Abstract
Purpose
The role of preoperative localization studies is controversial in surgery of secondary hyperparathyroidism (sHPT). The aim of study was to evaluate the accuracy of preoperative ultrasonography (USG), CT, and 99mTc sestamibi scintigraphy (MIBI) in localizing enlarged parathyroid glands and to find the impact of correct localization in successful parathyroidectomy.
Methods
We compared operative findings with the preoperative localization of ultrasonography, computerized tomography and sestamibi scintigraphy in 109 patients with sHPT and identified well-visualized locations of abnormal parathyroid glands by evaluating the sensitivity of each imaging study with regard to typical locations of glands. We investigated the effect of preoperative imaging localization on the surgical outcomes by measuring the intraoperative parathyroid hormone (ioPTH) decrement for positive or negative imaging localization.
Results
USG (91.5%) had the highest sensitivity and MIBI (56.1%) had the lowest among 3 modalities. The sensitivity of combined USG and CT (95.0%) was the highest among combined 2 modalities. The combination of all 3 modalities (95.4%) had the highest sensitivity among the combinations of modalities. The reduction of ioPTH in patients with positive imaging localization (86.6%) was greater than negative imaging localization (84.2%), with no significant difference (P = 0.586). The recurrence or persistence of sHPT was not correlated with preoperative imaging localization (19 patients in negative, 16 in positive; P = 0.14).
Secondary hyperparathyroidism (sHPT) is an intractable disease of patients with chronic kidney disease (CKD), leading to substantial morbidity or mortality through severe osteodystrophy and vascular calcification [12]. Exacerbated sHPT may be refractory to phosphate lowering therapy and in such cases, parathyroidectomy (PTx) is indicated. However, surgical results are unsatisfactory with high rates of persistent and recurrent sHPT, ranging between 10% and 30%, due to difficulty in removing the complete parathyroid glands (PTGs) including supernumerary or ectopic glands, which are present in 13% and 22% on explorations, respectively [3456]. Thus, the preoperative localization of PTGs is considered important to succeed in PTx for sHPT. However, it is still controversial whether the preoperative localization of imaging studies could improve surgical outcomes in sHPT. It is suggested that preoperative imaging studies before initial PTx for sHPT is not indicated because bilateral neck exploration is required for identification of all glands, given that the underlying pathology is generally parathyroid hyperplasia. Imaging techniques are indicated for reoperative PTx when ectopic or supernumerary glands cannot be identified or recurrent diseases occur, despite adequate first-time surgical exploration. In addition, the sensitivity and specificity of imaging are limited in patients with CKD, perhaps because of variations in size and function among the different glands, despite increased overall metabolic activity [678910]. Intraoperative parathyroid hormone (ioPTH) monitoring is used in the effective surgical treatment for HPT as a wellrecognized predictor of surgical success [11,12,13,14]. It is expected that the association of preoperative imaging localization with intraoperative PTH monitoring could improve surgical outcomes.
The present study aimed to evaluate the sensitivity and the effect of surgical outcomes of ultrasonography (USG), 99m-Tc sestamibi scintigraphy (MIBI), and CT in the preoperative localization of PTGs in sHPT and to identify benefits of the combination of ioPTH measurement with imaging studies.
We included 109 patients with CKD on hemodialysis who were scheduled for PTx for refractory sHPT between January 2003 and April 2014. Medical record review included patient demographics, results of preoperative localization studies (negative or positive), the sensitivity of imaging studies, the number, size (the maximum longitudinal diameter, MLD) and location of PTGs identified on these studies and at pathology, surgical procedure performed, and surgical outcomes (recurrence or persistence). There were 43 females (39.4%) and 66 males (60.6 %). Mean age was 49.1 ± 10.4 years and mean dialytic years were 14.1 ± 6.1 years. Mean body mass index was 22.8 ± 4.1 kg/m2. Mean follow-up duration was 5.8 ± 4.3 years. All patients underwent preoperative USG, CT, MIBI, respectively. The study was approved by the local ethics committee, and written informed consent was obtained from all patients before preoperative diagnostic studies and PTx. USG was performed by surgeons and considered positive when there were oval, hypoechoic nodules clearly separated by the thyroid capsule. If the nodular lesions were suspected of being enlarged parathyroid tissue, fine needle aspiration with parathyroid washout was performed under ultrasound guidance. A positive cutoff value for the PTH washout was defined as being superior to the patient's serum PTH level. MIBI was interpreted as positive when there was a focal area of increased uptake showing a relative increase over time, but undetected in thyroid scintigraphy. In cases where enlargement of PTGs was noted, a subtotal or total PTx with or without autotransplantation was carried out. The surgery was performed by exploration of the neck initially focusing at the usual anatomic sites that harbor the upper and lower PTGs bilaterally. If fewer than 4 PTGs were located during this process, the search for the remaining PTGs proceeded by systematic sequential ipsilateral dissection and finger palpation of the thymus, level VI clearance, and sequential opening of the retropharyngeal space, retroesophageal space, and carotid sheath. If there was lesion suspected as parathyroid tissue during surgery, histologic analysis of frozen sections was conducted. If the intrathyroidal nodule suspected as parathyroid tissue was found at the anatomical site where no PTG was detected, partial thyroidectomy was performed. The thymectomy was done only when the induration was identified by finger palpation. All procedures were performed by the same surgeon. Baseline level of ioPTH prior to incision was determined. After exploration and resection of all enlarged PTGs, ioPTH levels were determined in the same fashion at 20 and 40 minutes after excision for ioPTH measurements. PTH levels were determined with the Elecsys 2010 apparatus (Roche Diagnostics, Indianapolis, IN, USA). Recurrence was defined as having PTH > 300 ng/mL in 6 months after surgery and persistence before 6 month after surgery [15]. Chi-square test and McNemar test were used for dichotomous and categorical variables and independent t-test for numerous variables. All P-values were 2-tailed, and for all tests, P < 0.05 was considered statistically significant.
One hundred and nine patients underwent PTx for sHPT. Eighty patients underwent total PTx with or without autotransplantation, 19 patients subtotal PTx and 10 partial PTx by removing less than 4 glands. At pathologic examination, nodular hyperplasia was shown in 86 patients (78.9%) and diffuse hyperplasia in 23 patients (21.1%). Recurrent or persistent patients were 35 (32.1%). When we compared negative localization group with positive, there was no significant difference in age, sex, years of dialysis, body mass index, preoperative PTH, calcium, phosphate, PTx, size of PTGs, ioPTH at pre-excision, after 20 minutes, 40 minutes, location, recurrence or persistence between negative and positive group except operation time (Table 1). The operation time in negative group (81.3 ± 23.6 minutes) was longer than in positive (65.2 ±17.4 minutes) group (P = 0.02). Four hundred twenty-three PTGs in the 109 patients were identified and surgically removed. Four hundred twenty-two PTGs were found in typical sites (106 glands were right upper, 107 right lower, 105 left upper, and 104 left lower) and 1 ectopic PTGs in the upper mediastinum. As shown in Table 2, USG had the highest sensitivity (91.5%) and MIBI had the lowest (56.1%) among the 3 modalities. The sensitivity of CT was 84.8%. USG and CT had higher sensitivity than MIBI with significant differences (P < 0.001). The sensitivity of combined USG and CT (95.0%) was the highest among combined 2 modalities. The combination of CT and MIBI had the lowest sensitivity (88.3%). The combination of all 3 modalities (95.4%) had the highest sensitivities among the combinations of modalities with no significant difference (P = 0.500) except the combination of CT and MIBI (P = 0.016). With regard to the location, the percentage of lower PTGs visualized by imaging modalities was higher than that of upper PTGs, with no significant difference (P = 0.549). Right lower, left lower, left upper, and right upper PTGs were arranged in order of sensitivity. The MLDs of PTGs visualized by modalities were larger than those of the ones missed (Table 3). In addition, MLDs of upper PTGs (16.2 ± 7.1 mm) were larger than those of lower PTGs (13.4 ± 5.6 mm) significantly (P = 0.001). For ectopic PTGs, USG, and CT were always negative, whereas MIBI was positive in 1 (0.9%), which was in superior mediastinal space and surgically removed. With regard to ioPTH monitoring, the reduction of ioPTH in patients with positive imaging localization (86.6%) was greater than negative imaging localization (84.2%), with no significant difference (P = 0.583) (Fig. 1). Successful PTx could be achieved by ioPTH monitoring irrespective of preoperative imaging localization in these patients.
The pathogenesis of sHPT, commonly arising in the setting of CKD, is complex and remains somewhat enigmatic. Impaired urinary phosphate excretion and hyperphosphatemia, along with decreased activity of renal 1-alpha hydroxylase have been implicated in the functional reduction of nephrons in CKD. Both result in hypocalcemia leading to sHPT. sHPT is linked to bone mineral disorder such as renal osteodystrophy, and cardiovascular morbidity and mortality, as compared with patients with non-CKD with the relative risk of death estimated as 1.06 to 3.9 [1617]. sHPT control in CKD is therefore desirable. Although the indications for PTx in sHPT are not well established, guidelines for PTX in sHPT of the National Kidney Foundation's Kidney Disease Quality Outcomes Initiative propose that patients with severe HPT (PTH > 800 pg/mL) associated with hypercalcemia and/or hyperphosphatemia, despite medical therapy, should be offered PTX [15]. In surgical treatment for sHPT, accurate localization of abnormal PTGs is needed to prevent recurrent or persistent disease and to perform more rapid and meticulous surgery in high risk patients with renal failure. Our study demonstrated that the sensitivity of USG, CT, MIBI was 91.5%, 84.8%, and 56.1%, respectively. USG had the highest sensitivity among 3 imaging studies. The sensitivity of the combination of USG with CT, USG with MIBI, CT with MIBI was 95.0%, 93.8%, and 88.3%, respectively. The sensitivity of the combination of USG, CT, and MIBI (95.4%) was higher than those of other combinations of 2 imaging modalties. The sensitivities in our study were as high as or higher than those in other studies. Although CT was not included in imaging studies, Saengsuda [18] found that parathyroid scan localized abnormal glands in 63.6% of patients with SHPT in a retrospective study that included 71 patients with primary HPT and sHPT. Perie et al. [9] showed that USG detected 75% of hyperplastic glands, while MIBI identified 66%. The combination of both modalities identified 88% of glands. Most missed glands on scintigraphy were superior glands. Vulpio et al. [7] reported that the sensitivity of MIBI and USG is 62% and 55% and the sensitivity of combined techniques is 73%. Another series of 11 patients reported a 91% sensitivity of MIBI in identifying hyperplastic glands in sHPT [19]. Although patients were exposed to radiation and contrast medium in CT, our study showed that CT might be an alternative and more accurate modality than USG in sHPT. Two studies showed that CT had an adequate utility of detecting abnormal PTGs in sHPT [2021]. Takagi et al. [20] demonstrated that CT had a higher sensitivity (86.7%) than USG (77.8%) in 1 of 2 studies. On the other hand, Adalet et al. [22] found the sensitivity of parathyroid scan is 25% in patients with sHPT or tertiary HPT. Another study also showed a low yield of preoperative localization studies in patients with sHPT with MIBI showing only 36.6% and USG showing 35.9% of surgically confirmed enlarged glands [8]. In a prospective study of Mohammadi et al. [23], the sensitivity of USG and MIBI, combined USG and MIBI was 54%, 25%, and 45%, respectively. A recent meta-analysis that included 24 studies with 471 patients showed 58% sensitivity of MIBI in detecting hyperplastic glands in sHPT [24]. This study indicated that lower PTGs were detected more frequently than upper PTGs, as shown in other studies [725]. Upper PTGs can be seen more inferiorly, deep in relation to the midpole of the thyroid lobes (4%), or they may be located at or above the most superior aspect of the thyroid (3%). Rarely, the superior glands can be found in the retropharyngeal (1%) or retroesophageal (1%) spaces, or in the thyroid gland itself (0.2%) [25]. This probably makes identification by imaging studies difficult. It seems difficult to localize all PTGs by imaging studies and to have similar sensitivities of imaging modalities in studies because PTG hyperplasia in sHPT is an asynchronous and asymmetrical process and 3 modalities are performed by different mechanisms or interpreted by surgeons or radiologists with different expertise and techniques [7]. Even if less than 4 glands removal was performed due to undetected abnormal or normal glands, combined imaging studies had a tendency of higher detection rate than each study alone, but with no significant difference. Preoperative imaging studies, specially combined studies in sHPT prevent unnecessary dissection by reducing the operation time in CKD patients with high operative risks, although they do not improve surgical outcomes.
The ioPTH measurements are a functional diagnostic tool during parathyroid surgery for prediction of postoperative outcome and thereby help surgeons to decide whether further exploration is necessary. In primary hyperparathyroidism, ioPTH measurements are used to facilitate unilateral and minimal invasive procedures or focused PTx [26]. In patients with sHPT, bilateral exploration is needed and the value of ioPTH measurements is less obvious. However, most studies suggested that ioPTH measurements in sHPT improve surgical results, especially in patients with 3 or 5 PTGs and patients with ectopic parathyroid tissue [1112131427]. Few studies conclude that ioPTH measurements cannot adequately predict surgical outcomes in patients with sHPT [1128]. Our study demonstrated that the reduction of ioPTH and the percentage decline (86.6%) in positive localization were similar to those (84.2%) of negative localization (P = 0.583). Although ioPTH measurement could improve surgical outcomes when the decline of ioPTH met with the criterion of success in sHPT, preoperative imaging localization could not predict surgical results because recurrence or persistence rate had no significant difference for positive or negative localization (P = 0.138). This study had some limitations since it was a retrospective and observational study for consecutive patients during a specific period and a single center study in a tertiary hospital. Hence, we could not evaluate the institutional variability as compared to smaller or community hospitals. A multicenter, randomized, prospective study of preoperative imaging modalities might be needed for more accurate and objective investigation.
In conclusion, the present study showed that the combined use of USG, CT, and MIBI, as well as each modality alone in the preoperative evaluation of CKD patients with sHPT has a high sensitivity to localize hyperfunctioning or hyperplastic PTGs in sHPT. Therefore, preoperative imaging localization prevented unnecessary dissection, but could not predict or improve surgical outcomes. The combination of localization imaging use and ioPTH measurement might be a worthwhile method to improve surgical success or outcomes considering the lack of a modality that leads to optimal surgical results in sHPT.
Figures and Tables
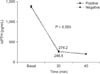 | Fig. 1Preoperative PTH and serum PTH levels after parathyroidectomy of negative and positive localization in secondary hyperparathyroidism. PTH, parathyroid hormone; ioPTH, intraoperative parathyroid hormone. |
Table 1
Comparison of demographic, histological, and biochemical data between negative and positive preoperative localization in secondary hyperparathyroidism

Values are presented as mean ± standard deviation or number (%).
PTH, parathyroid hormone; PTx, parathyroidectomy; ioPTH, intraoperative parathyroid hormone.
a)Negative: patients having undetected glands by any imaging modalities. b)Positive: patients having no undetected gland by all 3 modalities. *P < 0.05, statistically significant.
Table 2
Sensitivity (%) of USG, CT, MIBI, and combined imaging studies for locations of glands in secondary hyperparathyroidism

References
1. Tominaga Y, Tanaka Y, Sato K, Nagasaka T, Takagi H. Histopathology, pathophysiology, and indications for surgical treatment of renal hyperparathyroidism. Semin Surg Oncol. 1997; 13:78–86.
2. Martin KJ, Olgaard K, Coburn JW, Coen GM, Fukagawa M, Langman C, et al. Diagnosis, assessment, and treatment of bone turnover abnormalities in renal osteodystrophy. Am J Kidney Dis. 2004; 43:558–565.
3. Akerstrom G, Malmaeus J, Bergstrom R. Surgical anatomy of human parathyroid glands. Surgery. 1984; 95:14–21.
4. Roy M, Mazeh H, Chen H, Sippel RS. Incidence and localization of ectopic parathyroid adenomas in previously unexplored patients. World J Surg. 2013; 37:102–106.
5. Loftus KA, Anderson S, Mulloy AL, Terris DJ. Value of sestamibi scans in tertiary hyperparathyroidism. Laryngoscope. 2007; 117:2135–2138.
6. Alkhalili E, Tasci Y, Aksoy E, Aliyev S, Soundararajan S, Taskin E, et al. The utility of neck ultrasound and sestamibi scans in patients with secondary and tertiary hyperparathyroidism. World J Surg. 2015; 39:701–705.
7. Vulpio C, Bossola M, De Gaetano A, Maresca G, Bruno I, Fadda G, et al. Usefulness of the combination of ultrasonography and 99mTc-sestamibi scintigraphy in the preoperative evaluation of uremic secondary hyperparathyroidism. Head Neck. 2010; 32:1226–1235.
8. Lai EC, Ching AS, Leong HT. Secondary and tertiary hyperparathyroidism: role of preoperative localization. ANZ J Surg. 2007; 77:880–882.
9. Perie S, Fessi H, Tassart M, Younsi N, Poli I, St Guily JL, et al. Usefulness of combination of high-resolution ultrasonography and dual-phase dual-isotope iodine 123/technetium Tc 99m sestamibi scintigraphy for the preoperative localization of hyperplastic parathyroid glands in renal hyperparathyroidism. Am J Kidney Dis. 2005; 45:344–352.
10. Kawata R, Kotetsu L, Takamaki A, Yoshimura K, Takenaka H. Ultrasonography for preoperative localization of enlarged parathyroid glands in secondary hyperparathyroidism. Auris Nasus Larynx. 2009; 36:461–465.
11. Echenique Elizondo M, Diaz-Aguirregoitia FJ, Amondarain JA, Vidaur F. Intraoperative monitoring of intact PTH in surgery for renal hyperparathyroidism as an indicator of complete parathyroid removal. World J Surg. 2005; 29:1504–1509.
12. Seehofer D, Rayes N, Klupp J, Steinmuller T, Ulrich F, Muller C, et al. Predictive value of intact parathyroid hormone measurement during surgery for renal hyperparathyroidism. Langenbecks Arch Surg. 2005; 390:222–229.
13. Lokey J, Pattou F, Mondragon-Sanchez A, Minuto M, Mullineris B, Wambergue F, et al. Intraoperative decay profile of intact (1-84) parathyroid hormone in surgery for renal hyperparathyroidism: a consecutive series of 80 patients. Surgery. 2000; 128:1029–1034.
14. Barczynski M, Cichon S, Konturek A, Cichon W. A randomised study on a new cost-effective algorithm of quick intraoperative intact parathyroid hormone assay in secondary hyperparathyroidism. Langenbecks Arch Surg. 2005; 390:121–127.
15. National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003; 42:4 Suppl 3. S1–S201.
16. Trombetti A, Stoermann C, Robert JH, Herrmann FR, Pennisi P, Martin PY, et al. Survival after parathyroidectomy in patients with end-stage renal disease and severe hyperparathyroidism. World J Surg. 2007; 31:1014–1021.
17. Madorin C, Owen RP, Fraser WD, Pellitteri PK, Radbill B, Rinaldo A, et al. The surgical management of renal hyperparathyroidism. Eur Arch Otorhinolaryngol. 2012; 269:1565–1576.
18. Saengsuda Y. The accuracy of 99m Tc-MIBI scintigraphy for preoperative parathyroid localization in primary and secondary-tertiary hyperparathyroidism. J Med Assoc Thai. 2012; 95:Suppl 3. S81–S91.
19. Hindie E, Urena P, Jeanguillaume C, Melliere D, Berthelot JM, Menoyo-Calonge V, et al. Preoperative imaging of parathyroid glands with technetium-99m-labelled sestamibi and iodine-123 subtraction scanning in secondary hyperparathyroidism. Lancet. 1999; 353:2200–2204.
20. Takagi H, Tominaga Y, Uchida K, Yamada N, Morimoto T, Yasue M. Image diagnosis of parathyroid glands in chronic renal failure. Ann Surg. 1983; 198:74–79.
21. Kohri K, Ishikawa Y, Kodama M, Katayama Y, Iguchi M, Yachiku S, et al. Comparison of imaging methods for localization of parathyroid tumors. Am J Surg. 1992; 164:140–145.
22. Adalet I, Hawkins T, Clark F, Wilkinson R. Thallium-technetium-subtraction scintigraphy in secondary hyperparathyroidism. Eur J Nucl Med. 1994; 21:509–513.
23. Mohammadi A, Moloudi F, Ghasemi-Rad M. Preoperative localization of parathyroid lesion: diagnostic usefulness of color doppler ultrasonography. Int J Clin Exp Med. 2012; 5:80–86.
24. Caldarella C, Treglia G, Pontecorvi A, Giordano A. Diagnostic performance of planar scintigraphy using 99mTc-MIBI in patients with secondary hyperparathyroidism: a meta-analysis. Ann Nucl Med. 2012; 26:794–803.
25. Harari A, Mitmaker E, Grogan RH, Lee J, Shen W, Gosnell J, et al. Primary hyperparathyroidism patients with positive preoperative sestamibi scan and negative ultrasound are more likely to have posteriorly located upper gland adenomas (PLUGs). Ann Surg Oncol. 2011; 18:1717–1722.
26. Inabnet WB. Intraoperative parathyroid hormone monitoring. World J Surg. 2004; 28:1212–1215.
27. Weber T, Zeier M, Hinz U, Schilling T, Buchler MW. Impact of intraoperative parathyroid hormone levels on surgical results in patients with renal hyperparathyroidism. World J Surg. 2005; 29:1176–1179.
28. Yamashita H, Cantor T, Uchino S, Watanabe S, Ogawa T, Moriyama T, et al. Sequential changes in plasma intact and whole parathyroid hormone levels during parathyroidectomy for secondary hyperparathyroidism. World J Surg. 2005; 29:169–173.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download