Abstract
Purpose
This retrospective study was an investigation of overall survival (OS), disease-free survival (DFS) and prognostic factors affecting OS and DFS in cirrhotic patients who received intraoperative radiofrequency ablation (IORFA).
Methods
Between April 2009 and November 2013, 112 patients (94 men, 84%; 18 women, 16%) underwent IORFA for 185 cases of hepatocellular carcinomas (HCC). Repeat IORFA was done in 9 patients during the same period (total of 121 treatments).
Results
All patients were followed-up for at least 12 months (mean follow-up, 32 months). Surgical resection combined with IORFA was performed in 20 patients. The technical effectiveness at 1 week was 91.78% (111 of 121). Readmission was 9.1% (11 of 121) and the most common cause was ventral hernia. Procedure-related mortality was 2.7% (3 of 112) and continued fatal biliary leakage was 1.8% (2 of 112). Local recurrence developed in 10 patients (8.9%). Most recurrence was intrahepatic. Cumulative survival was assessed in 33 patients who received IORFA as primary treatment (naive patients) and 79 non-naive patients. The cumulative DFS and OS rate at l and 3 years was 54% and 24%, and 87% and 66%, respectively. Moderate ascites (P = 0.001), tumor located segment I (P = 0.001), portal vein thrombosis (P = 0.001) had poor survival were significant factors by multivariate analysis.
Hepatocellular carcinoma (HCC) commonly develops in patients with cirrhosis. Treatment options are limited in most patients with HCC because of inadequate functional hepatic reserve and multinodularity. Repeated treatments are required by the individual HCC progression [1]. Surgical resection has been the best treatment option for patients with HCC. However, this option is often not indicated for various reasons including the presence of multiple bilobar tumors, invasion or close proximity of tumor to major vessels or bile ducts, limited liver function, or high surgical risk due to comorbidities. Moreover, tumor recurrence is common after curative resection [23].
When the surgical resection is not safe in most HCC patients with cirrhosis, radiofrequency ablation (RFA) could be considered as alternative treatment modality, which is being rapidly adopted for its potential benefits, including reduced morbidity and mortality [4]. RFA is a new local thermal ablation modality, which has been increasingly investigated recently with advances in technology, such as percutaneous, laparoscopic, intraoperative approaches, and development of special RFA devices. In addition, RFA preserves more of the hepatic parenchyma than surgical resection, which is crucial especially in patients whose whole hepatic functional reserve is limited. Due to unfavorable location of the tumors, a proportion (9%) of HCC cannot be treated by percutaneous RFA [5].
Intraoperative radiofrequency ablation (IORFA) offers many advantages, as compared to the percutaneous and laparoscopic approaches. The placement of the RFA electrode is more accurate and safe, which may be the reason for improved tumor control in the case of open surgical approach. Thus IORFA may extend the feasibility of surgery in the case of multiple tumors [67]. The recently introduced hepatectomy in combination with RFA for multifocal hepatic tumors could expand the range of patients for hepatic resection eradicating all sonographically detectable tumors and preserving hepatic reserve [89].
The purpose of this study was to evaluate the clinical features, changing trends of treatment modality, comorbidities, long-term survival and prognostic factors associated with curative treatment. IORFA for HCC were performed in cases that could not be treated percutaneously due to risky nodules adjacent to a large vessel or extrahepatic organ or subcapsular locations or cases where the surgical resection was not feasible in a large series at a single center.
Between April 2009 and November 2013, 112 patients underwent IORFA with or without hepatic resection. HCC was diagnosed in accordance with the Korean Liver Cancer Study Group Guideline, based on the combination of characteristic image findings at dynamic CT or MRI, and elevated serum α-FP levels in patients with chronic hepatitis B, hepatitis C, or liver cirrhosis. Patients were excluded from IORFA if their platelet count was <40,000/mL. If platelet transfusion corrected the abnormal values, the patients received treatment. Laparotomy was performed by a surgeon and IORFA by a radiologist. Indication for IORFA, surgical resection, and the combination of both was made individually and the decision was only determined intraoperatively according to the location and extent of tumor, ascites and degree of cirrhosis, severity of adhesion, risk of major vessel or hepatic duct injury, and expected loss of functional liver volume. Hepatic resection was generally performed before IORFA. When considering IORFA, the initial treatment planned involved 1 ablation for tumor of <2 cm in diameter and ≥2 ablations with overlapping techniques for tumors of ≥2 cm in diameter and at least a l-cm zone of normal liver parenchyma. Real time visualization of the target lesion is sometimes difficult because of shape change and coarse parenchymal echogenicity in cirrhotic liver. HCC nodules that contain few Kupffer cells, are clearly delineated as a contrast defect (Kupffer imaging). Sonazoid (Daiichi Sankyo, Tokyo, Japan) has been used clinically since January 2013. The technical effectiveness of ablation was presently assessed by CT 1 week postoperatively. If incompletely treated, viable tumors were detected, then the patients were immediately retreated with percutaneous RFA or transarterial embolization (TAE). Local recurrence was defined as recurrence at surgical bed after R0 resection or when subsequent CT demonstrated tumor growth and enhancement within or along the margin of ablation zone where the technique was considered to be completely effective. Intrahepatic distant recurrence was defined when new tumor growth appeared remote from the ablation zone. For purpose of this study, the following were collected: patient age and sex, cause and degree of liver cirrhosis, associated disease, tumor markers (α-FP, Pivka), previous treatment, and IORFA decision criteria. Tumor number, location, size, type of surgery, operative details, recurrence and their treatments, complication data, follow-up and death data, and cause of death. Disease status was defined as no evidence of disease, alive with disease, and dead of disease. Treatment mortality was defined as any death within 30 days after the procedure.
Data were summarized using descriptive statistics: frequency and percentage for categorical variables and mean and standard deviation for continuous variables. OS was estimated using Kaplan-Meier curves and defined as the time from RFA to death. DFS was defined as the time from RFA to recurrence or death. Survival curves were compared between groups using the log-rank test. Univariate analyses of prognostic factors were performed using Cox regression to examine differences with respect to OS and DFS. Multivariate analysis using Cox regression was performed to identify prognostic factors, which are independently related to OS and DFS. All P-values <0.05 were considered statistically significant. This study was explorative in nature and therefore no adjustment for multiple testing was applied. All statistically analyses were carried out using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA) and MedCalc 11.6.0 (MedCalc, Ostend, Belgium).
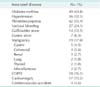
All surviving patients were followed-up for at least 12 months after IORFA. Among 92 hepatitis B/or/and C patients, antiviral titers were stable in 65 patients (68%) and unstable in 30 patients (32%) during follow-up. During the study period, 112 patients were treated using IORFA (Table 1); these comprised 94 men (84%) and 18 women (16%), with a median age of 61.3 years (range, 38–82 years). The etiologic factors for cirrhosis were chronic hepatitis B (n = 70, 62.5%), chronic hepatic C (n = 22, 19.6%) virus infection, both hepatitis B and C infections (n = 4, 3.5%), chronic ethanol ingestion (n = 9, 8%), cryptogenic (n = 6, 5.4%), and primary biliary cirrhosis (n = 1, 0.9%). Child-Turcotte-Pugh class at time of IORFA treatment was A in 71 patients (63.4%), B in 37 patients (33%), and C in 4 patients (3.6%). Combined comorbidities were listed in Table 2. The time lag between HCC diagnosis and performing IORFA was <1 year in 52 patients (46.4%) and >1 year in 60 patients (53.6%). Tumor diameter was <3 cm in 105 patients (93.8%) and >3 cm in 7 patients (6.3%). The median diameter was 1.87 ± 0.83 cm (range, 0.6–5 cm). The number of tumor nodules was 1 in 87 patients (77.7%), >2 in 25 patients (22.3%), with a median number of 1.30 ± 0.66 (range, 1–5). The distribution of tumor nodules was in segment I (n =7, 6.3%) and other segments (n = 105, 93.8%).
IORFA as a primary treatment was 33 (naive patients, 29%), other previous primary treatment modalities were TAE (n = 39, 35%), percutaneous RFA (P-RFA; n = 34, 30%), and surgical resection (n = 6, 5%). (non-naive patients, 71%). Before IORFA, previous treatments conducted using more than twice comprised 50 patients (44.6%) and less than once in 62 patients (56.4%), with a median incidence of 2.0 ± 2.5 (range, 0–11).
American Society of Anesthesiologists Physical Status (ASAPS) scale was classified as ASA 1 (n = 1, 0.9%), ASA 2 (n = 37, 33%), ASA 3 (n = 74, 66%). For measurement of liver functional reserve, indocyanine green (ICG) clearance test was adopted and median ICG clearance rate 15 mintes (ICG R15) was 29.6% (range, 6%–89%). To correct preoperative thrombocytopenia, platelet transfusion was carried out in 44 patients (39%). During the operation, 8 patients (7%) were transfused with over 1L of blood product. Open celiotomy was performed by subcostal or midline skin incision in 91 patients (81%), previous skin incision in 14 patients (12.5%), hand assisted in 5 patients (4%), and laparoscopically in 2 patients (1.6%). Upon initial exploration, the severity of liver cirrhosis was mild (n = 18, 16%), moderate (n = 50, 45%), and severe (n = 44, 39%). Ascites was absent (n = 72, 64.3%), slight (n = 27, 24%), or moderate (n = 13, 11.6%). Decision for performing IORFA was planned preoperatively in 71 patients (63.4%) and intraoperatively in 41 patients (36.6%). IORFA was performed for several reasons. The most common was failed TAE due to the inability to define the tumor feeder or recurrence at previous P-RFA or TAE site (n = 33, 29.5%), high ICG R15 value (n = 27, 24%), severe adhesion due to previous TAE or P-RFA, or poor visibility of tumor nodule on ultrasonic examination (n = 28, 25%), risk of injury to the adjacent organs, large portal vein, hepatic vein, bile duct, or located in segment I (n = 20, 18%), and patient request (n = 4, 3%). Of the 112 patients treated with IORFA, 20 (18%) underwent additional hepatic resection. A wedge resection was performed in 14 patients, single hepatic segmentectomy was conducted in 3 patients, left lateral segmentectomy was performed in 2 patients, and right lobectomy was performed in 1 patient. Cholecystectomy was performed in 21 patients to facilitate either resection or IORFA of a segment. Three IORFA-associated complications occurred: 1 partial thickness serosal tearing to the adjacent stomach and 2 diaphragmatic perforations due to severe adhesion. All were repaired immediately at time of injury. The median operative time for the IORFA procedure was 2.9 hours (range, 1.5–9 hours). The pathologic report of resected specimen were well differentiated (n = 8), moderately differentiated (n = 9), and poorly differentiated (n = 3). The median resection margin of the specimen was 0.5 cm (range, 0.1–2.5 cm). The duration of the hospital stay after IORFA ranged from 4 to 24 days (mean, 9.85 days). Of the 112 patients treated with IORFA, 10 (8.9%) had evidence of incompletely treatment, with residual viable tumor evident on the first imaging study 1 week postoperatively. The cause of incomplete IORFA was too large a size (n = 2), close proximity to major vessel (n = 3), bile duct (n = 1), severe adhesion (n = 1), and missed intraoperative diagnosis (n = 3). Immediate retreatments modalities were TAE (n = 4), CT-guided RFA (n = 2), P-RFA (n = 1), ethanol injection (n = 1), and no further treatment (n = 2). Tumor marker (alpha fetoprotein and Pivka: cutoff level of 20 ng/mL and 125 mAU/mL, respectively) were preoperatively elevated in 44 and 31 patients, respectively. After IORFA treatment, there was a reduction from preoperative levels in 74 (71.2%) and 82 patients (86.3%), respectively. Multivariate DFS analysis revealed Pivka reduction was more accurate than α-FP reduction as a clinically significant effect (B).
At a median follow-up of 32 months, HCC recurred in 78 patients (69.6%). Cumulative recurrence rate at 1 and 3 years was 44% and 73%, respectively (Fig. 1). The site of recurrence was local in 10 patients (8.9%), with local recurrence commonly developing in segment I (n = 4), previous TAE or P-RFA (n = 4) site. Local recurrence was treated with TAE (n = 6), P-RFA (n = 1), IORFA (n = 1), irradiation (n = 1), and chemotherapy (n = 1). The intrahepatic site in the liver in 68 patients (61%) showed dominant pattern of recurrence. Intrahepatic liver site with distant pulmonary metastasis occurred in 4 patients, pulmonary with bone metastasis occurred in 3 patients, brain metastasis occurred in 2 patients, and adrenal metastasis occurred in 1 patient. Tumor recurrence was treated with combined sessions of P-RFA (n = 24), TAE (n = 25), hepatic resection (n = 7), chemotherapy (n = 19), irradiation (n = 12), IORFA (n = 13), ethanol injection (n =3), and liver transplantation (n = 2). Chemotherapy regimens included Folfiri (irinotecan, fluorouracil, folinate; n = 2), hepatic artery floxuridine infusion; (n = 12), and FP (5-fluorouracil, cisplatin; n = 5).
Following 121 treatments, there were 52 complications (43%) according to Clavien-Dindo classification (Table 3).
Over grade III complications were observed in 27 patients (22.3%). There were 3 treatment-related deaths. One patient with variceal bleeding with asphyxia died 3 days after the operation. Two patients developed myocardial infarction with heart failure and died 2 and 15 days after the operation.
Bile duct rupture occurred in 2 patients, 1 of which had continued fatal biliary leakage; the patients died 9 and 12 months postoperatively. Readmission were required in 9 patients for ventral herniorrhaphy (n = 4), wound revision (n = 3), and diuretic therapy for scrotal edema (n = 2).
Cumulative DFS rate at 1 and 3 years was 54% and 24%, respectively (Fig. 2). In univariate analysis for DFS, Child-Pugh classification, previous treatment incidence, Pivka reduction, and portal vein thrombosis (PVT) statistically affected DFS. On multivariate analysis for DFS, age, previous treatment incidence, Pivka reduction and PVT showed a significant main effect (Table 4).
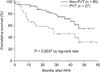
With regard to OS with a follow-up of at least 12 months, 37 patients died of disease and, 75 patients were still alive. Cause of death were cancer progression in 17 patients, variceal bleeding in 3 patients, PVT in 12 patients, multiple organ failure with sepsis in 3 patients, and heart failure in 2 patients. Cumulative OS rate at 1 and 3 years was 87% and 66%, respectively (Fig. 2). Child classification, previous treatment incidence, amount of ascites, operative time, PVT, and esophageal variceal bleeding (EVB) were factors for OS in univariate analysis. On multivariate OS analysis, age, segment I location of tumor, amount of ascites, and PVT were significant main effects (Table 5).
PVT developed in 27 patients at the main trunk (n = 21, 18.8%) and segmental branch (n = 6, 5.3%). Causes of PVT were tumor progression (n = 22), post-IORFA induced (n = 2), post-TAE induced (n = 1), and unknown (n = 2). Patients without PVT had a statistically significant longer OS, as compared to patients with PVT that associated tumor progression (P = 0.004). The hazard ratio [HR] for OS in PVT patients compared with that in non-PVT patients was 2.54 (P = 0.005: 95% confidence interval [CI], 1.32–4.89) (Fig. 3). Among ascites fluid culture in 23 patients, paracentesis cultures were positive for Enterococcus faecalis in 3 patients and for Actinetobacter Iwoffii in 1.
Whatever the initial therapy, most patients with HCC receive multimodality treatment that includes surgical resection, transarterial chemoembolization (TACE), percutaneous RFA, radiation therapy. chemotherapy, and ethanol injection, either in sequence or combination as dictated by an individual's disease progression. Surgical resection or local ablation can produce long-term DFS and OS in a subset of patients. However, it cannot overcome the tumor biology in patients who already have micrometastasis that express the inherent multicentric nature of HCC in cirrhosis [1011].
Not surprisingly, the most common site of recurrence in the present study was at a new site in the liver. Thus IORFA site local recurrence rate was only 9% and intrahepatic distant recurrence was noted in over 50% of the patients. The main cause of local recurrence was deeply seated (S1) location (n = 4) due to partial visibility, poor electrode path, risk of incomplete ablation and previous TAE or P-RFA site recurrence (n = 4). S1 patients had short-term overall survival compared to other patients (HR for OS, 9.54; P < 0.001; 95% CI, 2.74–33.16) although there was no significant difference in DFS between S1 and other patients.
Some clinicians feel that TACE is theoretically helpful in multinodular or infiltrative type of HCC. However, the arguments against the use of TACE are that it mainly involves well differentiated HCC and fails to completely kill poorly differentiated cells, with the residual HCC cells being more aggressive. Another counterargument is that incomplete tumor cell necrosis weakens adhesiveness within the tumor, facilitating the release of cancer cells from the primary focus into the distant bloodstream; also, employing TACE may complicate liver mobilization owing to the perihepatic adhesion [12].
RFA for HCC can be performed by a percutaneous approach (P-RFA) or an open approach (IORFA). When employing P-RFA, there is the possibility of severe complications at a risky location, such as HCC nodules adjacent to large vessel, bile duct or extrahepatic organ. Also, subcapsular locations are a risk factor for local recurrence after P-RFA. Moreover, recurrence is associated with lower accuracy, poor accessibility in certain areas of liver, and a lower complete ablation rate than IORFA [1314]. IORFA is no longer a minimally invasive procedure. Intraoperative ultrasonographic imaging performed directly on the surface of the hepatic capsule increases the diagnostic accuracy. Liver mobilization creates an injury-free space for larger vessels and adjacent organs, which can increase technical effectiveness. Laparotomy can enable the combination of surgical resection. Sometimes IORFA is necessary because of significant adhesions from previous TAE or P-RFA [15161718].
In our series, due to TACE-induced dense adhesions preoperative planned hepatic resection (n = 18) should have been changed to IORFA intraoperatively. The main limitations of the IORFA are its invasiveness ("trauma of access") with increased morbidity and longer recovery time and hospital stay. In our series, due to underlying liver cirrhosis with comorbidities, 9 patients were readmitted. The main causes of readmissions were ventral herniorrhaphy (n = 4), wound revision (n = 3), and ascites control combined with scrotal edema (n = 2).
To manage multifocal HCC, combined hepatectomy and IORFA is easier, if not better, than multiple anatomical resection. If a tumor is small but requires a large resection volume, IORFA is a safer option in terms of liver function preservation [1920]. IORFA may be a less traumatic approach in case of reoperation at a site with dense adhesion, as adhesiolysis for resection can lead to bleeding problems in patients with coagulopathy, thrombocytopenia, and underlying comorbidities [21]. In our study, almost all the patients had comorbidities, such as cirrhotic liver including thrombocytopenia, EVB, gastric ulcer, underlying heart problems (e.g., atrial fibrillation, myocardial infarction), accompanied malignancy (e.g., colorectal cancer, gastric cancer), metabolic disease (e.g., diabetes mellitus, hypertension) were main obstacles to treat HCC patients with liver cirrhosis [2223]. In our series, the main cause of mortality within 1 month were 2 cases of heart failure, and 1 case of variceal bleeding with asphyxia, which suggests the importance of preoperative control of comorbidities to treat the HCC patients with liver cirrhosis. Alpha-fetoprotein and Pivka are useful markers for DFS and OS, particularly in patients in whom the serum Pivka level does not return to normal after IORFA [24].
Hindrances include HCC nodules <1 cm, invisible or vague nodules, concomitant confusing or misleading nodular lesions around the tumor, and local tumor progression of previously TAE or ablated lesions. All these circumstances can hinder lesion targeting. Sonazoid contrast agent is particularly useful in detecting nodules that lack Kuffer cells. The detectability of tumor nodules was reported as 83.5% in conventional ultrasonography and 93.2% in Sonazoid enhanced ultrasonography [2526]. In our institution, which adopted use of Sonazoid beginning in 2013, the incidence of incomplete treatment and local recurrences was markedly reduced. As a general complication of IORFA, infections are frequently encountered in the presence of diabetes and biliary leakage. Diabetes patients are at greater risk for infection owing to their less robust immune system [27]. In our study, focal dilatation of the bile duct in 2 patients was noted on follow-up CT with no clinical significance. IORFA may not produce efficient sealing of biliary radicale, and postoperative detachment of necrotic bile duct stumps, which occurred in 2 of our patients, causes continuous bile leakage, biloma, and delayed fatal complications 9 to 12 months after IORFA [2829]. A high risk for bleeding has been reported in patients with cirrhosis, given the high percentage of clinical or subclinical coagulation disorders with end stage liver disease. In our series, 2 partial portal vein thromboses were noted on follow-up CT with no clinical significance. Tumor seeding has been reported, particularly in superficially located, poorly differentiated HCC. Follow-up CT is always performed within a week following IORFA; the incomplete treatment rate in our series (8.3%) was higher than other reports [15]. The main cause of incomplete IORFA was large (>3 cm) size of the HCC nodules (n = 2), vague ultrasonic diagnosis (n = 4), and risk of adjacent organ injury (n = 4).
During the study period, the protocol was changed in an effort to reduce the incidence of incomplete treatment and local recurrences. Regarding the tumor size and number, HCC nodules should be within the Milan criteria (3 or fewer nodules ≤3 cm in diameter); secondly, invisible or vague nodules should be eliminated around the previously ablated portion, for which, Sonazoid enhanced ultrasonography was adopted; thirdly, as an initial therapy for HCC nodules, IORFA replaced TACE due to the lower rate of complete tumor remission and post-TACE adhesion.
This study had some limitations. The decision to perform IORFA was made by physician choice on a case-by-case basis, and was not standardized. This might be an inevitable limitation of a retrospective study. Further studies will also be needed to evaluate the impact of IORFA in patient's quality of life. In addition, the high propensity for regional and systematic HCC recurrence in a significant number of patients emphasizes the need for effective multimodality approaches.
In conclusion, IORFA alone or in combination with surgical resection extends the spectrum of liver surgery. A fundamental understanding of RF ablation, additional comorbidities, and post ablation complication are necessary to maximize the safety and efficacy of IORFA for treating HCC with cirrhosis.
Figures and Tables
 | Fig. 1The cumulative rates for local tumor progression (A), intrahepatic distant recurrence (B) of the 112 patients who underwent intraoperative radiofrequency ablation. RFA, radiofrequency ablation. |
 | Fig. 2The cumulative rates for disease-free survival (A) overall survival (B) of the 112 patients who underwent intraoperative radiofrequency ablation. RFA, radiofrequency ablation. |
 | Fig. 3Patients without portal vein thrombosis (PVT) had a statistically significant longer overall survival compared to patients with PVT (P = 0.004). RFA, radiofrequency ablation. |
Table 1
Patients' baseline characteristics (n = 112)

Values are presented as mean ± standard deviation (range) or number (%).
HCC, hepatocellular carcinomas; HB, hepatitis B; HC, hepatitis C; PBC, primary biliary cirrhosis; ASA, American Society of Anesthesiologists; IORFA, intraoperative radiofrequency ablation; PVT, portal vein thrombosis; EVB, esophageal variceal bleeding.
Table 3
Postoperative complications and deaths according to Clavien-Dindo classification in 121 treatments

References
1. Raut CP, Izzo F, Marra P, Ellis LM, Vauthey JN, Cremona F, et al. Significant long-term survival after radiofrequency ablation of unresectable hepatocellular carcinoma in patients with cirrhosis. Ann Surg Oncol. 2005; 12:616–628.
2. El-Gendi A, El-Shafei M, Abdel-Aziz F, Bedewy E. Intraoperative ablation for small HCC not amenable for percutaneous radiofrequency ablation in Child A cirrhotic patients. J Gastrointest Surg. 2013; 17:712–718.
3. Nishikawa H, Inuzuka T, Takeda H, Nakajima J, Matsuda F, Sakamoto A, et al. Comparison of percutaneous radiofrequency thermal ablation and surgical resection for small hepatocellular carcinoma in patients with cirrhosis. BMC Gastroenterology. 2011; 11:143.
4. Ribeiro MA Jr, Rodrigues JJ, Habr-Gama A, Chaib E, D'Ipolitto G, Fonseca AZ, et al. Radiofrequency ablation of primary and metastatic liver tumors: 4 years experience. Hepatogastroenterology. 2007; 54:1170–1175.
5. Kim YS, Rhim H, Lim HK, Choi D, Lee WJ, Jeon TY, et al. Intraoperative radiofrequency ablation for hepatocellular carcinoma: long-term results in a large series. Ann Surg Oncol. 2008; 15:1862–1870.
6. Elias D, Goharin A, El Otmany A, Taieb J, Duvillard P, Lasser P, et al. Usefulness of intraoperative radiofrequency thermoablation of liver tumours associated or not with hepatectomy. Eur J Surg Oncol. 2000; 26:763–769.
7. Cheung TT, Ng KK, Chok KS, Chan SC, Poon RT, Lo CM, et al. Combined resection and radiofrequency ablation for multifocal hepatocellular carcinoma: prognosis and outcomes. World J Gastroenterol. 2010; 16:3056–3062.
8. Eisele RM, Zhukowa J, Chopra S, Schmidt SC, Neumann U, Pratschke J, et al. Results of liver resection in combination with radiofrequency ablation for hepatic malignancies. Eur J Surg Oncol. 2010; 36:269–274.
9. Choi D, Lim HK, Joh JW, Kim SJ, Kim MJ, Rhim H, et al. Combined hepatectomy and radiofrequency ablation for multifocal hepatocellular carcinomas: long-term follow-up results and prognostic factors. Ann Surg Oncol. 2007; 14:3510–3518.
10. Pawlik TM, Izzo F, Cohen DS, Morris JS, Curley SA. Combined resection and radiofrequency ablation for advanced hepatic malignancies: results in 172 patients. Ann Surg Oncol. 2003; 10:1059–1069.
11. Lencioni R, Cioni D, Crocetti L, Franchini C, Pina CD, Lera J, et al. Early-stage hepatocellular carcinoma in patients with cirrhosis: long-term results of percutaneous image-guided radiofrequency ablation. Radiology. 2005; 234:961–967.
12. Gao ZH, Bai DS, Jiang GQ, Jin SJ. Review of preoperative transarterial chemoembolization for resectable hepatocellular carcinoma. World J Hepatol. 2015; 7:40–43.
13. Khan MR, Poon RT, Ng KK, Chan AC, Yuen J, Tung H, et al. Comparison of percutaneous and surgical approaches for radiofrequency ablation of small and medium hepatocellular carcinoma. Arch Surg. 2007; 142:1136–1143.
14. Machi J, Uchida S, Sumida K, Limm WM, Hundahl SA, Oishi AJ, et al. Ultrasound-guided radiofrequency thermal ablation of liver tumors: percutaneous, laparoscopic, and open surgical approaches. J Gastrointest Surg. 2001; 5:477–489.
15. Lee SD, Han HS, Cho JY, Yoon YS, Hwang DW, Jung K, et al. Safety and efficacy of laparoscopic radiofrequency ablation for hepatic malignancies. J Korean Surg Soc. 2012; 83:36–42.
16. Sakoda M, Ueno S, Iino S, Minami K, Ando K, Kawasaki Y, et al. Endoscopic versus open radiofrequency ablation for treatment of small hepatocellular carcinoma. World J Surg. 2013; 37:597–601.
17. Livraghi T, Meloni F, Di Stasi M, Rolle E, Solbiati L, Tinelli C, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: is resection still the treatment of choice? Hepatology. 2008; 47:82–89.
18. Shen SQ, Xiang JJ, Xiong CL, Wu SM, Zhu SS. Intraoperative radiofrequency thermal ablation combined with portal vein infusion chemotherapy and transarterial chemoembolization for unresectable HCC. Hepatogastroenterology. 2005; 52:1403–1407.
19. Minami Y, Kawasaki T, Kudo M, Haji S, Shiraishi O, Kawabe T, et al. Treatment of large and/or multiple hepatic malignancies: open surgical approaches of radiofrequency ablation. Hepatogastroenterology. 2007; 54:2358–2360.
20. Ueno S, Sakoda M, Kubo F, Hiwatashi K, Tateno T, Baba Y, et al. Surgical resection versus radiofrequency ablation for small hepatocellular carcinomas within the Milan criteria. J Hepatobiliary Pancreat Surg. 2009; 16:359–366.
21. Tateishi R, Shiina S, Teratani T, Obi S, Sato S, Koike Y, et al. Percutaneous radiofrequency ablation for hepatocellular carcinoma. An analysis of 1000 cases. Cancer. 2005; 103:1201–1209.
22. Tepel J, Hinz S, Klomp HJ, Kapischke M, Kremer B. Intraoperative radiofrequency ablation (RFA) for irresectable liver malignancies. Eur J Surg Oncol. 2004; 30:551–555.
23. de Baere T, Risse O, Kuoch V, Dromain C, Sengel C, Smayra T, et al. Adverse events during radiofrequency treatment of 582 hepatic tumors. AJR Am J Roentgenol. 2003; 181:695–700.
24. Curley SA, Izzo F, Ellis LM, Nicolas Vauthey J, Vallone P. Radiofrequency ablation of hepatocellular cancer in 110 patients with cirrhosis. Ann Surg. 2000; 232:381–391.
25. Masuzaki R, Shiina S, Tateishi R, Yoshida H, Goto E, Sugioka Y, et al. Utility of contrast-enhanced ultrasonography with Sonazoid in radiofrequency ablation for hepatocellular carcinoma. J Gastroenterol Hepatol. 2011; 26:759–764.
26. Ikeda K, Osaki Y, Nakanishi H, Nasu A, Kawamura Y, Jyoko K, et al. Recent progress in radiofrequency ablation therapy for hepatocellular carcinoma. Oncology. 2014; 87:Suppl 1. 73–77.
27. Rhim H, Dodd GD 3rd, Chintapalli KN, Wood BJ, Dupuy DE, Hvizda JL, et al. Radiofrequency thermal ablation of abdominal tumors: lessons learned from complications. Radiographics. 2004; 24:41–52.
28. Xiao WK, Chen D, Hu AB, Peng BG, Guo YZ, Fu SJ, et al. Radiofrequency-assisted versus clamp-crush liver resection: a systematic review and meta-analysis. J Surg Res. 2014; 187:471–483.
29. Kim HO, Kim SK, Son BH, Yoo CH, Hong HP, Cho YK, et al. Intraoperative radiofrequency ablation with or without tumorectomy for hepatocellular carcinoma in locations difficult for a percutaneous approach. Hepatobiliary Pancreat Dis Int. 2009; 8:591–596.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download