Abstract
Purpose
Postoperative pain for robotic thyroid surgeries including bilateral axillo-breast approach (BABA) has not been well studied. In this study, we have developed a self-reporting application (SRA) for iPad and prospectively collected pain scores from open thyroidectomy (OT) and BABA robotic thyroidectomy (RT) patients.
Methods
Female patients who underwent total thyroidectomy for papillary thyroid carcinoma were included. Patients recorded pain scores for throat, anterior neck, posterior neck, chest, and back on postoperative days 1, 2, and 3. Once discharged, on postoperative day 14, a survey was also conducted on satisfaction of SRA and cosmesis.
Results
A total of 54 patients were enrolled (27 BABA RT and 27 OT). There were no significant differences between the 2 groups in clinicopathological characteristics and postoperative complication rates. Postoperative pain scores at days 1, 2, 3, and 14 were not significantly different between the groups for throat, anterior neck, posterior neck, or back. Postoperative analgesic requirements were similar between the 2 groups. Wound satisfaction scores were significantly higher in the BABA RT group (BABA RT 7.4 vs. OT 5.7; P = 0.016). Satisfaction scores for the usefulness of SRA were above 7.2 for all four questionnaire items on the 10-point scale.
Thyroid carcinoma is the most common endocrine malignancy necessitating thyroid surgeries with an excellent overall survival outcome. In general, open thyroid surgeries are well tolerated, but may result in conspicuous neck scars. To minimize such undesirable outcomes, remotely accessed endoscopic thyroid surgeries utilizing the da Vinci robot surgical system have been adopted. Thus far, surgical safety and oncologic outcomes are reported to be comparable to traditional open surgery [1].
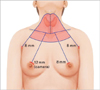
Among the various robotic thyroidectomy (RT) approaches, unilateral transaxillary approach is one of the most widely used methods [2]. Despite several advantages of this approach, complete removal of the contralateral thyroid gland is difficult due to limited view and challenging dissection of the contralateral recurrent laryngeal nerve [3]. On the other hand, bilateral axillo-breast approach (BABA) RT uses 4 small incisions via bilateral axillae and areolae. The right areolar skin incision is used as a camera port to offer a near symmetrical midline view (Fig. 1), which is familiar to surgeons [45]. This enables surgeons to perform bilateral thyroid lobectomy safely and completely in direct vision of bilateral recurrent laryngeal nerves [678]. However, there are some concerns that BABA RT might cause greater pain compared to conventional open thyroidectomy (OT) because BABA RT requires subcutaneous tissue tunneling from the four skin incision sites and wide flap dissection around neck.
In order to assess the postoperative pain for BABA RT and compare it to that of conventional OT, we have developed an iPad (Apple, Cupertino, CA, USA) application named self-reporting application (SRA). Using this application, postoperative pain scores were entered by the patients at bedside, which were then uploaded to the database using wireless networks. Pain scores were compartmentalized and recorded separately for throat, anterior neck, left and right chest, posterior neck, and back.
The Institutional Review Board at Seoul National University Hospital approved this study (IRB No. H-1212-074-451). Female patients undergoing total thyroidectomy with ipsilateral central lymph node dissection for preoperative diagnosis consistent with papillary thyroid cancer were enrolled in this prospective study. Only female patients were enrolled given the predominant preference for RT. Patients were allocated into RT or OT group based on their preference during the clinic visit. Age range for both RT and OT groups were 21 to 60 and all participants were capable of using iPad. Exclusion criteria included the patients who underwent lateral neck lymph node dissection or who had difficulties using iPad even after instruction. Once the patient consented to the study, medical staff (J.K, Y.J.C) provided iPads and explained how to input the pain scale data using the SRA program prior to the surgery. Several educational video clips regarding thyroid cancer, thyroid surgery, BABA RT procedure, and postoperative care were also provided via the iPads.
Along with the routine preoperative work-up for OT patients, BABA RT patients had additional breast imaging work-ups, preoperatively. Breast ultrasound and mammography were performed routinely within 3 months of surgery, and proper management including further imaging work-up or breast biopsy were selected according to the results. When the patients had mastalgia or inflammation on the breast, the operation was delayed and the patients were referred to breast surgeons.
OT was performed using a standard transverse low cervical incision along the natural skin crease (average, 5 to 6 cm). Once the subplatysmal flaps were created the midline fascia was divided to expose the thyroid gland. Then, the thyroid isthmus was routinely transected. After detaching strap muscles from the lateral side of the thyroid glands, superior and inferior thyroidal arteries were ligated and divided after recurrent laryngeal nerve identification. Superior and inferior parathyroid glands were preserved when possible. Midline fascia and platysma were approximated and then skin was closed using an absorbable suture.
BABA RT techniques are described in detail previously [4]. In brief, patients were placed in a supine position with slight neck extension. After drawing an outline for the flap dissection, about 200 mL of diluted epinephrine (1:200,000) were injected along the upper chest and the subplatysmal space. Then, two superomedial circumareolar marginal incisions (right, 1.2cm; left, 0.8 cm) and two axillary skin incisions (0.8 cm each) were made for the port sites. Flap dissections were initially carried out using endoscopic instruments and CO2 insufflation was followed by the docking of robotic instruments. Once the working space was established, the rest of the surgical approaches were essentially the same compared to OT. Thyroid specimens were pulled out through the left axillary incision using an endoplastic bag. The midline and the skin closure were done in a routine manner.
Lymph node dissection was performed in the same principle and same manner for both OT and BABA RT patients. A prophylactic ipsilateral central lymph node dissection was performed routinely regardless of tumor size. Bilateral central lymph node dissection was performed for the bilateral tumors.
A serum total calcium level less than 8 mg/dL with hypocalcemic symptoms during the hospitalization was defined as transient hypoparathyroidism. Permanent hypoparathyroidism was diagnosed when oral calcium supplementation was required for more than 6 months in setting serum parathyroid hormone levels of less than 5 pg/mL. Indirect laryngoscopy was performed in all patients and transient vocal cord palsy was diagnosed when the palsy lasted for less than 6 months while permanent palsy was diagnosed if the symptom lasted for more than 6 months.
The following questions were answered by the patients daily from postoperative days 1 to 3 and then at postoperative day 14; (1) voice quality, (2) throat pain, (3) anterior neck pain, (4) posterior neck pain, (5) right anterior chest pain, (6) left anterior chest pain, and (7) back pain. Each question was scored using a visual analog scale (VAS) ranging from 0 (no voice change or no pain) to 10 (worst voice change or worst pain), and the patient could mark the score by dragging a pointer with their finger (Fig. 2). Corresponding flickering red light assisted in selection visualization while Faces Pain Rating Scale was used to understand the VAS (Fig. 3). On postop day 14, the following surveys were obtained at the follow up clinic: (1) degree of wound satisfaction, (2) Voice Handicap Index-10 (VHI-10) questionnaire, and (3) 4 questions regarding the usefulness of the SRA. Pathological data including tumor size, multifocality, extrathyroidal extension, lymphovascular invasion, presence of thyroiditis, and TNM stage were retrieved from the database of Seoul National University Hospital, and they were based on the pathologic reports.
Input data were automatically uploaded to a designated website via the institutional WiFi and the data were downloaded from the website in the Microsoft Excel 2010 file format. Data input times for each question were recorded.
Results were analyzed with IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA). Univariate analysis was performed using the Student t-test for continuous variables and chi-square or Fisher exact tests for categorical variables. Differences were considered significant when P < 0.05.
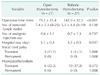
From March 2013 to May 2014, 54 patients were enrolled for the study (27 for OT, 27 for RT group). Patient demographics and clinicopathological characteristics are demonstrated in Table 1. There were no significant differences between the OT and RT groups in terms of age, body mass index, tumor size, multifocality, extrathyroidal extension, lymphovascular invasion, presence of thyroiditis, and TNM stage.
Table 2 demonstrates surgical outcomes of the OT and RT groups. RT group was associated with longer operation time (79.2 ± 25.4 minutes for OT vs. 142.0 ± 32.5 minutes for RT, P < 0.001), and longer hospital stay (3.1 ± 0.3 days for OT vs. 3.3 ± 0.5 days for RT, P = 0.037) than OT group. There was no significance difference in the number of removed lymph nodes (7.4 ± 5.3 for OT vs. 5.3 ± 4.8 for RT, P = 0.138). No significant differences were found in the total number of analgesic injections during hospitalization (0.6 ± 1.1 for OT vs. 0.7 ± 1.3 for RT, P = 0.737) or postoperative complications such as transient vocal cord palsy (11.1% for OT vs. 11.1% for RT, P = 1.000) and transient hypoparathyroidism (22.2% for OT vs. 37.0% for RT, P = 0.372). There was no complication such as open conversion from RT, tracheal injury, hematoma, chyle leak, or wound problem in either of the groups.
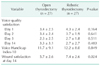
Postoperative pain scores at days 1, 2, 3, and 14 were not significantly different in the 2 groups for throat, anterior neck, posterior neck, or back (Table 3). Mean postoperative pain scores at days 1, 2, 3, and 14 were 3.6, 2.9, 2.3, and 1.4, respectively for the right chest, and 4.5, 3.2, 2.5, and 1.4, respectively for the left chest. Table 4 showed that patient satisfaction for voice quality was similar at days 1, 2, 3, and 14 in the 2 groups, and the mean VHI-10 scores at day 14 were similar between the groups (OT 11.7 ± 9.1 vs. RT 12.2 ± 8.0, P = 0.849). Wound satisfaction scores of the RT group were higher than the OT group (OT 5.7 ± 2.6 vs. RT 7.4 ± 2.6, P = 0.024). Satisfaction scores for the usefulness of SRA were 7.6 ± 2.2, 7.6 ± 2.2, 7.2 ± 2.1, and 7.5 ± 2.2 on the 10-point scale (Table 5).
With the evolution of endoscopic and robotic surgical techniques for thyroidectomy, appropriate assessment and management of postoperative pain for these patients are essential as pain management can be often overlooked amidst all the interest towards success of the novel surgical approach [9]. Furthermore, some of the patients, especially in pediatric populations, may not have acquired appropriate cognitive or social communication skills [10]. Regarding postoperative pain for BABA RT, compared to conventional open thyroidectomies which are generally well tolerated, one may expect a significantly greater pain associated with BABA RT given the wide skin flap creation.
Postoperative pain score at days 1, 2, 3, and 14 were not significantly different in the 2 groups for throat, anterior neck, posterior neck, or back, which is in concordance with the results by Ryu et al. [11], who reported that transaxillary RT does not cause more pain nor does it require more analgesic injection after surgery when compared with OT. As for possible reasons for similar pain after RT with OT, Ryu et al. [11] suggested that the axilla is less sensitive to pain and less mobile than the neck. In addition, it might be because postoperative pain is more dependent on the pressure put into the skin incision and strap muscles during the operation rather than the range of the dissection. During the BABA RT procedure, little pressure is applied to the incision sites because the robotic arms are relatively fixed and supported at pivot points, whereas the neck skin and strap muscles are extensively stretched and manipulated by retractors during OT.
Meanwhile, subcutaneous tunneling from the both areolae to the neck area is a unique process in BABA RT, and causes chest pain, which is not present in the OT group patients. Chest pain scores in the BABA RT group at days 1, 2, and 3 were considerable. However, the mean pain scores at day 14 decreased to 1.4 and the pain score of 1.4 can be considered minimum based on the pain scale of 0 to 10, and can be properly treated with usual analgesic medications.
Thyroid cancer patients choose RT mainly for the cosmetic purpose. More than 85% of the patients who undergo RT are female [612], and they do not want to leave visible scars on the neck. The cosmetic satisfaction in patients who underwent unilateral transaxillary RT was reported to be higher than patients who underwent OT [1314]. In this study, wound satisfaction scores at day 14 were significantly higher in the BABA RT group than in the OT group (7.4 ± 2.6 vs. 5.7 ± 2.6, P = 0.024), which suggests that BABA RT is superior to OT in terms of cosmesis. These results are partially limited due to the small number of study patients, and further study with larger population and longer follow-up is necessary for more accurate comparison of OT and BABA RT.
In this study, SRA was optimized to evaluate postoperative pain as objectively as possible at multiple potential pain sites. For example, we have assessed throat pain separately from anterior neck pain in order to distinguish the pain related to flap formation in BABA RT patients from routine sore throat observed in the OT patients. Another benefit of this system is the convenience of instant automatic upload of user input to the database, which can be easily retrieved in an Excel format.
Previous studies have demonstrated positive effects on management of diabetes or hypertension patients using mobile applications [1516]. Mobile applications are also useful for evaluation of medical care satisfaction for patients [17]. One limitation of such patient directed application is that it requires familiarity and active participation from the patient. Therefore, health care providers should offer appropriate education and motivation to use the application regularly. In this study, we have uploaded several educational video clips in the iPad and provided free WiFi service to encourage the use of the device. We also demonstrated that a mobile-based application can be easily used for pain assessment among the hospitalized patients, and found potential benefits in utilizing this in accurate pain assessment and immediate intervention, which are essential for pain management in the future. Further efforts to make SRA more user-friendly are necessary in order to promote facile exchange of feedback between patients and health care providers, especially in elderly or adolescent patients. For the future, in addition to being a study tool, it would be more meaningful if SRA can be used as an actual pain management tool according to the pain score with an immediate feedback method.
In conclusion, this is the first study to evaluate postoperative pain after BABA RT in comparison to OT. The results suggest that BABA RT offers greater cosmetic satisfaction without increased pain compared to OT. Furthermore, utilization of mobile applications such as SRA for pain assessment can be useful and potentially beneficial for pain management as well.
Figures and Tables
Fig. 1
Location of 4 incisions and flap dissection area (in red) for bilateral axillo-breast approach robotic thyroidectomy.
ACKNOWLEDGEMENTS
This study was supported by Korean Foundation for Cancer Research (grant number: CB-2011-03-01).
References
1. Kim WW, Kim JS, Hur SM, Kim SH, Lee SK, Choi JH, et al. Is robotic surgery superior to endoscopic and open surgeries in thyroid cancer? World J Surg. 2011; 35:779–784.
2. Kang SW, Jeong JJ, Yun JS, Sung TY, Lee SC, Lee YS, et al. Robot-assisted endoscopic surgery for thyroid cancer: experience with the first 100 patients. Surg Endosc. 2009; 23:2399–2406.
3. Lee S, Lee CR, Lee SC, Park S, Kim HY, Son H, et al. Surgical completeness of robotic thyroidectomy: a prospective comparison with conventional open thyroidectomy in papillary thyroid carcinoma patients. Surg Endosc. 2014; 28:1068–1075.
4. Lee KE, Choi JY, Youn YK. Bilateral axillobreast approach robotic thyroidectomy. Surg Laparosc Endosc Percutan Tech. 2011; 21:230–236.
5. Kim HY, d'Ajello F, Woo SU, Son GS, Lee JB, Bae JW. Robotic thyroid surgery using bilateral axillo-breast approach: personal initial experience over two years. Minerva Chir. 2012; 67:39–48.
6. Lee KE, Kim E, Koo do H, Choi JY, Kim KH, Youn YK. Robotic thyroidectomy by bilateral axillo-breast approach: review of 1,026 cases and surgical completeness. Surg Endosc. 2013; 27:2955–2962.
7. Lee KE, Koo do H, Im HJ, Park SK, Choi JY, Paeng JC, et al. Surgical completeness of bilateral axillo-breast approach robotic thyroidectomy: comparison with conventional open thyroidectomy after propensity score matching. Surgery. 2011; 150:1266–1274.
8. Lee KE, Koo do H, Kim SJ, Lee J, Park KS, Oh SK, et al. Outcomes of 109 patients with papillary thyroid carcinoma who underwent robotic total thyroidectomy with central node dissection via the bilateral axillo-breast approach. Surgery. 2010; 148:1207–1213.
9. Breivik H, Stubhaug A. Management of acute postoperative pain: still a long way to go! Pain. 2008; 137:233–234.
10. Stanford EA, Chambers CT, Craig KD. A normative analysis of the development of pain-related vocabulary in children. Pain. 2005; 114:278–284.
11. Ryu HR, Lee J, Park JH, Kang SW, Jeong JJ, Hong JY, et al. A comparison of postoperative pain after conventional open thyroidectomy and transaxillary single-incision robotic thyroidectomy: a prospective study. Ann Surg Oncol. 2013; 20:2279–2284.
12. Ban EJ, Yoo JY, Kim WW, Son HY, Park S, Lee SH, et al. Surgical complications after robotic thyroidectomy for thyroid carcinoma: a single center experience with 3,000 patients. Surg Endosc. 2014; 28:2555–2563.
13. Lee J, Nah KY, Kim RM, Ahn YH, Soh EY, Chung WY. Differences in postoperative outcomes, function, and cosmesis: open versus robotic thyroidectomy. Surg Endosc. 2010; 24:3186–3194.
14. Tae K, Ji YB, Cho SH, Lee SH, Kim DS, Kim TW. Early surgical outcomes of robotic thyroidectomy by a gasless unilateral axillo-breast or axillary approach for papillary thyroid carcinoma: 2 years' experience. Head Neck. 2012; 34:617–625.
15. Årsand E, Froisland DH, Skrovseth SO, Chomutare T, Tatara N, Hartvigsen G, et al. Mobile health applications to assist patients with diabetes: lessons learned and design implications. J Diabetes Sci Technol. 2012; 6:1197–1206.
16. Hallberg I, Taft C, Ranerup A, Bengtsson U, Hoffmann M, Hofer S, et al. Phases in development of an interactive mobile phone-based system to support self-management of hypertension. Integr Blood Press Control. 2014; 7:19–28.
17. Turney BW, Reynard JM. Obtaining patient feedback in an outpatient lithotripsy service is facilitated by use of a touchscreen tablet (iPad™) survey. Urolithiasis. 2014; 42:317–321.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download