Abstract
Purpose
The aim of this study was to investigate the risk factors for conversion to conventional laparoscopic cholecystectomy (CLC) in single incision laparoscopic cholecystectomy (SILC) along with the proposal for procedure selection guidelines in treating patients with benign gallbladder (GB) diseases.
Methods
SILC was performed in 697 cases between April 2010 and July 2014. Seventeen cases (2.4%) underwent conversion to conventional LC. We compared these 2 groups and analyzed the risk factors for conversion to CLC.
Results
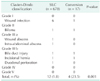
In univariate analysis, American Society of Anesthesiologist score > 3, preoperative percutaneous transhepatic GB drainage status and pathology (acute cholecystitis or GB empyema) were significant risk factors for conversion (P = 0.010, P = 0.019 and P < 0.001). In multivariate analysis, pathology (acute cholecystitis or GB empyema) was significant risk factors for conversion to CLC in SILC (P < 0.001).
Laparoscopic cholecystectomy has been recognized as the gold standard for treatment of benign gallbladder (GB) diseases [123]. Numerous previous studies have reported that laparoscopic cholecystectomy provides better cosmetic benefits, less postoperative pain, and short recovery time compared with open cholecystectomy. Corresponding with the development of minimal invasive laparoscopic surgery, Single incision laparoscopic cholecystectomy (SILC) is increasingly the preferred method in the treatment of benign GB diseases [4]. SILC was first introduced in 1997 by Navarra et al. [5]. Since then, numerous institutions have reported its safety and feasibility [6789] including many studies comparing SILC with conventional laparoscopic cholecystectomy (CLC) using multiport. Also, several studies have reported the advantages of SILC over CLC in terms of cosmetic benefit [121011]. However, there was a higher complications rate of SILC compared to CLC in another study [12]. Currently, SILC can be applied to many patients with benign gall bladder diseases. However, there is still controversy in SILC application. Despite advances in laparoscopic surgical techniques, several cases are required to convert to CLC in SILC. However, there are few data and studies on the risk of conversion or port addition in SILC. Several studies about SILC have suggested that careful attention required in patients with some risk factors including high body weight, poor physical status and/or acute cholecystitis. However, no definite indication criteria for SILC application have been established. Here we report our experiences of 697 cases treated by SILC with aim to investigate risk factors for conversion to CLC in SILC and to propose guidelines for choosing procedures to treat patients with benign GB diseases.
We retrospectively reviewed patients treated with SILC in our institution. This study included total of 697 patients initially diagnosed with benign GB diseases including acute cholecystitis, chronic cholecystitis, symptomatic GB stone, polyp, adenomyomatosis and empyema between April 2010 and July 2014. In this study, we excluded patients with suspected early-staged GB malignancy and with concurrent cardiopulmonary disorder who strongly expected perioperative morbidity. Between October 2010 and September 2012, we have performed SILC using the Konyang standard method based on the 3-channel method. Since then, we have performed SILC using the Modified Konyang standard method based on the 4-channel method. All operations were performed by two surgeons. We reported patient demography including Age (<80 years old or ≥80 years old), sex, body mass index (BMI, <30 or ≥30), previous abdominal operation history (upper abdominal surgery or lower abdominal surgery), preoperative percutaneous transhepatic GB drainage (PTGBD) status (yes or no), American Society of Anesthesiologist (ASA) score (<3 or ≥3), Pathological results and operative factors including operation time, estimated blood loss and hemovac insertion. In addition, postoperative complications were also included for analysis in our study. All the complications were recorded according to the Clavien-Dindo classification. Seventeen cases underwent conversion to CLC. We defined them as 'conversion group', others as 'SILC group', compared them to each other and analyzed risk factors for conversion to CLC.
We have reported the Konyang standard method in the Annals of Surgical Treatment and Research in 2014 [13]. The Konyang standard method is SILC using the 3-channel method and composed of traction, dissection, isolation, ligation and dissection from GB bed. We used a hand-made port constructed from a 10-mm-sized ALEXIS wound retractor (Applied Medical, Rancho Santa Margarita, CA, USA) and a size-7 sterile glove in which two 5-mm ports and one 10-mm port (Laport, Sejong Medical, Paju, Korea) and working channels for the laparoscopic instruments were prepared on the fingertip. We used a flexible telescope (Olympus, Tokyo, Japan), and a long articulated Endo-Roticulator (Covidien, Mansfield, MA, USA) for traction and dissection. The surgeons used right hand for traction and left hand for main procedures. In the modified Konyang standard method based on the 4-channel method, we applied one more additional port on the same single glove port [14]. Then, a 5-mm snake liver retractor (Diamond-Flex Triangular retractors, CareFusion, Waukegan, IL, USA) was introduced through this port to lift the liver more efficiently. Then, the modified Konyang standard method provided better exposure of the Calot's triangle so the operator could easily assess the Calot's triangle. Because of this advantage, we have more frequently performed SILC using modified Konyang standard method since 2012.
Variables are presented as mean ± standard deviation unless otherwise indicated. Categorical variables were analyzed using chi-square tests, continuous data by Student t-test. Univariate analysis and multivariate analysis was performed using logistic regression analysis to assess predictive risk factors for conversion to CLC. Statistical significance was considered as a P-value of less than 0.05. All statistical analyses were performed using IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA).
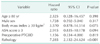
A total of 697 patients, all of whom were diagnosed with benign GB disease and treated with SILC, were included in our study. They consisted of 323 male (46.3%) and 374 female patients (53.7%) with a mean age of 52.4 ± 14.8 years. The mean BMI was 24.6 ± 3.6 kg/m2. Fifty-five patients (7.9%) were BMI over 30. Eighteen patients (2.6%) had previous upper abdomen operation history and 152 (21.8%) had lower abdomen operation history. ASA score was under 3 in 638 patients (91.5%) and 3 or over 3 in 59 patients (8.5%). Ninety-five patients (13.6%) were identified to have preoperative PTGBD. In perioperative factors, the mean operation time was 53.9 ± 20.1 minutes, the mean blood loss was 20.6 ± 42.1 mL and the mean hospital stay was 2.7 ± 2.4 days. In a total of 17 patients, drainages were inserted (Table 1).
The conversion rate was 2.4% (17 of 697 patients). The most common cause of conversion was inadequate exposure of the Calot's triangle due to severe adhesion and inflammation in 9 patients (52.9%); and one of them finally underwent open cholecystectomy. Seven patients (41.1%) were converted due to uncontrollable bleeding during the operation including bleeding of cystic artery and branches of small hepatic arteries or veins near the GB bed. The other causes of conversion included common bile duct injury during the operation.
Seventeen patients (2.4%) underwent conversion to CLC. Age was relatively higher in conversion group than SILC group (52.2 ± 14.7 years vs. 60.9 ± 16.9 years, P = 0.051). Also the proportion of patient aged over 80 years was relatively higher in conversion group (2.4% vs. 11.8%, P = 0.068). There were no significant differences in sex and BMI. Conversion group significantly had more prolonged operation time (52.7 ± 17.7 minutes vs. 101.2 ± 38.8 minutes, P < 0.001) and estimated blood loss (18.0 ± 20.0 mL vs. 125.3 ± 200.0 mL, P < 0.001) than SILC group. Postoperative hospital stay (2.7 ± 2.3 days vs. 4.3 ± 3.3 days, P = 0.047) was relatively higher in conversion group. In univariate analysis, pathological diagnosis in acute cholecystitis and GB empyema were significant risk factors for conversion (P < 0.001). Also, patients with ASA score 3 or over 3 were likely to require conversion (7.9% vs. 29.4%, P = 0.010) and preoperative PTGBD status was a significant risk factor for conversion (13.1% vs. 35.3%, P = 0.019) (Table 2).
In multivariate analysis, pathological diagnosis in acute cholecystitis or GB empyema were significant risk factors for conversion to CLC in SILC (hazard ratio, 7.285; P < 0.001) (Table 3).
Sixteen patients (2.2%) underwent postoperative complications. Complication rate was significantly higher in conversion group, Twelve complications occurred in SILC group and 4 complications occurred in conversion group (1.8% vs. 23.5%, P = 0.001). Six patients experienced grade I complication, mild wound complications that spontaneously resolved within a few days. Two patients developed grade II complications. Grade IIIa complications including wound abscess and intra-abdominal abscess occurred in 2 patients and they were treated with percutaneous drainage and antibiotics. Five patients developed grade IIIb complications which required surgical intervention. Two patients underwent bile duct injuries. One patient was treated with primary repair of common bile duct during the operation, and another detected at postoperative day 2 was determined as type E by Strasberg classification and was treated with hepaticojejunostomy. Two patients with incisional hernia were treated with laparoscopic hernioplasty with mesh. One patient who developed duodenal perforation was found in postoperative day 2 and treated with laparoscopic primary repair of duodenum (Table 4).
Many patients with benign GB disease are able to receive SILC. However, some of them also require to be converted to CLC with additional ports. There are limited data or studies to assess the risk factors for conversion to CLC in SILC and to find guidelines for SILC application. Although a larger multicenter trial is needed to confirm our results, our study is unique and significant in that it investigates the risk factors for conversion to CLC in SILC and we expect that these results will contribute to establish guidelines for SILC application.
In single institution experience with 80 cases reported in 2010 by Edwards et al. [6], nine patients out of 80 patients underwent conversion to multi-incision laparoscopic cholecystectomy and the most common cause of conversion was inadequate visualization of the Calot's triangle. Likewise, in a previous study, our leading causes of conversion were inadequate exposure of the Calot's triangle due to severe adhesion and inflammation and uncontrollable bleeding during the operation including bleeding of cystic artery and branches of small hepatic arteries or veins near the GB bed. Because there was more technical difficulty in patients with severe inflammation when we performed dissection of cystic artery, conversion due to bleeding mainly occurred as a result of inadequate exposure of the Calot's triangle. In the early days of SILC in our hospital, we used the 3-channel method named as 'Konyang standard method.' This method had limitations in visualization of the Calot's triangle. We excluded several patients with severe acute inflammation in this early period. To compensate for this limitation, we modified our 3-channel method with the addition of the snake liver retractor. Thus, visualization of the Calot's triangle has improved somewhat since then and application of SILC has been expanded; however, careful and exact dissection of vessels is still required when treating patients with acute inflammation. The application of SILC for acute inflammation of the GB is currently considered to be a contraindication because of the difficulty of the procedure [15]. Our results also revealed that patients diagnosed with acute cholecystitis or GB empyema are potentially more likely to be converted to CLC.
Ibrahim et al. [16] reported risk factors for conversion to open cholecystectomy in laparoscopic cholecystectomy to be male gender, advanced age (>60 years), higher body weight > 65 kg, acute cholecystitis, previous upper abdominal surgery, junior surgeon, and diabetes [17]. A previous study reported by Sato et al. [18] that investigated risk factors for a prolonged operative time in SILC, BMI and acute cholecystitis were significant risk factors for a prolonged operative time in SILC [19]. However, there are few data about risk factors for conversion in SILC to CLC. Our study focused on the risk factors for conversion to CLC in SILC. In univariate analysis, patients with ASA score 3 or over 3, perioperative PTGBD and acute inflammation were significant risk factors for conversion to CLC. And mulitivariate analysis revealed that pathological diagnosis in acute cholecystitis or GB empyema was only a significant risk factor for conversion. Although another study reported by Chuang et al. in 2013 [20] concluded that SILC is safe and feasible for patients with acute cholecystitis, our results suggest that careful treatment should be performed in acute cholecystitis or GB empyema. Maybe these risk factors will help surgeons plan and choose proper procedures when treating patients with benign GB disease.
Numerous previous studies have performed SILC with each technique. And their techniques had some differences from each other. Langwieler et al. [15] has reported Transumbilical single-port access cholecystectomy (SPACE) in 2009. This technique performed multichannel access that allows multiple instruments to pass through one incision at the same time using the TriPort Laparoscopic Access Device (Olympus). Because this technique had some problems such as crushing of the laparoscopic instruments and impeded movement of operator, Aprea et al. [2] have reported laparo-endoscopic single site (LESS) technique which modified previous SPACE cholecystectomy using a 0°-endoscopic camera with flexible head and transparietal suture for GB fundus retraction to make visualization and dissection of Calot's triangle easier and safer. Some other authors have reported several modified techniques for better exposure of Calot's triangle. In 2014, we reported SILC by Konyang standard method using a 3-trocar single port (hand-made) and long articulated instruments [13]. Because of limitation in exposure of Calot's triangle, we modified this technique and reported a 4-channel SILC called the modified Konyang standard method using a snake liver retractor for efficient retraction of the liver. This technique has several advantages such as better visibility and accessibility for dissection of the Calot's triangle. Since we modified the previous 3-channel SILC, many patients with acute cholecystitis could be treated with SILC. We expect that this technique could expand the range of applications of SILC.
There is limited information about postoperative complications in SILC and concern about the incidence of postoperative complications in SILC has risen with rapid development of surgical techniques. In our study, the most common postoperative complication was wound infection at umbilicus, which did not require surgical intervention in 9 patients. Complications requiring surgical interventions occurred in 4 patients (0.6%). Two patients with incisional hernia were successfully treated with laparoscopic hernioplasty with mesh. One patient who developed duodenal perforation was found in postoperative day 2 and treated with laparoscopic primary repair of duodenum. In 2012, Joseph et al. [12] reported higher risk of common bile duct injury in SILC. Only 2 patients (0.28%) sustained bile duct injuries in our study. One patient was treated with primary repair of common bile duct during the operation, and another detected at postoperative day 2 determined as type E by Strasberg classification was treated with hepaticojejunostomy. These 2 bile duct injuries occurred in the early stages of SILC in Konyang University Hospital. Since we applied the modified Konyang standard method, incidence of bile duct injury and other complications has tended to decrease gradually.
Recently, with the advance and widespread application of laparoscopic cholecystectomy, the incidence of incidental GB cancer has increased [16]. Three patients of all treated with SILC were diagnosed with incidental GB cancer. There were no GB perforations or bile spillage during the operations. One of them revealed T1a so we maintained close observation without further surgical intervention. And there is no recurrence or distant metastasis. Others revealed T2. However, one of them transferred to another clinic and the other refused reoperation for radical resection because of age and poor physical status. Several studies have reported the application of laparoscopic cholecystectomy in GB tumor suspicious of malignancy [21]. Although CLC could be appropriate for early GB cancer, there is still high risk of bile spillage in laparoscopic cholecystectomy. And bile spillage is likely to be associate with an incomplete resection and systemic recurrence [17]. Therefore, when patients are suspected of GB cancer preoperatively, SILC should be avoided and further evaluation for incidental GB cancer in SILC should be required.
In summary, the conversion rate in SILC was 2.4%. Main causes of conversion were inadequate exposure of the Calot's triangle and bleeding. And the complication rate was significantly higher in conversion group. Pathological diagnosis in acute cholecystitis or GB empyema, ASA score 3 or over 3, and preoperative PTGBD were significant risk factors for conversion in univariate analysis. In multivariate analysis, the risk factors for conversion were pathological diagnoses in acute cholecystitis or GB empyema.
In conclusion, for most patients with benign GB disease, SILC is a safe and feasible method. However, if patients are diagnosed with acute cholecystitis or GB empyema, it is likely to result in inadequate visualization of the Calot's triangle and more bleeding risk in SILC. Therefore, CLC should be considered in these cases.
Figures and Tables
References
1. Lirici MM, Califano AD, Angelini P, Corcione F. Laparo-endoscopic single site cholecystectomy versus standard laparoscopic cholecystectomy: results of a pilot randomized trial. Am J Surg. 2011; 202:45–52.
2. Aprea G, Coppola Bottazzi E, Guida F, Masone S, Persico G. Laparoendoscopic single site (LESS) versus classic video-laparoscopic cholecystectomy: a randomized prospective study. J Surg Res. 2011; 166:e109–e112.
3. Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. 2006; (4):CD006231.
4. Chamberlain RS, Sakpal SV. A comprehensive review of single-incision laparoscopic surgery (SILS) and natural orifice transluminal endoscopic surgery (NOTES) techniques for cholecystectomy. J Gastrointest Surg. 2009; 13:1733–1740.
5. Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997; 84:695.
6. Edwards C, Bradshaw A, Ahearne P, Dematos P, Humble T, Johnson R, et al. Single-incision laparoscopic cholecystectomy is feasible: initial experience with 80 cases. Surg Endosc. 2010; 24:2241–2247.
7. Erbella J Jr, Bunch GM. Single-incision laparoscopic cholecystectomy: the first 100 outpatients. Surg Endosc. 2010; 24:1958–1961.
8. Rivas H, Varela E, Scott D. Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc. 2010; 24:1403–1412.
9. Hirano Y, Watanabe T, Uchida T, Yoshida S, Tawaraya K, Kato H, et al. Single-incision laparoscopic cholecystectomy: single institution experience and literature review. World J Gastroenterol. 2010; 16:270–274.
10. Lai EC, Yang GP, Tang CN, Yih PC, Chan OC, Li MK. Prospective randomized comparative study of single incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy. Am J Surg. 2011; 202:254–258.
11. van den Boezem PB, Velthuis S, Lourens HJ, Cuesta MA, Sietses C. Single-incision and NOTES cholecystectomy, are there clinical or cosmetic advantages when compared to conventional laparoscopic cholecystectomy? A case-control study comparing single-incision, transvaginal, and conventional laparoscopic technique for cholecystectomy. World J Surg. 2014; 38:25–32.
12. Joseph M, Phillips MR, Farrell TM, Rupp CC. Single incision laparoscopic cholecystectomy is associated with a higher bile duct injury rate: a review and a word of caution. Ann Surg. 2012; 256:1–6.
13. Son JI, Choi IS, Moon JI, Ra YM, Lee SE, Choi WJ, et al. Single incision laparoscopic cholecystectomy using Konyang Standard Method. Ann Surg Treat Res. 2014; 86:177–183.
14. Sung NS, Choi IS, Moon JI, Ra YM, Lee SE, Choi WJ. Four-channel single incision laparoscopic cholecystectomy using a snake retractor: comparison between 3- and 4-channel SILC 4-channel single incision cholecystectomy. Ann Surg Treat Res. 2014; 87:81–86.
15. Langwieler TE, Nimmesgern T, Back M. Single-port access in laparoscopic cholecystectomy. Surg Endosc. 2009; 23:1138–1141.
16. Ibrahim S, Hean TK, Ho LS, Ravintharan T, Chye TN, Chee CH. Risk factors for conversion to open surgery in patients undergoing laparoscopic cholecystectomy. World J Surg. 2006; 30:1698–1704.
17. Lee JM, Kim BW, Kim WH, Wang HJ, Kim MW. Clinical implication of bile spillage in patients undergoing laparoscopic cholecystectomy for gallbladder cancer. Am Surg. 2011; 77:697–701.
18. Sato N, Yabuki K, Shibao K, Mori Y, Tamura T, Higure A, et al. Risk factors for a prolonged operative time in a single-incision laparoscopic cholecystectomy. HPB (Oxford). 2014; 16:177–182.
19. Tian YH, Ji X, Liu B, Yang GY, Meng XF, Xia HT, et al. Surgical treatment of incidental gallbladder cancer discovered during or following laparoscopic cholecystectomy. World J Surg. 2015; 39:746–752.
20. Chuang SH, Chen PH, Chang CM, Lin CS. Single-incision vs three-incision laparoscopic cholecystectomy for complicated and uncomplicated acute cholecystitis. World J Gastroenterol. 2013; 19:7743–7750.
21. Fujisaki S, Saitoh Y, Tomita R, Fukuzawa M. Laparoscopic extended cholecystectomy. J Laparoendosc Adv Surg Tech A. 2001; 11:219–222.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download