Jr, Chapman JB, Schwesinger WH, Kurtin WE. Gallstone size and risk of pancreatitis. Arch Intern Med. 1997; 157:1674–1678.
23. Venneman NG, Buskens E, Besselink MG, Stads S, Go PM, Bosscha K, et al. Small gallstones are associated with increased risk of acute pancreatitis: potential benefits of prophylactic cholecystectomy? Am J Gastroenterol. 2005; 100:2540–2550.
24. Andrews S. Gallstone size related to incidence of post cholecystectomy retained common bile duct stones. Int J Surg. 2013; 11:319–321.
25. Ballal M, David G, Willmott S, Corless DJ, Deakin M, Slavin JP. Conversion after laparoscopic cholecystectomy in England. Surg Endosc. 2009; 23:2338–2344.
26. Peters JH, Krailadsiri W, Incarbone R, Bremner CG, Froes E, Ireland AP, et al. Reasons for conversion from laparoscopic to open cholecystectomy in an urban teaching hospital. Am J Surg. 1994; 168:555–558.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download