Abstract
Purpose
Ankaferd Blood Stopper (ABS) is an herbal extract attained from 5 different plants. It has the therapeutic potential to be used for the management of external hemorrhage and controlling gastrointestinal bleedings. To date, the safety of ABS for intraperitoneal usage is not clear. In this study, we investigated the effectiveness and safety of using intraperitoneal ABS in an experimental peritoneal adhesion model.
Methods
Twenty-four male Wistar Albino rats were used in the study. The rats were randomly divided into 3 groups: saline, ABS, and control. On the 10th day, all rats were euthanized. The adhesions were evaluated by Nair's macroscopic adhesion classification, and pathologically evaluated with Zühlke's microscopic adhesion classification.
The most common cause of peritoneal adhesion (PA) is abdominal surgery. A number of mechanisms have been proposed as potential triggering factors in the development postsurgical PA [1]. To date, several treatment modalities have been performed to prevent postsurgical PA [234]. However, no effective treatment has yet been validated.
Ankaferd blood stopper (ABS) is an herbal extract derived from five different plants and each 100 mL of liquid contains a standard mixture of: 5-mg Thymus Vulgaris, 9-mg Glycyrrhiza glabra, 8-mg Vitis vinifera, 7-mg Alpinia officinarum, and 6-mg Urtica dioica [5]. It forms a system by precipitating fibrinogen and forming a protein network, which acts as an anchor for vital physiological erythrocyte aggregation, covering the classical cascade model of the clotting system, independently acting on the coagulation factors and platelets in the blood and serum [5]. It has the therapeutic potential to be used for the management of external hemorrhage and controlling gastrointestinal bleedings [67]. The topical use of ABS has been approved by the Turkish Ministry of Health for the management of dermal, external postsurgical, and postdental surgery bleeding [5]. Besides its homeostatic activity, ABS has antineoplastic actions and an in vitro anti-infectious affect [89]. Several experimental studies investigated the effect of ABS on inflammation and fibrosis in the bladder, liver and renal tissues [101112]. To date the safety of ABS for intraperitoneal usage is not clear. In this study, we investigated the effectiveness and safety of using intraperitoneal ABS in an experimental PA model.
The study was approved by the Institutional Animal Use and Care Committee of Ankara Education and Research Hospital and performed in accordance with the National Institute of Health Guidelines. Twenty-four male Wistar Albino rats were used in the study, with a mean age of four months and mean weight of 200–280 g. All the animals were fed standard food and water. Twelve hours before the study procedure, feeding was stopped and the rats were only allowed to drink water. On the day of induction, all the rats were anesthetized with intramuscular ketamine (8 mg/kg) and a 5 mg/kg intramuscular dose of xylazine. Following anesthesia, the midline of the abdomen was shaved and antisepsis was provided with povidone iodine. The peritoneal cavity was entered through a 3-cm vertical midline incision. The cecum and terminal ileum were explored and placed on a damp gauze pad. Cecum and a segment of the terminal ileum measuring 2 cm were scraped with a dry gauze pad. This procedure was carried out until a focus of petechial hemorrhage was observed (scraping model) [13]. The rats were randomly divided into 3 groups:
Group I (saline group, n=8): Cecum was exposed and abraded by a dry cloth until bleeding. Thereafter, 3–4 mL of intraperitoneal saline solution was given.
Group II (ABS group, n=8): Cecum was exposed and abraded by a dry cloth until bleeding. Thereafter, and 3–4 mL of intraperitoneal ABS was given.
Group III (control group, n=8): Cecum was exposed and abraded by a dry cloth until bleeding.
All the laparotomy wounds were closed using 4/0 silk sutures.
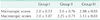
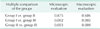
On the 10th day, all the rats were euthanized with a high dose of ketamine. A reverse U shaped incision was made in order to observe the entire adhesion site and to perform an accurate adhesion grading. The adhesions were evaluated using Nair's macroscopic adhesion classification [14] (Table 1). Subsequently, the ileum and the cecum were totally excised for evaluation by a single blind pathologist using Zühlke's microscopic adhesion classification [15] (Table 2).
For statistical analysis, both the macroscopic and microscopic adhesion classification grades were interpreted as numbers (i.e., grade 0=0, grade 1=1, grade 2=2, grade 3=3, grade 4=4). All the results were reported as mean ± standard error of the mean. The statistical analyses were performed using the SPSS ver. 11.5 (SPSS Inc., Chicago, IL, USA). Due to the limited number of rats in each group, nonparametric methods were used for statistical analysis. To compare the means of two or more groups, Kruskal-Wallis variance analysis was used to determine whether there was a statistical difference between the groups. A P-value of less than 0.05 was accepted as significant.
The results of the macroscopic and microscopic evaluation are shown in Table 3 and the comparison results, as the P-values between the groups, are shown in Table 4.
In this study, according to Nair's macroscopic evaluation, intra-abdominal adhesions were found to be significantly less in the saline group when the control and saline groups were compared, and significantly less in the ABS group when the control and ABS groups were compared (P < 0.002 and P < 0.008, respectively). No statistically significant difference was found between the saline and ABS groups.
Microscopic Zühlke evaluation revealed that, Intra-abdominal adhesions were found to be statistically significantly lower in saline and ABS groups compared to the control group when control group and saline and ABS groups were compared (P < 0.002 and P < 0.003, respectively). No statistically significant difference was found between the other groups.
When examined both macroscopically and microscopically, the formation of a lesser amount of adhesion in the ABS group compared to the control group can be interpreted as ABS decreasing intra-abdominal adhesion.
ABS System is a stable solution that contains five different herbal extracts. It has been proven for use in cases with arterial or venous bleeding.
We planned this research because the number of previous studies, which investigated the potential effects of ABS on abdominal adhesion formation following its use for bleeding, was insufficient.
Adhesions are the common results of all kinds of abdominal procedures: all foreign bodies (i.e., talc of the gloves, sutures), which come into direct contact with the peritoneum, can cause adhesions. The formation of adhesions causes either postoperative restrictions on bowel movements and a decline in the quality of life or the mechanical ileus that may require further operations. For that reason, all materials used in the abdomen must be evaluated for their adhesion formation potential. Adhesion formation starts on the 5th–7th days following trauma [16] and so the most appropriate evaluation must be done after the 7th day, postoperatively [17]. Therefore, in our study we evaluated the adhesions on the 10th postoperative day.
An important point that differentiated this study from the others was the concentration and application dose of ABS. The concentration and viscosity of the ABS are important parameters concerning adhesion formation [2,18,19]. In previous studies diluted ABS was used but in our study we used the undiluted form. Although the fact that kidney and liver tissues were not fragile macroscopically in this present study, and there was no bleeding or color change on organ surfaces, and no occasion of rat death occurred during the study, gives rise to the thought that ABS does not have an acute toxic effect. Further studies are needed to carry out the aim of evaluating the toxic effects of ABS.
We considered this to be an indicator for the safety of this material for intra-abdominal applications.
In one of the previous studies, it was noted that abdominal ABS applications resulted in acute and chronic inflammatory changes on the serosal surfaces of intestines, and minor structural changes in the liver. But these changes were not evaluated as toxic [20]. On the other hand, in our study application of ABS did not cause any toxic changes on the serosal surfaces of the intestines. We only observed a brownish color change on the serosal surfaces following the application. Only one study depicting a similar color change on intestinal serosal surfaces attributed to encapsulating protein network was found in the literature search [21].
Our results indicated that the adhesion formation potential of ABS in the microscopic evaluation was equal to that of saline and the saline and ABS groups were found to be effective in the prevention of intra-abdominal adhesion formation compared with the control group. These results establish that intra-abdominal use of nondiluted ABS decreases intra-abdominal adhesion formation compared to the control group. In the macroscopic evaluation, the ABS group was found to be significantly superior compared with the control group, demonstrating the adhesion preventing effects of ABS.
Various methods have been employed in the prevention of intra-abdominal adhesions. In some studies saline irrigation has been applied, which can be used in open or laparoscopic cases, and has been established to decrease adhesion formation [2223]. The results of this present study are also compatible with this finding. Furthermore, in this present study, the adhesion preventing effect in the saline group and the ABS group were found to be similar and superior to the control group. As such, it can be inferred that both saline and ABS decrease the formation of intra-abdominal adhesions and ABS can be safely used for intra-abdominal bleeding without any fear of increasing the risk of adhesion formation.
In previous studies, there was evidence of the anti-inflammatory and antineoplastic effects of ABS. ABS also decreases incidences of the necrotic processes and does not have any foreign body reaction potential on the application site [8,9,24]. Due to its anti inflammatory properties, we anticipated a lower adhesion formation potential for ABS, and this was proved by the results, as adhesion formation for ABS was similar to that of saline.
Because of the restrictions of the local ethics committee, the number of animals used for this study was limited. Although this was a negative factor concerning the power of the results, this experiment, taken as a first step study, contributed a positive indication of the possibly low potential of ABS on the formation of abdominal fibrosis.
The positive effects of ABS on the prevention of fibrosis formation were previously shown in studies on the bladder, liver, and kidneys [101112]. In our study, a similarly preventive effect of ABS and saline on fibrosis formation was observed macroscopically. Our results therefore support previous studies on fibrosis formation.
In previous studies, which investigated the effects of ABS on adhesion formation in the abdomen, it was observed that ABS did not cause an increase in adhesion formation. In a study using different methodology, we investigated the potential adhesion formation effect of ABS in an intra-abdominal bleeding model. This preliminary study conducted on a restricted number of animals, due to ethical limitations, is the first of its kind to have investigated the potential inhibitory effect of ABS on adhesion formation in intra-abdominal bleeding using the drug in a standard concentration. We observed that ABS, when used in the abdomen for intra-abdominal bleeding, has a similar adhesion formation potential to saline. We consider that these early results should be supported by further detailed studies.
ACKNOWLEDGEMENTS
The preliminary results of this study were presented at the 48th Congress of the European Society for Surgical Research (ESSR), Istanbul, Turkey, in 2013.
References
1. Davey AK, Maher PJ. Surgical adhesions: a timely update, a great challenge for the future. J Minim Invasive Gynecol. 2007; 14:15–22.
2. Aysan E, Basak E, Kinaci F, Yanar H, Coskun H. Experimental adhesion model: effect of viscosities of fluids put in the peritoneal cavity on preventing peritoneal adhesions. Exp Anim. 2007; 56:349–354.
3. Tarhan OR, Barut I, Sutcu R, Akdeniz Y, Akturk O. Pentoxifylline, a methyl xanthine derivative, reduces peritoneal adhesions and increases peritoneal fibrinolysis in rats. Tohoku J Exp Med. 2006; 209:249–255.
4. Muller SA, Treutner KH, Haase G, Kinzel S, Tietze L, Schumpelick V. Effect of intra-peritoneal antiadhesive fluids in a rat peritonitis model. Arch Surg. 2003; 138:286–290.
5. Gungor G, Goktepe MH, Biyik M, Polat I, Tuna T, Ataseven H, et al. Efficacy of ankaferd blood stopper application on non-variceal upper gastrointestinal bleeding. World J Gastrointest Endosc. 2012; 4:556–560.
6. Kurt M, Disibeyaz S, Akdogan M, Sasmaz N, Aksu S, Haznedaroglu IC. Endoscopic application of ankaferd blood stopper as a novel experimental treatment modality for upper gastrointestinal bleeding: a case report. Am J Gastroenterol. 2008; 103:2156–2158.
7. Shorbagi A, Sivri B. Successful management of a difficult case of radiation proctopathy with Ankaferd BloodStopper: a novel indication (with video). Gastrointest Endosc. 2010; 72:666–667.
8. Turhan N, Kurt M, Shorbagi A, Akdogan M, Haznedaroglu IC. Topical Ankaferd Blood Stopper administration to bleeding gastrointestinal carcinomas decreases tumor vascularization. Am J Gastroenterol. 2009; 104:2874–2877.
9. Tasdelen Fisgin N, Tanriverdi Cayci Y, Coban AY, Ozatli D, Tanyel E, Durupinar B, et al. Antimicrobial activity of plant extract Ankaferd Blood Stopper. Fitoterapia. 2009; 80:48–50.
10. Kilic O, Gonen M, Acar K, Yurdakul T, Avunduk MC, Esen HH, et al. Haemostatic role and histopathological effects of a new haemostatic agent in a rat bladder haemorrhage model: an experimental trial. BJU Int. 2010; 105:1722–1725.
11. Kalayci MU, Soylu A, Eroglu HE, Kubilay D, Sancak B, Ugurluoglu C, et al. Effect of ankaferd blood stopper on hemostas is and histopathological score in experimental liver injury. Bratisl Lek Listy. 2010; 111:183–188.
12. Huri E, Haznedaroglu IC, Akgul T, Astarci M, Ustun H, Germiyanoulu C. Biphasic effects of ankaferd blood stopper on renal tubular apoptosis in the rat partial nephrectomy model representing distinct levels of hemorrhage. Saudi Med J. 2010; 31:864–868.
13. Elkins TE, Bury RJ, Ritter JL, Ling FW, Ahokas RA, Homsey CA, et al. Adhesion prevention by solutions of sodium carboxymethylcellulose in the rat. I. Fertil Steril. 1984; 41:926–928.
14. Nair SK, Bhat IK, Aurora AL. Role of proteolytic enzyme in the prevention of postoperative intraperitoneal adhesions. Arch Surg. 1974; 108:849–853.
15. Zuhlke HV, Lorenz EM, Straub EM, Savvas V. Pathophysiology and classification of adhesions. Langenbecks Arch Chir Suppl II Verh Dtsch Ges Chir. 1990; 1009–1016.
16. Holmdahl L, Risberg B, Beck DE, Burns JW, Chegini N, diZerega GS, et al. Adhesions: pathogenesis and prevention-panel discussion and summary. Eur J Surg Suppl. 1997; (577):56–62.
17. Holmdahl L, al-Jabreen M, Risberg B. Experimental models for quantitative studies on adhesion formation in rats and rabbits. Eur Surg Res. 1994; 26:248–256.
18. Rasa K, Erverdi N, Karabulut Z, Renda N, Korkmaz A. The effect of methylene blue on peritoneal adhesion formation. Turk J Gastroenterol. 2002; 13:108–111.
19. Kluger Y, Weinbroum A, Ben-Avraham R, Galili Y, Klausner J, Rabau M. Reduction in formation of peritoneal adhesions by methylene blue in rats: a dose response study. Eur J Surg. 2000; 166:568–571.
20. Comert M, Karakaya K, Barut F, Karadeniz Cakmak G, Ucan HB, Gultekin FA, et al. Does intraabdominal use of Ankaferd Blood Stopper cause increased intraperitoneal adhesions? Ulus Travma Acil Cerrahi Derg. 2010; 16:383–389.
21. Kandemir O, Buyukates M, Kandemir NO, Aktunc E, Gul AE, Gul S, et al. Demonstration of the histopathological and immunohistochemical effects of a novel hemostatic agent, Ankaferd Blood Stopper, on vascular tissue in a rat aortic bleeding model. J Cardiothorac Surg. 2010; 5:110.
22. Elkelani OA, Molinas CR, Mynbaev O, Koninckx PR. Prevention of adhesions with crystalloids during laparoscopic surgery in mice. J Am Assoc Gynecol Laparosc. 2009; 9:447–452.
23. Larsson B, Lalos O, Marsk L, Tronstad SE, Bygdeman M, Pehrson S, et al. Effect of intraperitoneal instillation of 32% dextran 70 on postoperative adhesion formation after tubal surgery. Acta Obstet Gynecol Scand. 1985; 64:437–441.
24. Isler SC, Demircan S, Cakarer S, Cebi Z, Keskin C, Soluk M, et al. Effects of folk medicinal plant extract Ankaferd Blood Stopper on early bone healing. J Appl Oral Sci. 2010; 18:409–414.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download