Abstract
Purpose
Preoperative neutrophil-to-lymphocyte ratio (NLR) reflects patients' inflammation status, clinical stage, and survival in various malignancies. However, only a limited amount of information on the clinical importance and prognostic significance of NLR in gastric cancer has been reported. The objective of this study is to assess the prognostic values of preoperative NLR in patients with gastric cancer.
Methods
During the period between August 1, 2005 and December 31, 2011, we collected data from 601 patients among those who had undergone surgery for gastric cancer at the Department of Surgery, Konkuk University Medical Center. We classified the subjects into high NLR (NLR ≥ 1.7) group and low NLR (NLR < 1.7) group.
Results
The gender, age, and American Society of Anesthesiologists (ASA) score did not differ in the two NLR groups. The pathologic features (tumor size, histology, number of examined lymph node, T stage, N stage, and TNM stage) did not differ either, except for tumor location (P = 0.006). Multivariate analysis identified TNM stage, NLR, and age as significant prognostic factors. Gender, tumor size, location, and histology did not show their prognostic significance when we applied the Cox proportional hazard model.
Gastric cancer is the second most common malignancy and the third leading cause of cancer death in Korea [1]. Although preoperative staging is helpful in selecting the most appropriate therapeutic strategy for patients with gastric cancer, it is difficult to predict their prognosis based solely on clinical staging. It is now widely accepted that both oncological characteristics and host response factors can affect variations within disease progression and clinical outcome in patients with colorectal cancer [2]. For instance, the immune status of the host can affect the prevalence of different types of cancer and outcome of cancer patients [3]. Moreover, recent studies have revealed a possible association between the presence of a systemic inflammatory response and a poor prognosis in cancer patients [45].
Meanwhile, some have attempted to determine the prognostic value of various markers of systemic inflammatory responses in certain groups of cancer patients, including cytokines such as intercellular adhesion molecule 1 and a neutrophil-to-lymphocyte ratio (NLR) [6]. An NLR can be calculated easily from a differential white blood cell count, and it can be used to evaluate cell-mediated immune responses [7]. In addition, preoperative NLRs reflect patients' inflammation status, their clinical stage, and their survival rates for liver, lung and colon cancer [8910]. In gastric cancer, a few studies with relatively small number of cases on the clinical importance and prognostic significance of NLRs have been reported to date. These studies argue that a high preoperative NLR might be a useful biomarker for identifying patients who have a poor prognosis after resection of primary gastric cancer. These studies calculated the cutoff value of NLR using median, 75 percentile value, or comparing P-value in Kaplan-Meier curve [11121314].
The aim of this study is to find the cutoff value of NLR, and to assess clinicopathological features and prognostic values of preoperative NLRs in patients with gastric cancer.
During the period between August 1, 2005 and December 31, 2011, we collected data from 601 patients among those who had undergone surgery for gastric cancer at the Department of Surgery, Konkuk University Medical Center, and also who met the following inclusion criteria: the presence of primary gastric cancer; no preoperative chemotherapy; no distant metastasis; R0 resection (no residual macroscopic or microscopic tumor); and more than 15 examined lymph nodes (LNs). Clinical information and follow-up data were obtained from the hospital's electronic records. The obtained clinicopathological data include patient demographics (age and sex), preoperative NLRs, pathologic characteristics (size, location, histology, TNM stage according to the seventh American Joint Committee on Cancer TNM classification, and the number of examined LNs), and follow-up data (follow-up duration and survival status).
Peripheral blood samples were gathered within two weeks during the preoperative period. The number of white blood cells and the percentage of particular types of cells were determined by using a hemocytometer, and the NLR was defined as the absolute neutrophil count divided by the absolute lymphocyte count.
We used a receiver-operating characteristic (ROC) curve to determine an appropriate cutoff value of the NLR. The area under curve was 0.635. We selected the 1.7 as cutoff value, at this point the sensitivity and specificity were 0.66 and 0.54, and the positive predictive value and negative predictive value was 0.18 and 0.91 (Fig. 1). Thus we classified the subjects into high NLR (NLR ≥ 1.7) group and low NLR (NLR < 1.7) group.
The location of tumor was categorized into three groups according to the operation records: upper third, middle third, and lower third. The histologic subtype was categorized as differentiated types (papillary adenocarcinoma, well differentiated tubular adenocarcinoma, and moderately differentiated tubular adenocarcinoma) and undifferentiated types (poorly differentiated tubular adenocarcinoma, signet ring cell carcinoma, and mucinous adenocarcinoma). Lastly, the follow-up duration was estimated from the date of surgery to the last follow-up date.
An independent t-test, chi-square test, and Fisher exact test were performed to evaluate the clinicopathological characteristics between the high NLR group and low NLR group. The cumulative survival rates were compared using the Kaplan-Meier method and the log-rank test. Furthermore, the Cox proportional hazards model for multivariate analysis was applied to establish the independent prognostic factors. Data were analyzed by using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA) and P-values less than 0.050 were considered as statistically significant.
The patient demographics and clinicopathologic characteristics of the two NLR groups are summarized in Table 1. The gender, age, and American Society of Anesthesiologists score did not vary across the two groups. Moreover, the pathologic features (tumor size, histology, number of examined LN, T stage, N stage, and TNM stage) did not differ either, except for tumor location (P = 0.006). A median follow-up was 49.0 months (range, 2.4-104.4 months).
Fig. 2 presents the Kaplan-Meier curves with log-rank test of overall survival by gender, age, tumor location, histology, TNM stage, and NLR. Significant differences in survival were demonstrated by these variables.
Furthermore, multivariate analysis identified advanced TNM stage, high preoperative NLR (NLR ≥ 1.7), and old age (≥70 years) as significant prognostic factors (Table 2). Gender, tumor size, location, and histology did not show their prognostic significance when we applied the Cox proportional hazard model with forward stepwise selection procedures.
A few studies have claimed that high preoperative NLRs in patients with different types of carcinoma are associated with a poor prognosis [891011121314]. Likewise, our study also confirmed that the prognosis of patients with high NLRs was significantly worse than that of patients with low NLRs. Theoretically, since an NLR is significantly associated with tumor progression, the difference in survival rates may be partly explained by differences in tumor volumes between the low NLR group and high NLR group. However, this study did not find any difference in the distribution of TNM stage between the two groups, and established that NLR is a significant prognostic factor based on the multivariate analysis. This result means that NLR does not simply reflect the advancement of cancer, and might be an independent prognostic factor reflecting immune status of host.
Since a peripheral blood cell count is regarded as a convenient assay method, a NLR may be as a useful clinical biological marker that can be used to predict one's tumor load and host immune status. Moreover, neutrophils are described to be a major source of circulating angiogenetic and growth factors that can accelerate tumor progression, whereas lymphocytes are known to dominate the host immune responses via cytotoxic cell death and cytokines production that can inhibit proliferation of tumor cells [715]. The ability of tumors to invade and metastasize is dependent both on the intrinsic characteristics of the tumor cells and on the environment around the tumor [16]. In addition, the abnormal phenotype of the tumor may stimulate an influx of inflammatory cells into tissues around it, and the tissue destruction and disruption caused by the physical effects of the tumor may trigger a more generalized and nonspecific inflammatory response [17]. As a consequence of these inflammations, neutrophils may increase while lymphocytes decrease with the advancement of cancer [18]. Indeed, some studies have shown that increased neutrophils can suppress the cytolytic activity of lymphocytes, natural killer cells and activated T cells. Lastly, there is good, consistent evidence that the presence of a systemic inflammatory response is associated with a progressive nutritional and functional decline in cancer patients and their subsequent poor outcome [1920].
The results of this study are in line with the existing studies, and demonstrated that an increased pretreatment NLR is associated with decreased overall survival, after adjusting known prognostic factors such as TNM stage. However, this study did not find any difference in the distribution of TNM stage between the two groups, which means NLR might be an independent prognostic factor reflecting immune status of host. To the best of our knowledge, this study enrolled the largest number of gastric cancer patients to date and calculated the NLR using ROC curve. On the other hand, this study also has some limitations. Firstly, this is a retrospective study conducted at a single institution. Secondly, we could not examine the patients' underlying disease which could affect the NLR status. However, except emergency operations, scheduled operations usually were performed in good patients' condition. So, the effect of infectious disease would be minimal.
In conclusion, the study verified that a high preoperative NLR (NLR ≥ 1.7) with advanced stage and old age (≥70 years) is a significant, prognostic factor for overall survival in patients with gastric cancer. That is, preoperative NLRs are simple, easily accessible laboratory findings that can be used to identify patients with poorer prognosis, although the mechanism should be elucidated by further basic research and clinical trials.
Figures and Tables
Fig. 1
Receiver operating curve of preoperative NLR (NLR, 1.7; sensitivity, 0.66; specificity, 0.54; positive predictive value, 0.18; negative predictive value, 0.91). NLR, neutrophil to lymphocyte ratio; AUC, area under curve.
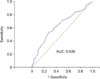
Fig. 2
Kaplan-Meier survival curve for significant variables in univariate analysis. NLR, neutrophil to lymphocyte ratio.

References
1. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Seo HG, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2009. Cancer Res Treat. 2012; 44:11–24.
2. Shin R, Jeong SY, Yoo HY, Park KJ, Heo SC, Kang GH, et al. Depth of mesorectal extension has prognostic significance in patients with T3 rectal cancer. Dis Colon Rectum. 2012; 55:1220–1228.
3. Strauss L, Bergmann C, Gooding W, Johnson JT, Whiteside TL. The frequency and suppressor function of CD4+CD25highFoxp3+ T cells in the circulation of patients with squamous cell carcinoma of the head and neck. Clin Cancer Res. 2007; 13:6301–6311.
4. Roxburgh CS, Salmond JM, Horgan PG, Oien KA, McMillan DC. Comparison of the prognostic value of inflammation-based pathologic and biochemical criteria in patients undergoing potentially curative resection for colorectal cancer. Ann Surg. 2009; 249:788–793.
5. Hwang JE, Kim HN, Kim DE, Choi HJ, Jung SH, Shim HJ, et al. Prognostic significance of a systemic inflammatory response in patients receiving first-line palliative chemotherapy for recurred or metastatic gastric cancer. BMC Cancer. 2011; 11:489.
6. Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M. The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology. 2007; 73:215–220.
7. Chochi K, Ichikura T, Majima T, Kawabata T, Matsumoto A, Sugasawa H, et al. The increase of CD57+ T cells in the peripheral blood and their impaired immune functions in patients with advanced gastric cancer. Oncol Rep. 2003; 10:1443–1448.
8. Gomez D, Farid S, Malik HZ, Young AL, Toogood GJ, Lodge JP, et al. Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after curative resection for hepatocellular carcinoma. World J Surg. 2008; 32:1757–1762.
9. Sarraf KM, Belcher E, Raevsky E, Nicholson AG, Goldstraw P, Lim E. Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg. 2009; 137:425–428.
10. Satomi A, Murakami S, Ishida K, Mastuki M, Hashimoto T, Sonoda M. Significance of increased neutrophils in patients with advanced colorectal cancer. Acta Oncol. 1995; 34:69–73.
11. Hirashima M, Higuchi S, Sakamoto K, Nishiyama T, Okada H. The ratio of neutrophils to lymphocytes and the phenotypes of neutrophils in patients with early gastric cancer. J Cancer Res Clin Oncol. 1998; 124:329–334.
12. Shimada H, Takiguchi N, Kainuma O, Soda H, Ikeda A, Cho A, et al. High preoperative neutrophil-lymphocyte ratio predicts poor survival in patients with gastric cancer. Gastric Cancer. 2010; 13:170–176.
13. Jung MR, Park YK, Jeong O, Seon JW, Ryu SY, Kim DY, et al. Elevated preoperative neutrophil to lymphocyte ratio predicts poor survival following resection in late stage gastric cancer. J Surg Oncol. 2011; 104:504–510.
14. Lee DY, Hong SW, Chang YG, Lee WY, Lee B. Clinical significance of preoperative inflammatory parameters in gastric cancer patients. J Gastric Cancer. 2013; 13:111–116.
15. Stockmann C, Schadendorf D, Klose R, Helfrich I. The impact of the immune system on tumor: angiogenesis and vascular remodeling. Front Oncol. 2014; 4:69.
16. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002; 420:860–867.
17. Nagtegaal ID, Marijnen CA, Kranenbarg EK, Mulder-Stapel A, Hermans J, van de Velde CJ, et al. Local and distant recurrences in rectal cancer patients are predicted by the nonspecific immune response; specific immune response has only a systemic effect--a histopathological and immunohistochemical study. BMC Cancer. 2001; 1:7.
18. Petrie HT, Klassen LW, Kay HD. Inhibition of human cytotoxic T lymphocyte activity in vitro by autologous peripheral blood granulocytes. J Immunol. 1985; 134:230–234.
19. el-Hag A, Clark RA. Immunosuppression by activated human neutrophils: dependence on the myeloperoxidase system. J Immunol. 1987; 139:2406–2413.
20. McMillan DC. Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care. 2009; 12:223–226.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download