Abstract
Purpose
The aim of this study was to find risk factors for early recurrence (ER) and early death (ED) after liver resection for colorectal cancer liver metastasis (CRCLM).
Methods
Between May 1990 and December 2011, 279 patients underwent liver resection for CRCLM at Korea University Medical Center. They were assigned to group ER (recurrence within 6 months after liver resection) or group NER (non-ER; no recurrence within 6 months after liver resection) and group ED (death within 6 months after liver resection) or group NED (alive > 6 months after liver resection).
Results
The ER group included 30 patients (10.8%) and the NER group included 247 patients (89.2%). The ED group included 18 patients (6.6%) and the NED group included 253 patients (93.4%). Prognostic factors for ER in a univariate analysis were poorly differentiated colorectal cancer (CRC), synchronous metastasis, ≥5 cm of liver mass, ≥50 ng/mL preoperative carcinoembryonic antigen level, positive liver resection margin, and surgery alone without perioperative chemotherapy. Prognostic factors for ED in a univariate analysis were poorly differentiated CRC, positive liver resection margin, and surgery alone without perioperative chemotherapy. Multivariate analysis showed that poorly differentiated CRC, ≥5-cm metastatic tumor size, positive liver resection margin, and surgery alone without perioperative chemotherapy were independent risk factors related to ER. For ED, poorly differentiated CRC, positive liver resection margin, and surgery alone without perioperative chemotherapy were risk factors in multivariate analysis.
Many authors have reported that survival can be prolonged by adequate chemotherapy and molecular target drugs for unresectable or recurrent colorectal cancer liver metastasis (CRCLM). But, surgical resection is still the lone potentially therapeutic treatment for CRCLM. Complete surgical resection combined with chemotherapy can raise 5-year survival rates up to 60% [1]. Despite these excellent results, about 60% of patients who underwent first liver resection for CRCLM will experience recurrence during follow-up [2]. Recurrence is the main cause of death after liver resection for CRCLM [3]. Survival rates are getting worse in patients with repeat liver resection for recurrent hepatic metastasis after previous liver resection. The 3-year overall survival rate of these patients with repeat liver resection is about 30%.
In a previous study, Takahashi et al. [4] showed that time to recurrence after liver resection for CRCLM correlated with prognosis. In their study, patients with recurrence within 6 months after liver resection have the poorest outcome. The aim of this study was to retrospectively investigate risk factors related to recurrence and death within 6 months after liver resection for CRCLM.
A total of 279 patients underwent liver resection for CRCLM between May 1990 and December 2011 at Korea University Medical Center was included in this retrospective study. Two patients revealed positive resection margin after CRC and they were excluded from this study. So, 277 patients were included in this study and they were followed for a minimum 1 year or until death. They were categorized into group ER (early recurrence; recurrence within 6 months after liver resection) or group NER (non-ER; no recurrence within 6 months after liver resection) and group ED (early death; death within 6 months after liver resection) or group NED (non-ED; alive > 6 months after liver resection). The ER group included 30 patients (10.8%), and the NER group included 247 patients (89.2%). The ED group included 18 patients (6.6%), and the NED group included 253 patients (93.4%). Of all 277 patients, 6 patients (2.2%) who died due to postoperative complications (3 patients, 1.1%), ischemic heart disease (2 patients, 0.8%), and unknown cause (1 patient, 0.4%) within 6 months after liver resection were excluded from groups ED and NED.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The characteristics of the primary colorectal cancer (CRC) were evaluated for predictive factors, including tumor location (colon or rectum), tumor T stage (T1–2 or T3–4), nodal status (N0-N2b), and tumor differentiation (well to moderately or poorly differentiated adenocarcinoma).
Liver resection was indicated for CRCLM when the primary CRC was completely resected and metastasis occurred only in the liver. CRCLM are considered unresectable when the following criteria are met:
(1) Resection of the liver metastasis would not allow for the preservation of sufficient volume of liver to avoid postoperative liver failure.
(2) Treatment of primary colorectal lesion would not be curable resection.
(3) There were uncontrolled extrahepatic metastases.
All patients received therapeutic liver resection with a safety margin but hepatic hilar lymph node dissection was not performed routinely. Synchronous CRCLM was characterized as concurrent appearance of liver metastasis at the time of CRC diagnosis or operation. All patients underwent simultaneous or staged liver resection. Anatomical resection was characterized as complete anatomical resection based on Couinaud's classification (segmentectomy, sectionectomy, and hemihepatectomy or extended hemihepatectomy) in patients with an acceptable liver reserve. Nonanatomical resection was defined as limited resection or tumor enucleation.
The choice of neoadjuvant chemotherapy or adjuvant chemotherapy alone was determined based on the CRC histological result. Patients needed an Eastern Cooperative Oncology Group status of 0-2 to receive chemotherapy. Regimens were composed of 5-fluorouracil (5-FU) alone, 5-FU/leucovorin (LV), 5-FU/cisplatin, FOLFOX (infusional 5-FU/LV + oxaliplatin) and FOLFIRI (infusional 5-FU/LV + irinotecan).
Patient data were examined by liver function tests, tumor marker measurements, and computed tomography or ultrasonography every 3-6 months for the first year after liver resection. If recurrence was suspected, magnetic resonance imaging or bone scintigraphy was performed.
We analyzed patient demographics, tumor markers, tumor characteristics, treatment, recurrence, and survival data to identify risk factors for ED or recurrence within 6 months after liver resection for CRCLM. Preoperative CEA levels were classified into 2 categories of ≥50 and <50 ng/mL. We assessed different tumor characteristics, such as size of the largest tumor, number of tumors, tumor distribution, histology and extent of the tumor. The largest tumor was classified into 2 categories of ≥5 and <5 cm.
We performed analyses with standard tests (chi-square and t-test) where appropriate. We also performed a univariate analysis with the log-rank test. A multivariate analysis and logistic regression were performed for parameters with a univariate analysis result of P < 0.5. P < 0.05 was considered significant.
The mean age of the 277 patients was 65.5 years (range, 33-89 years). Of the 277 patients, 189 patients (68.2%) were male and 88 patients (31.8%) were female, 69 patients (24.9%) were HBV surface antigen positive, 5 patients (1.8%) were HCV antibody positive, and 8 patients (2.9%) had liver cirrhosis. Two hundred sixty-nine patients (97.1%) were categorized as Child-Pugh class A. The patients were followed up for a median of 45.1 months (range, 13.1-214.0 months). Univariate and multivariate analysis revealed that sex, age at liver resection, presence of HBV or HCV, liver cirrhosis, and Child-Pugh class were not associated with ER or ED (Tables 1, 2).
The primary CRC was in the colon in 163 patients (58.8%) and in the rectum in 114 patients (41.2%). But, Primary CRC tumor location was not connected to ER or ED. One hundred seventy-three patients (62.5%) had advanced T stage (T3–4) and 185 patients (66.8%) patients had regional lymph node metastasis. However, advanced T stage and node-positive primary tumor were also not connected to ER or ED.
Ninety-eight patients (35.4%) had poorly differentiated histology. The risk of ER and ED increased among patients with poorly differentiated primary CRC (ER 66.7% vs. NER 31.6%, P = 0.007; ED 83.3% vs. NED 31.6%, P = 0.008). At multivariate analysis, poorly differentiated primary CRC was an independent risk factor with ER (odds ratio [OR], 4.52; P = 0.005) and ED (OR, 3.21; P = 0.003).
Synchronous CRCLM was detected in 175 patients (63.2%) and metachronous CRCLM was detected in 102 patients (36.8%). In univariate analysis, the risk of ER was increased among patients with synchronous metastasis (ER 93.3% vs. NER 59.5%, P = 0.04). However, in multivariate analysis, synchronous metastasis was not independent risk factor for ER.
Among the 175 patients with synchronous CRCLM, simultaneous liver resection was done in 91 patients (52%) and staged liver resection was done in 84 patients (48%). Time of liver resection was not associated with ER or ED.
The mean and median sizes of the largest liver tumor were 4.12 ± 1.21 cm and 4.2 cm. Of the 277 patients, 186 patients (67.1%) underwent liver resection for solitary metastasis, 85 patients (30.7%) for 2 or 3 tumors, and 6 patients (2.2%) had four or more tumors resected. The tumor was located in single lobar in 187 patients (67.5%), in multi lobar in 90 patients (32.5%).
The number and distribution of CRCLM were not associated with ER or ED. But, the risk of ER increased among patients with the largest tumors (≥5 cm), which was identified as a risk factor for ER (ER 43.3% vs. NER 11.7%, P = 0.04; OR, 2.82, P = 0.003).
Forty-one patients (14.8%) had preoperative elevated serum CEA levels (≥50 ng/mL). The ER rate increased by elevated serum CEA levels (ER 53.3% vs. NER 10.1%, P = 0.04); however, it was not risk factor for ER in multivariate analysis (OR, 1.21; P = 0.48).
Anatomic liver resection was done in 97 patients (35%) and over 3 segment liver resections were done in 50 patients (18%). Thirteen patients (5%) underwent laparoscopic liver resection. The type (anatomic vs. nonanatomic), extent (<3 segments vs. ≥3 segments), and resection method (laparoscopic vs. open) were not associated with ER and ED.
Twenty-two patients (7.9%) had positive resection margin after liver resection. Positive liver resection margins were revealed as a significant risk factor for both ER (ER 63.3% vs. NER 1.2%, P = 0.006; OR, 3.25, P = 0.001) and both ED (ED 83.3% vs. NED 2.8%, P = 0.004; OR, 4.45; P = 0.003) in univariate and multivariate analysis.
A total of 229 patients (82.7%) received perioperative chemotherapy (5-FU alone, 31 patients [14%]; 5-FU/LV, 98 patients [43%]; 5-FU/cisplatin, 22 patients [10%]; FOLFOX, 53 patients [23%]; FOLFIRI, 25 patients [11%]), and 48 patients (17.3%) underwent liver resection without perioperative chemotherapy. It was impossible to determine why these 48 patients did not receive chemotherapy because this is a retrospective study. Among the 229 patients who underwent perioperative chemotherapy, 57 patients (24.9%) received chemotherapy before and after liver resection and 172 patients (75.1%) received chemotherapy only after liver resection. The risk of ER and ED increased among patients with surgery without perioperative chemotherapy (ER 60.0% vs. NER 12.1%, P = 0.04; ED 44.4% vs. NED 13.4%, P = 0.03), and it was a significant risk factor for ER (OR, 3.53; P = 0.004) and ED (OR, 2.35; P = 0.002) in multivariate analysis.
The liver is a common site of metastasis from gastrointestinal tumors, probably because of dissemination via the portal venous system. Liver resection is the gold-standard treatment for CRCLM. Many studies have demonstrated that long-term survival can be achieved after surgical resection of CRCLM [5]. But, surgical treatments can only be performed in 10% of patients with metastasis from CRC and 50%–75% of these patients progress to disease recurrence after therapeutic resection of CRCLM; and recurrence is the leading cause of death even after curative liver resection [3]. Unfortunately, most recurrence occurs within first 2 years [2].
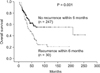
In most previous study, delay of recurrence is a well-known prognostic factor and lower survival was observed in patients with ER than in patients with late recurrence. ER after liver resection is one of the most critical factors for prognosis and quality of life in patients with CRCLM, and recurrence is the main cause of death after liver resection for CRCLM. In the present study, 5-year overall survival rate was 57.6% in patients without recurrence within 6 months after hepatectomy for CRCLM and 33.8% in patients with recurrence within 6 months (P = 0.001) (Fig. 1). ER (within 6 months after liver resection for CRCLM) rates were reported at about 10.6% in a previous large-scale study [6] and our study showed similar ER rates (10.8%).
ER is more common in patients with aggressive disease, such as those with synchronous and multiple metastases, or advanced T and N Staging [7]. Scheele and Stang [8] reported that location of CRC (rectum), high-grade histology of CRC, lymph node metastasis of CRC, and synchronous liver metastasis were poor prognostic factors for patient survival and disease-free survival. In our study, location of primary CRC, lymph node metastasis of CRC, and synchronous liver metastases were not related with ER and ED. But, poorly differentiated CRC was a risk factor for ER and ED in univariate and multivariate analysis.
ERs were also related to some technical issues. Complete surgery with R0 resection is considered mandatory; however, debate about the adequate width of the surgical margin is ongoing [7]. A recent study by Pawlik et al. [9] showed that positive margin after resection of CRCLM is associated with adverse biological factors and increased risk of surgical-margin recurrence. They also reported that the width of a negative surgical margin dose not affect survival, recurrence risk, or site of recurrence. In our study, positive liver resection margin was an independent risk factor related to ER and ED in multivariate analysis. Unfortunately, we could not confirm width of resection margins in our study because of lack of medical records.
Fong et al. [6] reported that the number of liver metastases and the size of the metastasis were associated with a poor prognosis. In contrast, the hepatic distribution (single lobar vs. multi lobar) was not a prognostic parameter related to poor prognosis. In this study, number of hepatic tumors >1 and largest hepatic tumor >5 cm were selected as an independent risk factor for poor long-term outcome by multivariate analysis. In our study, ≥5-cm metastatic tumor size was also related with ER, but not related with ED in multivariate analysis. Moreover, number of liver metastases and hepatic distribution (single lobar vs. multi lobar) was not related with ER or ED.
Controversy exists as to whether or not to perform simultaneous liver resection for CRCLM. Many patients receive staged liver resection, because of postoperative morbidity and prolonged, tiring treatment. Turrini et al. [10] reported that they did not observe any statistical difference on survival between simultaneous and staged liver resection, but they supported simultaneous liver resection. In our study, no difference in the prognosis was observed between simultaneous and staged liver resection.
Many authors have reported on the relationship of preoperative CEA levels and prognosis. Koga et al. [11] reported that CEA is an independent prognostic factor for recurrence and survival in patients who had undergone liver resection for CRCLM. Fong et al. [6] showed that high serum CEA levels (>200 ng/mL) are associated with more aggressive tumor behavior and a poor prognosis. In our study, preoperative elevated serum CEA levels (≥50 ng/mL) were risk factors for ER in univariate analysis, but not in multivariate analysis. Also, it was not related with ED in univariate and multivariate analysis.
Nordlinger et al. [12] showed that perioperative chemotherapy with FOLFOX4 is compatible with major liver resection and reduces the risk of events of progression free survival in eligible and resected patients in their study. In our study, the combination of surgical therapy and perioperative chemotherapy was effective for ER and a good prognosis. However, a subgroup analysis (divided by chemotherapy regimen; 5-FU, 5-FU/LV, 5-FU/cisplatin, FOLFOX, and FOLFIRI) revealed no difference in ER or ED. We should consider that the chemotherapy regimen in this study consisted of 5-FU, 5-FU/LV, 5-FU/cisplatin, FOLFOX, and FOLFIRI. However, many recent studies have shown that molecular targeting agents, such as bevacizumab and cetuximab, could be effective for recurrent or unresectable CRC [1314]. They were not included in this study. It is difficult to evaluate the impact of perioperative chemotherapy. But, we could assume a protective effect of perioperative chemotherapy, and that it might be related to a delay in recurrence.
In conclusion, complete liver resection with clear resection margin and perioperative chemotherapy should be carefully considered when patients have the following preoperative risk factors: metastatic tumor size ≥ 5 cm and poorly differentiated CRC.
Figures and Tables
References
1. Adam R, De Gramont A, Figueras J, Guthrie A, Kokudo N, Kunstlinger F, et al. The oncosurgery approach to managing liver metastases from colorectal cancer: a multidisciplinary international consensus. Oncologist. 2012; 17:1225–1239.
2. de Jong MC, Pulitano C, Ribero D, Strub J, Mentha G, Schulick RD, et al. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg. 2009; 250:440–448.
3. Fortner JG. Recurrence of colorectal cancer after hepatic resection. Am J Surg. 1988; 155:378–382.
4. Takahashi S, Konishi M, Nakagohri T, Gotohda N, Saito N, Kinoshita T. Short time to recurrence after hepatic resection correlates with poor prognosis in colorectal hepatic metastasis. Jpn J Clin Oncol. 2006; 36:368–375.
5. Choti MA, Sitzmann JV, Tiburi MF, Sumetchotimetha W, Rangsin R, Schulick RD, et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg. 2002; 235:759–766.
6. Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999; 230:309–318.
7. Vigano L, Capussotti L, Lapointe R, Barroso E, Hubert C, Giuliante F, et al. Early recurrence after liver resection for colorectal metastases: risk factors, prognosis, and treatment. A LiverMetSurvey-based study of 6,025 patients. Ann Surg Oncol. 2014; 21:1276–1286.
8. Scheele J, Stang R, Altendorf-Hofmann A, Paul M. Resection of colorectal liver metastases. World J Surg. 1995; 19:59–71.
9. Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005; 241:715–722.
10. Turrini O, Viret F, Guiramand J, Lelong B, Bege T, Delpero JR. Strategies for the treatment of synchronous liver metastasis. Eur J Surg Oncol. 2007; 33:735–740.
11. Koga H, Moriya Y, Akasu T, Fujita S. The relationship between prognosis and CEAdt after hepatic resection in patients with colorectal carcinomas. Eur J Surg Oncol. 1999; 25:292–296.
12. Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet. 2008; 371:1007–1016.
13. Meyerhardt JA, Mayer RJ. Systemic therapy for colorectal cancer. N Engl J Med. 2005; 352:476–487.
14. Leonard GD, Brenner B, Kemeny NE. Neoadjuvant chemotherapy before liver resection for patients with unresectable liver metastases from colorectal carcinoma. J Clin Oncol. 2005; 23:2038–2048.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download