Abstract
5-Fluorouracil (5-FU) based chemotherapy has been commonly used to treat metastatic or advanced colon cancer as an adjuvant chemotherapy. Although the side effects of 5-FU such as gastrointestinal problems and neutropenia and thrombocytopenia are common, not many cases of 5-FU related encephalopathy are reported. Hyperammonemic encephalopathy is a rare central nervous system toxicity following 5-FU chemotherapy manifesting as altered mental status with elevated ammonia levels with no radiologic abnormality. We report one case of 5-FU induced hyperammonemic encephalopathy occurring after Folfox4 (oxaliplatin, folinic acid and 5-fluorouracil) chemotherapy in a colon cancer patient who presented with confused mental status soon after the chemotherapy and review the 5-FU related encephalopathy.
Colon cancer is the second most common malignancy except for the thyroid cancer in Korea is the one of the leading cause of cancer related mortality. Colon cancer is well known for its excellent responsiveness to chemotherapy compared with the other gastrointestinal tract cancer and chemotherapy has been performed on patients with advanced colon cancer as an adjuvant or palliative treatment modality.
5-Fluorouracil (5-FU) based chemotherapy has been widely used to treat metastatic or advanced colon cancer as an adjuvant chemotherapy [1]. The common side effects related with 5-FU are gastrointestinal problems including nausea, vomiting, diarrhea and stomatitis and neutropenia and thrombocytopenia originating from bone marrow suppression. However, not many cases of 5-FU related encephalopathy are reported. Hyperammonemic encephalopathy is a rare central nervous system toxicity after 5-FU chemotherapy and it manifests with altered mental status without any radiologic abnormality or abnormal laboratory finding except for elevated ammonia levels.
We report one case of 5-FU induced hyperammonemic encephalopathy that occurred soon after Folfox4 (oxaliplatin, folinic acid and 5-fluorouracil) chemotherapy for a colon cancer patient in which the patient presented with confused mental status, with a review of the 5-FU induced encephalopathy.
A 59-year-old female underwent curative surgical resection for stage IIb (T4aN0) rectal cancer. About 4 weeks after surgery, she was admitted for her first cycle of FOLFOX4 chemotherapy, which consisted of oxaliplatin 85 mg/m2 on day 1 and levofolic acid 100 mg/m2, and 5-FU 400-mg/m2 bolus and 600 mg/m2 by continuous infusion for 22 hours on days 1 and 2.
On the first day of chemotherapy, she had no specific complaint except for mild nausea. The next day, she suffered severe nausea and vomiting. On the morning of the third day of chemotherapy, she showed confused mental status during 5-FU infusion. She showed no response to verbal commands, and right-sided eye deviation was observed. Patient vital signs did not reveal any abnormality and there was no the other neurologic deficit. Laboratory finding showed no electrolyte disturbance, but metabolic acidosis with respiratory compensation and lactic acidosis were seen. The patient's ammonia level was markedly increased to 629 µg/dL (normal range, ~75 µg/dL) but other liver function test results were in the normal range.
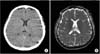
There was no abnormal finding in her imaging studies performed before the chemotherapy (Figs. 1, 2). Electroencephalography showed frontal intermittent rhythmic delta activity but no seizure activity was seen. Brain image study including brain CT and MRI did not show any abnormality (Fig. 3).
We immediately stopped infusion of 5-FU and an anticonvulsant was given 2 times. Eye deviation slightly improved but mental status remained in a confused state.
She was transferred to intensive care unit, and along with hydration, we performed a lactulose enema to lower the ammonia levels. After we performed the enema twice, the ammonia levels dramatically dropped to the normal range (44 µg/dL) and the patient's mental status improved so that she could communicate appropriately. However, she felt fatigue and general weakness and her metabolic acidosis continued and PCO2 was low. Thus, we had her breathe into a vinyl bag to induce CO2 retention, then the acidosis improved gradually. The next day, which was the fourth day of chemotherapy, all the laboratory findings improved to within the normal range and the patient's mental status also completely recovered. We observed the patient for 2 days more, and then the patient was discharged. We decided to change the regimen to capecitabine only (capecitabine twice a day for 14 days) and she was admitted after a month for the chemotherapy. Symptoms were observed and she was discharged after three days without any problem. She is presently receiving the capecitabine and no adverse event has been noted until now.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
As an adjuvant treatment modality for advanced colon cancer, FOLFOX regimen is considered a primary regimen. With our patient, we started chemotherapy with a FOLFOX4 regimen and she presented symptoms of altered mental status on the third day of the first cycle of chemotherapy during 5-FU infusion. The diagnosis of chemotherapy induced encephalopathy is an exclusive diagnosis. In our patient's case, she had no past history or use of medication that could cause encephalopathy, and there was no abnormal laboratory finding before the chemotherapy and no abnormal neurologic finding on MRI study. And because she developed the symptoms during 5-FU infusion and the symptom improved after ceasing the infusion and supportive treatment, we could make the diagnosis of chemotherapy-induced encephalopathy.
Regarding encephalopathy after FOLFOX chemotherapy, posterior reversible encephalopathy, Wernike's encephalopathy, and hyperammonemic encephalopathy have been reported [23]. With our patient, we could reach the conclusion of chemotherapy-induced hyperammonemic encephalopathy because the patient's brain images did not show abnormal findings, and there is no abnormal laboratory findings to indicate altered mentality except for markedly increased ammonia levels.
In the literature review, only one case has been reported on hyperammonemic encephalopathy related to oxaliplatin after FOLFOX chemotherapy, and in most cases, hyperammonemic encephalopathy developed in association with infusion of 5-FU [4].
5-FU induced encephalopathy has been reported in 5.7% of patients treated with high dose 5-FU chemotherapy and it is known that two different pathogenesis contribute to development of 5-FU induced encephalopathy. The first is dihydropyrimidine dehydrogenase (DPD) deficiency type. DPD is a major enzyme inactivating 5-FU and in patients with DPD deficiency, symptoms may occur associated with 5-FU accumulation. DPD deficiency is reported in 2.7% of cancer patients and it is thought to be due to DPD gene mutation encoding DPD enzymes. High concentrations of 5-FU in the DPD deficiency penetrate into CSF and cause acute demyelination of neurons. In our case, we were unable to confirm the presence of DPD deficiency but we believe this mechanism is not a suitable explanation because the ammonia, which is a catabolite of 5-FU, was markedly increased in our patient. The second is a 5-FU catabolite type that is known as a milder type than DPD deficiency. According to this mechanism, major catabolic pathways are intact and transient accumulation of 5-FU catabolite cause encephalopathy by high rates of infusion of 5-FU. Koenig et al. [5] explained that large-dose administration of 5-FU induces accumulation of fluoroacetate and directly inhibits the Kreb's cycle. Hence, transient hyperammonemia develops due to impairment of ATP-dependent urea cycle.
As an aggravating factor of 5-FU induced encephalopathy, renal dysfunction and dehydration, constipation and body weight loss might be attribute to its development. In patients with renal dysfunction or patients in a dehydrated state, blood levels of 5-FU catabolite such as fluoroacetate or ammonia will increase thus causing encephalopathy [6]. In our patient, there was no predisposing factor that may cause development of encephalopathy. However, she complained of intractable nausea and vomiting before the altered mental status presented, thus there is the possibility that dehydration might be attributed to the development of encephalopathy.
As of yet, there is no solid strategy regarding the treatment of 5-FU induced hyperammonemic encephalopathy. When 5-FU induced hyperammonemic encephalopathy is suspected, the immediate stop of 5-FU infusion is necessary. Then, along with large volume hydration, diagnostic procedures including laboratory tests and imaging studies should be performed for differential diagnosis. In most cases, patients with 5-FU-induced hyperammonemic encephalopathy improved without complication after supportive treatment including discontinuation of 5-FU, hydration, and lactulose enema. Our patient also recovered dramatically within 24 hours after ceasing the infusion of 5-FU, fluid supplement, and lactulose enema. We did not administer branched-chain amino acid, but some studies have reported that branched-chain amino acid showed excellent results when administered to patients with hyperammonemia [7].
Although most cases of 5-FU induced encephalopathy spontaneously improve, recurrence is possible when it is given to the same patient. Thus, it is very difficult to make a decision as to what we should choose as alternative treatment modality. A few centers performed single-agent chemotherapy with oxaliplatin or irrinotecan, raltitrexed without 5-FU, but the outcomes were disappointing [8]. On the other hand, according to a report about the application of tegafur-uracil (tegafur, uracil in a molar ratio 1:4), taking tegafur (oral 5-FU prodrug) with uracil, which is a natural substrate for DPD, 5-FU is slowly released by the inclusion of uracil thus reducing the side effects of 5-FU catabolite by preventing rapid degradation of 5-FU [9]. In some cases, by reducing the dose of infusional 5-FU or exchanging it with capecitabine, which is an oral 5-FU prodrug, chemotherapy was done successfully without recurrence [10]. We also changed the regimen to oral chemotherapy using capecitabine and it was successful. However, close monitoring will be needed because a few cases have reported that capacitabine could also induce encephalopathy.
Figures and Tables
References
1. Mayer RJ. Moving beyond fluorouracil for colorectal cancer. N Engl J Med. 2000; 343:963–964.
2. Porcello Marrone LC, Marrone BF, Pascoal TA, Schilling LP, Soder RB, Ferreira SS, et al. Posterior Reversible Encephalopathy Syndrome Associated with FOLFOX Chemotherapy. Case Rep Oncol Med. 2013; 2013:306983.
3. Truman N, Nethercott D. Posterior reversible encephalopathy syndrome (PRES) after treatment with oxaliplatin and 5-fluorouracil. Clin Colorectal Cancer. 2013; 12:70–72.
4. Chang YY, Lin JK, Jiang JK. Oxaliplatin-related hyperammonaemic encephalopathy in a patient with colon cancer. Colorectal Dis. 2012; 14:e821.
5. Koenig H, Patel A. Biochemical basis for fluorouracil neurotoxicity. The role of Krebs cycle inhibition by fluoroacetate. Arch Neurol. 1970; 23:155–160.
6. Kikuta S, Asakage T, Nakao K, Sugasawa M, Kubota A. The aggravating factors of hyperammonemia related to 5-fluorouracil infusion: a report of two cases. Auris Nasus Larynx. 2008; 35:295–299.
7. Teraishi F, Suzuki T, Nakamoto M, Chikuba A, Nezu M, Shimamura H, et al. A case of hyperammonemic encephalopathy in a patient with recurrent colon cancer treated with modified FOLFOX6. Gan To Kagaku Ryoho. 2009; 36:867–869.
8. Volk J, Reinke F, van Kuilenburg AB, van Gennip AH, Schlichting C, Ganser A, et al. Safe administration of irinotecan, oxaliplatin and raltitrexed in a DPD-deficient patient with metastatic colon cancer. Ann Oncol. 2001; 12:569–571.
9. Malet-Martino M, Martino R. Clinical studies of three oral prodrugs of 5-fluorouracil (capecitabine, UFT, S-1): a review. Oncologist. 2002; 7:288–323.
10. Advani PP, Fakih MG. 5-FU-induced hyperammonemic encephalopathy in a case of metastatic rectal adenocarcinoid successfully rechallenged with the fluoropyrimidine analog, capecitabine. Anticancer Res. 2011; 31:335–338.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download