Abstract
Purpose
There is still some debate on surgical procedures for hepatocellular carcinoma (HCC) patients with bile duct tumor thrombi (BDTT, Ueda type 3 or 4). What is adequate extent of liver resection for curative treatment? Is extrahepatic bile duct resection mandatory for cure? The aim of this study is to answer these questions.
Methods
Between February 1994 and December 2012, 877 consecutive HCC patients underwent hepatic resection at Ajou University Hospital. Thirty HCC patients (3.4%) with BDTT (Ueda type 3 or 4) were retrospective reviewed in this study.
Results
In total, 20 patients enrolled in this study were divided into 2 groups: patients who underwent hemihepatectomy with extrahepatic bile duct resection (group 1, n = 10) and with only removal of BDTT (group 2, n = 10). The 1-, 3- and 5-year overall survival rates were 75.0%, 50.0%, and 27.8%, respectively. The 1-, 3-, and 5-year survival rates of group 1 were 100.0%, 80.0%, and 45.7%, and those of group 2 were 50.0%, 20.0%, and 10.0%, respectively (P = 0.014). The 1-, 3-, and 5-year recurrences free survival rates of group 1 were 90.0%, 70.0%, and 42.0%, and those of group 2 were 36.0%, 36.0%, and 0%, respectively (P = 0.014). Thrombectomy and infiltrative growth type (Ig) were found as independent prognostic factors for recurrence free survival by multivariate analysis. Thrombectomy, Ig, and high indocyanine green retention rate at 15 minutes were found as independent prognostic factors for overall survival by multivariate analysis.
Jaundice is present in 19% to 40% of patients with hepatocellular carcinoma (HCC). Among the common causes is decompensation of underlying liver cirrhosis or extensive destruction of liver parenchyma by tumor. However, bile duct tumor invasion or bile duct tumor thrombi (BDTT), hemobilia and compression of bile duct by tumor may also cause jaundice. Lin [1] classified such cases of HCC as "icteric hepatocellular carcinoma". Icteric HCC has been rarely reported in the past. In 1947, Clark and Schulz [2] first reported 12 cases of icteric HCC caused by tumor invasion to extrahepatic bile duct. Edmondson [3] encountered common bile duct (CBD) tumor thrombus causing icteric HCC in 1950. In 1956, a case reported by Creed and Fisher [4] described an HCC patient presenting jaundice and right upper quadrant abdominal discomfort.
In 1975, Lin [1] reported eight cases of icteric HCC among 408 HCC patients, and in 1979, Tsuzuki et al. [5] reported the successful resection of 20 icteric HCCs. According to Lau et al. [6] in 1990, the icteric type HCC manifests in 3%, and Ueda et al. [7] reported only 1.66% of HCC patients had jaundice. The mean survival after diagnosis of icteric HCC is shorter compared with conventional HCC, as reports by Kojiro et al. [8] and Lau et al. [6]; 16 and 35 days. This is owing to the lower diagnostic rate. For patients presenting to hospital with jaundice, the differential diagnosis from bile duct cancer, bile duct stone, and hepatic hilar cancer is not easy. Recently, even MRI in diagnosing of HCC with BDTT has improved preoperative accuracy on HCC diagnosis [9]. However, the resection rate is markedly low, because, in many cases, the tumor presents near liver hilum, and especially at caudate lobe [510]. There is no consensus as to the treatment of the icteric HCC.
In 1999, we reported that the most appropriate curative treatment for icteric HCC is hemihepatectomy with caudate lobectomy and extrahepatic bile duct resection (BDR). However, if the HCC extends to the vessels and to the contralateral lobe, or if liver function is very poor, external drainage of bile duct or biliary stent insertion followed by hepatic artery embolization is preferred to limited hepatectomy or removal of BDTT through choledochotomy [11]. In this article, however, we would like to discuss the adequate extent of liver resection in curative resection of icteric HCC. Three questions are still under debate: Is hemihepatectomy mandatory? Is extrahepatic BDR mandatory? Should liver transplantation be considered if primary tumor meets Milan criteria? Through our experience and review of the literature, we would like to answer to these questions.
Between February 1994 and December 2012, 877 HCC patients underwent hepatic resection in Ajou University Hospital; their clinical data were prospectively collected. In this study, we focus on icteric HCC (B3 or B4). According to Ueda et al. [7], the most common cause of icteric HCC is BDTT. They classified icteric HCC into 4 types; type 1: BDTT located in the secondary branch of the bile duct tree; type 2: BDTT extended to the first branch of the bile duct tree; type 3a: BDTT extended to the common hepatic duct; type 3b: an implanted tumor growing in the CBD, type 4: floating tumor debris from the ruptured tumor in CBD (Fig. 1). In total, 30 cases with gross BDTT (B3 or B4) were retrospectively reviewed. Ten out of 30 patients were excluded in this study for the following reasons: HCC invasion in major portal vein and/or hepatic vein (n = 8; 6 cases with Vp3, 1 case with Vp4, and 1 case with Vv3), combined HCC and CCC (n = 2). Finally, 20 patients who received ipsilateral hemihepatectomy with radical treatment intention were enrolled in this study. They were divided into 2 groups: patients who underwent ipsilateral hemihepatectomy with extrahepatic BDR (group 1, n = 10) and ipsilateral hemihepatectomy with removal of BDTT by throbectomy (group 2: n = 10). These patients were followed up until September 2015 or patient death.
Any statistical difference among the groups was analyzed with the unpaired t-test or chi-square test. Overall survivals were calculated using the Kaplan-Meier method. Univariate and multivariate analysis for the risk factor of recurrencefree survival and overall survival were performed with Cox regression. Statistical significance was defined as P < 0.05. SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
The clinical and pathology data of the 20 patients underwent ipsilateral hemihepatectomy who were divided into extrahepatic BDR (group 1) and thrombectomy (group 2) are showed in Table 1. Even though the infiltrative growth type (Igs) were found more frequently in thrombectomy group (6 in 10), the results did not reach statistical significance (P = 0.170). And there were no differences between the 2 groups for all the other variables in Table 1.
In this study, the median survival time was 39 months (range, 2–233 months). The 1-, 3- and 5-year overall survival rates were 75.0%, 50.0%, and 27.8%, respectively (Fig. 2). The 1-, 3-, and 5-year survival rates of group 1 were 100%, 80%, and 45.7%, and those of group 2 were 50%, 20%, and 10%, respectively (P = 0.014) (Fig. 3A). The 1-, 3-, and 5-year recurrence-free survival rates of group 1 were 90.0%, 70.0%, and 42.0%, and those of group 2 were 36.0%, 36.0%, and 0%, respectively (P = 0.023) (Fig. 3B).
There were 15 patients who experienced recurrence during the follow-up period, 7 cases in extrahepatic BDR group and 8 cases in thrombectomy group (Fig. 4). In thrombectomy group, 6 of 8 cases had recurrence within 12 months. However, 6 in 7 cases had recurrence beyond 12 months in extrahepatic BDR group. The frequency of postoperative recurrence in the remnant bile duct was: 30% (3 of 10) after hemihepatectomy with thrombectomy, and 0% (0 of 10) after hemihepatectomy with extrahepatic BDR. The most important cause of recurrence is thought to be the microscopic skipped invasion of BDTT into the bile duct wall. The key factor of a skipped invasion seems to be tightness of contact between bile duct wall and BDTT. Shiomi et al. [12] reported that the BDTT invaded the bile duct wall microscopically in 1 of the 5 patients (20%) who underwent BDR and reconstruction.
One case of skipped metastasis is shown in Fig. 5A, B. After removal of BDTT, there were some fibrous tissues with minute oozing without any residual tumor thrombi in the bile duct. Series of wedge biopsies of bile duct wall was done. Fig. 5C shows the results of histological examination of bile duct wall including fibrous tissues. There were the microscopic residual tumor thrombi (left), and we can see clear cell nest in the HCC foci (right).
As shown in Fig. 4, the recurrence pattern was significantly different between the 2 groups. And the median recurrence time for thrombectomy group was significantly shorter than extrahepatic BDR group (4.5 months vs. 47 months, P = 0.042). Table 2 show that the outcomes of univariate and multivariate analysis for recurrence-free survival and overall survival by cox regression. Ig (hazard ratio [HR], 8.512; range, 1.509–62.720; P = 0.044), ipsilateral hemihepatectomy with thrombectomy (HR, 5.669; range, 1.190–27.015; P = 0.029) were found as independent prognostic factors for recurrence free survival by multivariate analysis. Ig (HR, 6.106; range, 1.116–33.390; P = 0.037), ipsilateral hemihepatectomy with thrombectomy (HR, 7.308; range, 1.901–28.093; P = 0.004) and high indocyanine green retention rate at 15 minutes (ICG R15) (HR, 8.983; range, 1.461–55.243; P = 0.018) were found as independent prognostic factors for overall survival by multivariate analysis.
In this study, we have 4 long-term survivors after hemihepatectomy with extrahepatic BDR for icteric HCC (Table 3). The survival period ranged from 108 to 173 months after surgery and the recurrence free survival time ranged from 47 to 173. They had 4 common characteristics; Firstly, young patients with relatively early stage of primary tumor and preserved good liver function. Secondly, their preoperative AFP values were, somewhat, lower. Thirdly, all of the four patients were performed on with hemihepatectomy with caudate lobectomy and extrahepatic BDR, and lastly, the tumor growth pattern of the 4 cases was expanding gross type.
The first technical problem as to whether minor hepatectomy is feasible in the treatment of icteric HCCs is still under debate. There may be 2 different options; "to perform major or minor hepatectomy according to liver function" versus "to perform hemihepatectomy as a minimum-required surgery according to liver function". We believe we should perform hemihepatectomy as a minimum-required surgery according to liver function because of our early negative experience (3 patients who underwent minor hepatic resection with only removal of BDTT suffered from recurrence in the intrahepatic bile duct). The pathologic base may be skipped metastasis. That means the Ig tumor thrombi was infiltrative invasion of the bile duct. If the liver function is very limited, other nonsurgical modalities must be considered, instead. Huang et al. [13] reported that palliative treatment strategies for patients with poor liver function, including transarterial chemoembolization (TACE) and/or radiation therapy showed a beneficial effect in improving the survival time, the median survival time was 13.4 months.
The second concern is whether to remove the BDTT through a choledochotomy during surgical resection or to perform hemihepatectomy with caudate lobectomy and extrahepatic BDR. The authors [121415] who favor the previous viewpoint reported that there were no significant differences between the 2 groups in 5-year survival rates. Therefore, they concluded that it is not necessary to perform extrahepatic BDR. On the other hand, some authors [1116] reported contrary results that performing hemihepatectomy with caudate lobectomy and extrahepatic BDR could significantly increase the 5-year survival rates.
Of 4,308 HCC patients surgically treated at 4 Korean institutions, this single-arm retrospective study included 73 patients (1.7%) who underwent resection for HCC with BDTT. According to Ueda classification, BDTT was type 2 in 34 cases (46.6%) and type 3 in 39 cases (53.4%). Systematic hepatectomy was performed in 69 patients (94.5%), and concurrent BDR was performed in 31 patients (42.5%). Surgical curability types were R0 (n = 57, 78.1%), R1 (n = 11, 15.1%), and R2 (n = 5, 6.8%). Patient survival rates were 76.5% at 1 year, 41.4% at 3 years, 32.0% at 5 years, and 17.0% at 10 years. Recurrence rates were 42.9% at 1 year, 70.6% at 3 years, 77.3% at 5 years, and 81.1% at 10 years. Results of univariate survival analysis showed that maximal tumor size, BDR, and surgical curability were significant risk factors for survival, and surgical curability was a significant risk factor for recurrence. Multivariate analysis did not reveal any independent risk factors. HCC patients with BDTT achieved relatively favorable long-term results after resection; therefore, this study proposes that extensive surgery should be recommended when complete resection is anticipated. In this study, there is a problem; gross portal vein invasion in 24 patients (32.9%). We believe further study is required for icteric HCC patients without gross portal invasion because gross portal vein invasion is so strong a prognostic factor in HCC [17].
In the present study, we excluded 6 cases of gross portal vein invasion and 2 cases of gross hepatic vein invasion. The patients in group 1 who received extensive surgery by ipsilateral hemihepatectomy with caudate lobectomy and extrahepatic BDR have a significantly longer recurrence-free survival time. This extensive surgery procedure can achieve a R0 resection that the recurrence-free survival rate was higher, its 1-, 3-, and 5-year recurrence-free survival rate was 90.0%, 70.0%, and 42.0%, respectively. Additionally, the recurrent sites were not located at the bile duct in all the 7 recurrent cases—3 at liver, 2 at lung, 1 at bone, and 1 at abdominal lymph node. The patients with tumor recurrence at the liver were easily received subsequent treatment, such as TACE, reresection and/or transplantation. Finally, their 1-, 3-, and 5-year survival rate was 100%, 80%, and 45.7%, respectively. On the contrary, there were 8 cases that experienced recurrence in the group 2, 3 cases recurrence at bile duct, and 5 at the liver. Unfortunately, the 3 cases of recurrence at bile duct died within 6 months due to liver failure caused by obstruction on the bile duct and invasive tumor growth after operation. And the 1-, 3-, and 5-year survival rate of group 2 was 36.0%, 36.0%, and 0%, respectively. Our multivariate analysis demonstrated that removal of BDTT by thrombectomy and Ig were independent risk factors for tumor recurrence. And the combined high ICG R15 (more than 20%) was independent risk factors for overall survival.
The last technical debate is "Should icteric HCC be an indication for liver transplantation?" It is still under debate, because, so far, there have only been 3 reports within a total 19 cases [151718]. One report states that 4 patients (80%) died of HCC recurrence within 3 years [17]. Other reports have the same conclusion on the high risk of HCC recurrence posttransplantation [18]. Therefore, liver transplantation for HCC patients with BDTT still carries a high risk of HCC recurrence, thus requiring further study. How do we perform bile duct reconstruction after liver transplantation for icteric HCC? Duct-to-duct anastomosis versus hepaticojejunostomy. This is also a question as to whether to perform extrahepatic BDR or not. Peng et al. [15] asserted extrahepatic BDR should be followed by hepaticojejunostomy. On the contrary, Lee et al. [19] reported the following; after the extent of BDTT was manually evaluated, they performed a bile duct dissection, stapling the distal portion of BDTT with stapler. They examined the resection margin of the bile duct for malignant cells and reconstructed the bile duct with hepaticojejunostomy in case of insufficient length for duct-to-duct anastomosis. It is also debatable, however, due to the theory that tumor skipped metastasis of hepaticojejunostomy after extrahepatic BDR may be a more rational approach. Therefore, whether it's liver transplantation or ipsilateral hemihepatectomy with caudate lobectomy, extrahepatic BDR should be performed for icteric HCC patients.
In conclusion, the incidence of icteric HCC is very rare, and its prognosis is poor. Although surgical resection is the only option for curative treatment, there is still much debate on the technical aspects of surgical treatment of icteric HCC.
In most cases of icteric HCC, hepatectomy is performed in selected groups of patients because of liver cirrhosis. However, it also tends to recur within the bile duct, putting the surgeons in dilemma, whether to initially resect the extended portion of the liver including extrahepatic bile duct or not. If liver function is fair, it is wise to perform en bloc hepatectomy and affected biliary tree. In cases of poor liver function, however, external drainage of bile duct and biliary stent insertion followed by hepatic artery embolization is preferred to surgical resection.
The limitations of the present study are small case numbers, and no liver transplantation cases. In the future, international multicenter collaboration research on this subject may play an important role in forming global consensus.
Figures and Tables
Fig. 1
Ueda classification of hepatocellular carcinoma with bile duct tumor thrombi classified according to thrombus location [7].

Fig. 2
Actuarial survival curve after hemihepatectomy for hepatocellular carcinoma with grossly bile duct invasion (n = 20).
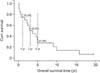
Fig. 3
(A) Actuarial survival curves of hemihepatectomy with thrombectomy group (light line) and hemihepatectomy with extrahepatic bile duct (BD) resection (deep line) (P = 0.014). (B) Actuarial recurrence free survival curves of hemihepatectomy with thrombectomy group (light line) and hemihepatectomy with extrahepatic BD resection (deep line) (P = 0.023).

Fig. 5
(A) One bile duct tumor thrombi (BDTT) case with a skipped bile duct (BD) invasion. Some fine fibrous tissues with minute oozing without any residual tumor thrombi. (B) One BDTT case with a skipped BD invasion. Some fine fibrous tissues with minute oozing without any residual tumor thrombi. (C) Histologic examination of the fibrous bridge structure. A focus of skipped tumor invasion (left: H&E, ×100; right: H&E, ×400). BDE, bile duct epithelium.

References
1. Lin TY. Tumor of the liver. In : Bockus HL, editor. Gastroenterology. Philadelphia: WB Saunders;1976. p. 522–533.
2. Clark W, Schulz MD. Hepatoma, with invasion of cystic duct and metastasis to third lumbar vertebra. N Engl J Med. 1947; 237:673–676.
3. Edmondson HA. Tumors of the liver and intrahepatic bile ducts. Washington: Armed Forces Institute of Pathology;1958.
4. Creed DL, Fisher ER. Clot formation in the common duct; an unusual manifestation of primary hepatic carcinoma. AMA Arch Surg. 1956; 73:261–265.
5. Tsuzuki T, Ogata Y, Iida S, Kasajima M, Takahashi S. Hepatoma with obstructive jaundice due to the migration of a tumor mass in the biliary tract: report of a successful resection. Surgery. 1979; 85:593–598.
6. Lau WY, Leung JW, Li AK. Management of hepatocellular carcinoma presenting as obstructive jaundice. Am J Surg. 1990; 160:280–282.
7. Ueda M, Takeuchi T, Takayasu T, Takahashi K, Okamoto S, Tanaka A, et al. Classification and surgical treatment of hepatocellular carcinoma (HCC) with bile duct thrombi. Hepatogastroenterology. 1994; 41:349–354.
8. Kojiro M, Kawabata K, Kawano Y, Shirai F, Takemoto N, Nakashima T. Hepatocellular carcinoma presenting as intrabile duct tumor growth: a clinicopathologic study of 24 cases. Cancer. 1982; 49:2144–2147.
9. Liu Q, Chen J, Li H, Liang B, Zhang L, Hu T. Hepatocellular carcinoma with bile duct tumor thrombi: correlation of magnetic resonance imaging features to histopathologic manifestations. Eur J Radiol. 2010; 76:103–109.
10. Taguchi H, Ogino T, Miyata A, Munehisa T. Bile duct invasion of hepatocellular carcinoma. Nihon Shokakibyo Gakkai Zasshi. 1983; 80:2259–2268.
11. Wang HJ, Kim JH, Kim JH, Kim WH, Kim MW. Hepatocellular carcinoma with tumor thrombi in the bile duct. Hepatogastroenterology. 1999; 46:2495–2499.
12. Shiomi M, Kamiya J, Nagino M, Uesaka K, Sano T, Hayakawa N, et al. Hepatocellular carcinoma with biliary tumor thrombi: aggressive operative approach after appropriate preoperative management. Surgery. 2001; 129:692–698.
13. Huang JF, Wang LY, Lin ZY, Chen SC, Hsieh MY, Chuang WL, et al. Incidence and clinical outcome of icteric type hepatocellular carcinoma. J Gastroenterol Hepatol. 2002; 17:190–195.
14. Satoh S, Ikai I, Honda G, Okabe H, Takeyama O, Yamamoto Y, et al. Clinicopathologic evaluation of hepatocellular carcinoma with bile duct thrombi. Surgery. 2000; 128:779–783.
15. Peng SY, Wang JW, Liu YB, Cai XJ, Deng GL, Xu B, et al. Surgical intervention for obstructive jaundice due to biliary tumor thrombus in hepatocellular carcinoma. World J Surg. 2004; 28:43–46.
16. Mok KT, Chang HT, Liu SI, Jou NW, Tsai CC, Wang BW. Surgical treatment of hepatocellular carcinoma with biliary tumor thrombi. Int Surg. 1996; 81:284–288.
17. Moon DB, Hwang S, Wang HJ, Yun SS, Kim KS, Lee YJ, et al. Surgical outcomes of hepatocellular carcinoma with bile duct tumor thrombus: a Korean multicenter study. World J Surg. 2013; 37:443–451.
18. Ha TY, Hwang S, Moon DB, Ahn CS, Kim KH, Song GW, et al. Long-term survival analysis of liver transplantation for hepatocellular carcinoma with bile duct tumor thrombus. Transplant Proc. 2014; 46:774–777.
19. Lee KW, Park JW, Park JB, Kim SJ, Choi SH, Heo JS, et al. Liver transplantation for hepatocellular carcinoma with bile duct thrombi. Transplant Proc. 2006; 38:2093–2094.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download