Abstract
Vitelline veins are a pair of embryonic structures. The veins develop the portal vein system. Serious problems occur if the vitelline vein does not regress and becomes an aneurysm. Thrombus formation in the vitelline vein aneurysm could lead to portal vein thrombosis and portal hypertension unless promptly and correctly treated. Though vitelline vein aneurysm is an extremely rare anomaly, it rapidly progresses to portal vein thrombosis that requires prompt diagnosis and treatment. We reported a case of neonatal vitelline vein aneurysm and thrombosis that was cured by prompt operation.
Vitelline veins are a pair of embryonic structures that develop portal vein systems, including splenic vein, superior mesenteric vein, and portal vein. Most parts of vitelline veins spontaneously regress, except for the portal vein system [12]. The vitelline vein remnant that does not regress as normal, can be affected by aneurysmal dilatation followed by possible thrombosis. The thrombus would pass through the connection with portal venous system and cause portal vein thrombosis that leads to serious problems, including portal hypertension and brain infarction [23]. Though the vitelline vein aneurysm and thrombosis can develop fatal results, due to their extremely low incidence, only few cases are reported. Here, we reported a case of vitelline vein aneurysm with thrombosis in a neonate that was successfully treated with operation; we additionally reviewed the relevant literature.
A 1-day-old boy was referred to our department with a history of 3-cm-sized ellipsoidal cystic lesion below the liver detected by prenatal ultrasonography at 30 weeks of gestation. Pregnancy was uncomplicated and the 2,320-g male infant was delivered at 36 weeks of gestation by caesarian section. There were no other structural anomalies and chromosomal abnormality.
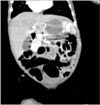
Postnatal Doppler sonography on the day of birth showed an elongated aneurismal tubular structure (Fig. 1). One day after birth, 3-dimensional CT revealed a 1.4-cm-sized abnormal aneurismal dilatation of the venous structure that had connection to the main portal vein and umbilicus, along with low attenuated hypoechoic lesion in the vitelline vein and distal portal vein, highly suggestive of the presence of vitelline vein aneurysm with thrombosis (Fig. 2).
Surgical exploration was performed to remove the venous thrombosis and dilatated venous portion via semilunar incision above the umbilicus. A vitelline vein aneurysm with 3.5-cm maximal diameter was present from the umbilicus at its most caudal portion, to the portal vein at its most cranial portion. After the division at the level of the umbilical ring, the dissection continued cranially and the aneurysm was resected just distal to the splenic vein inlet with thrombectomy. The postoperative course was uneventful. The ultrasound Doppler examination at 1 year after the operation revealed no evidence of thrombus formation from the superior mesenteric vein to the intrahepatic portal vein.
Understanding of portal-hepatic venous system development is needed for the evaluation and treatment of its congenital anomalies. The formation of the system begins at the 5th gestational week. Three pairs of veins are developed i.e., the cardinal veins, the umbilical veins and the vitelline veins [34]. Portal vein, hepatic veins and part of inferior vena cava come from umbilical veins and vitelline veins. Generally, cranial segments of left vitelline vein and caudal segments of right vitelline vein regress during the fetal period and splenic vein and the superior mesenteric vein are derived from the left vitelline vein [1]. In the first days after birth, the umbilical vein spontaneously obliterates by physiologic occurrence of thrombus [4]. In this case, as in the normal umbilical vein, thrombosis might occur at the abnormally patent vitelline vein aneurysm that regressed in the fetal period. Due to turbulent flow within the aneurysm, the thrombus might become rapidly bigger and increase the risk of spread to the portal vein and systemic circulation via patent connection to portal vein.
Generally, when fetal inraabdominal vascular dilatations are encountered, they are mostly fetal umbilical dilatations [1]. They are also a rare anomaly and sometimes led to fetal death [5]. Due to structural similarity, vitelline vein aneurysm occasionally mimics abnormal fetal umbilical vein dilatation [6]. To the best of our knowledge, vitelline vein aneurysm with thrombus is an extremely rare anomaly with only 6 cases reported in the English literature [123467] (Table 1). However, postnatal courses of both diseases are completely different. Vitelline vein aneurysm could cause thrombus that leads to portal hypertension and requires operation; whereas umbilical vein dilatations show relatively favorable pregnancy prognosis only with close fetal monitoring [5]. Kivilevitch and Achiron[2] suggested 3 criteria for differential diagnosis to umbilical vein dilatation. The criteria compromise 1. early gestational age (23-24 weeks); 2. abnormal course of vein (running downward and below the gallbladder); and 3. concomitant intrahepatic portal system variation with absence of the normal umbilicalportal venous system configuration [2]. Except for criteria 2, the criteria are not fully met in some cases, including the current case.
Doppler sonography is the most effective prenatal diagnostic tool. After birth, Doppler sonography also works as a screening test [13]. CT angiography is an effective additional modality to evaluate anatomy and progression of thrombus [16].
For patients with fetal vitelline vein aneurysm, multidisciplinary management is needed from the obstetrician, neonatologist, radiologist and pediatric surgeon. Its structures are similar to fetal intraabdominal umbilical vein dilatation that also causes potentially disastrous results, including fetal mortality [8]. Dilatated vitelline vein is connected to the placenta and fetal heart via portal veins, as in umbilical vein dilatation [26]; furthermore, vitelline vein might occasionally be the only vein that connects both structures due to abdnormal obliteration of the umbilical vein [16] and thrombus in the aneurysm is very dangerous and requires close fetal monitoring. Early postnatal detection and prompt treatment are important. The thrombosis might rapidly progress to the main portal vein within 10 days after birth [47]. Surgical thrombectomy with resection of vitelline vein including aneurysm is recommended [147]. Two reported cases showed progression of portal obstruction syndrome with portal hypertension after thrombectomy and aneurysm resection. These patients underwent surgery after involvement of thrombus in the intrahepatic portal vein [47]. Meanwhile, the patients who were operated early with thrombus confined distal to the confluence of splenic vein and superior mesenteric vein to portal vein, did not have complications and showed good prognosis.
In summary, if vitelline vein aneurysm is diagnosed and contains the thrombus, prompt surgical excision should be considered to prevent progression to portal vein thrombosis. Delayed operation for only a few days may have disastrous results including portal hypertension.
Figures and Tables
 | Fig. 1Ultrasonographic findings on the day of birth: (A) an elongated aneurismal tubular structure (V: vitelline vein aneurysm) with connection to the main portal vein (PV) coursing towards the umbilicus (U), (B) Color Doppler ultrasonography showed patent portal vein flow. |
References
1. Kang KW, Sung DJ, Park BJ, Kim MJ, Cho SB. Aneurysmal dilatation of persistent vitelline vein with thrombus in a neonate. Pediatr Radiol. 2014; 44:893–896.
2. Kivilevitch Z, Achiron R. Fetal extrahepatic vitelline vein aneurysm mimicking an umbilical vein varix. J Ultrasound Med. 2010; 29:1651–1656.
3. Scalabre A, Gorincour G, Hery G, Gamerre M, Guys JM, de Lagausie P. Evolution of congenital malformations of the umbilical-portal-hepatic venous system. J Pediatr Surg. 2012; 47:1490–1495.
4. Benoist G, Gauthier F, Belloy F, Laloum D, Herlicoviez M, Dreyfus M. Antenatal sonographic features of aneurysmal dilatation of a vitelline vein. Ultrasound Obstet Gynecol. 2007; 29:708–711.
5. Lee SW, Kim MY, Kim JE, Chung JH, Lee HJ, Yoon JY. Clinical characteristics and outcomes of antenatal fetal intra-abdominal umbilical vein varix detection. Obstet Gynecol Sci. 2014; 57:181–186.
6. Moon SB, Park KW, Jung SE. Abnormal direct entry of the umbilical vein into the portal vein: report of a case. Pediatr Surg Int. 2008; 24:1243–1245.
7. Hery G, Quarello E, Gorincour G, Franchi S, Gauthier F, de Lagausie P. Extrahepatic vitelline vein aneurysm: prenatal diagnosis and follow up. J Pediatr Surg. 2013; 48:e1–e4.
8. Beraud E, Rozel C, Milon J, Darnault P. Umbilical vein varix: importance of anteand post-natal monitoring by ultrasound. Diagn Interv Imaging. 2015; 96:21–26.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download