Abstract
Purpose
To determine the efficacy of a retrievable inferior vena cava filter (IVCF) for patients with deep vein thrombosis (DVT) and transient contraindication for anticoagulant therapy, and to analyze the risk factors for filter thrombus in these patients.
Methods
We retrospectively reviewed the records of 70 patients who received a retrievable IVCF from January 2007 to June 2014 because of documented DVT and transient contraindication for anticoagulant therapy. The protocol for follow-up care generally consisted of anticoagulant therapy after high-risk periods, follow-up CT around 2 weeks after IVCF placement, and retrieval if possible.
Results
The 70 patients had a mean age of 61.8 years (range, 17-88 years), and 30 were male (43%). The indications for IVCF were recent trauma including surgery in 48 patients, recent hemorrhage in 14, and planned major surgery with DVT in 8 patients. Follow-up CT of 61 patients (87%) was performed. Aggravation or new development of pulmonary embolism (PE) was not found in any patient. Filter thrombus was detected in 23% of patients with follow-up CT (14/61). Filter thrombus was not detected in patients with isolated calf vein thrombosis (ICVT) (P = 0.079). The risk factor for filter thrombus was DVT progression on follow-up CT (P = 0.007) on multivariate analysis.
Pulmonary embolism (PE) is a major preventable cause of death in hospitalized patients [1]. The mainstay of treatment for PE and deep vein thrombosis (DVT) is anticoagulant drugs. However, for some patients who either cannot tolerate anticoagulant drugs or for whom the risk of PE is too high, other measures such as inferior vena cava (IVC) interruption must be considered. For this purpose, the first IVC filter (IVCF) was introduced in 1967 [2] and several other permanent IVCFs were approved subsequently. However, recurrent DVT and IVC thrombosis associated with IVCF were documented to increase with prolonged IVCF indwelling times [3]. Other complications, such as filter fracture, IVC penetration by filter legs, and filter migration were increasingly reported [4,5,6]. In addition, many patients were in temporary risk of PE because of trauma, surgery, and immobilization. Retrieval of the filters is thus attractive because the long-term complications of a permanent IVCF can be eliminated with this strategy.
Currently, the indications for installation of a retrievable IVCF in medical or trauma patients at high risk of developing a PE differ according to various guidelines [7,8,9]. Nevertheless, the most important consensus for installation of a retrievable IVCF is the contraindication for anticoagulant therapy in patients with venous thromboembolism (VTE). However, the exact nature of the protective role of IVCFs for the development of PE is uncertain because of mixed results from different indications, including placement for documented VTE and prophylaxis [10,11]. Moreover, the risk factors for filter thrombus after instillation of IVCF are not clear.
The purpose of the present study was to determine the efficacy of retrievable IVCFs for patients with acute DVT and transient contraindication for anticoagulant therapy, and to analyze the risk factors for filter thrombus in these patients, in consideration of absolute indications for retrievable IVCFs.
We reviewed the records of 130 patients who had retrievable IVCFs placed for various reasons related to protection against PE between January 2007 and June 2014. An IVCF was used prophylactically in 6 patients without documented VTE. Other indications for IVCF were patients with a high-risk medical condition (n = 26), as an adjunctive procedure before endovenous intervention (n = 22), and for a free-floating IVC thrombus (n = 4). After exclusion of prophylaxis and the abovementioned cases, 72 patients received a retrievable IVCF because of demonstrated acute VTE with contraindication for anticoagulant therapy (DVT with or without PE in 70 patients, PE only in 2 patients). After excluding the 2 patients who had only PE, 70 patients with documented DVT were included in this study. Records were reviewed after obtaining approval from Institutional Review Board of Kyungpook National University Hospital. Written informed consent from patients for review of the medical records was exempted by the board because of the retrospective nature of this study. Patients were excluded from this study for specific reasons as follows: (1) patients with high-risk medical conditions, because filter thrombosis and PE were not evaluated radiologically in most of these patients because of their poor general condition, and the filter was used permanently; and (2) patients with peripheral endovenous intervention, because filter thrombosis could be affected by endovenous manipulation.
The diagnostic methods for DVT and PE were combined one-stage indirect computed tomographic venography after completion of CT pulmonary angiography in 68 patients. The other 2 patients included in the present study underwent duplex ultrasonography with pulmonary CT angiography. A radiologist (J.M.L.) diagnosed DVT and PE by CT based on the characteristic presence of an intraluminal filling defect, or a localized nonopacified venous segment [12].
After a diagnosis of DVT, all included patients had received a retrievable IVCF with the intention of its subsequent retrieval. In general, anticoagulant therapy was started after the period of high risk of bleeding. The anticoagulant therapy consisted of low-molecular-weight heparin (enoxaparin, 1 mg/kg twice a day) followed by warfarin or oral rivaroxaban (15 mg twice a day for 3 weeks followed by 20 mg once a day). Follow-up CT was usually performed around 2 weeks after IVCF placement. The changes in DVT, PE, and filter thrombus after IVCF placement were evaluated. The decision for retrieval was determined according to the patient's general condition, ongoing contraindication for anticoagulant therapy, immobilization status, and filter thrombus. In patients with large trapped thrombus within IVCF or IVC occlusion distal to IVCF, filter retrieval was not performed and additional period of anticoagulation was adopted. The decision for filter retrieval was discussed between the radiologist (J.M.L.) and the vascular surgeons (H.K.K. and S.H.). Anticoagulant therapy was not necessarily discontinued for filter retrieval. After sterile preparation, venous access was obtained with ultrasound guidance. Digital subtraction cavography was performed in the anteroposterior projection. An orthogonal view was not routinely obtained. Further retrieval procedure continued according to the instructions of the various filter manufacturers. After filter retrieval, anticoagulant therapy was continued for 3 to 6 months.
The outcomes of interest in the present study were aggravated or newly developed PE on follow-up CT at around 2 weeks after IVCF placement, filter thrombosis within the IVCF as a surrogate marker of PE protection, risk factors for filter thrombosis, and filter retrieval rate with causes of nonretrieval. Filter thrombosis was defined as combined isolated trapped emboli within IVCF and IVC thrombosis distal to IVCF because it can be caused by large trapped emboli followed by distal thrombosis.
An independent Student t-test was used to compare the differences between continuous variables in patients with or without filter thrombosis on follow-up CT. Sixteen categorical variables tested were subjected to chi-square analysis (if sample size was adequate) or Fisher exact test (for smaller samples). Multivariate analysis was performed using logistic regression. Odds ratio (OR), hazard ratio, and 95% confidence interval (CI) were calculated. All statistical analyses were performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Differences were considered significant when P < 0.05.
Of the 70 patients included in the present study, the transient contraindications for anticoagulant therapy were as follows: recent trauma including recent major surgery in 48 patients (recent trauma, 43; recent surgery, 5), recent major or critical site bleeding in 14 patients, and planned major surgery without recent trauma or bleeding in 8 patients (Table 1). The mean interval between trauma or recent bleeding to diagnosis of DVT was 12 days (range, 1-40 days). Among 8 patients with planned major surgery, 7 patients presented with malignancy and 1 patient demonstrated abdominal aortic aneurysm with impending rupture sign. These patients received operation after IVCF placement without postponement of operation.
The average age of patients was 61.8 ± 14.6 years (range, 17-88 years). Of the 70 patients included, 30 (43%) were male. Twenty-nine patients (41%) had concomitant PE at the time of initial CT. The proximal level of DVT was IVC in 10 patients, iliac veins in 15, common femoral vein in 7, femoropopliteal vein in 29, and isolated calf vein thrombosis (ICVT) in 9. DVT occurred in the right limb in 23 patients, and in the left limb in 34. Thirteen patients had DVT in bilateral lower limbs. Of the 29 patients with documented PE, the main pulmonary artery was involved in 9 patients, the lobar artery in 15, and the segmental artery in 5. Detailed characteristics of VTE, comorbidities, and reasons for contraindication for anticoagulant therapy are summarized in Table 1. Most of the filters in our series were Celect filters (n = 53; 76%; Cook, Bloomington, IN, USA), followed by Günther Tulip filters (n = 15; 21%; Cook), and OptEase filters (n = 2; Cordis, Warren, NJ, USA).
Of those patients who received a retrievable IVCF placement, 43 (61%) were placed on anticoagulant therapy after filter placement. The mean interval from filter placement to anticoagulant therapy was 7 days (median, 5 days; range, 1-26 days). Forty-five patients (64%) received surgery after IVCF placement and the mean interval between filter placement and surgery was 6 days (median, 3 days; range, 0-27 days). The most common operation was orthopedic surgery in 38 patients, followed by gastrointestinal surgery in 3 patients, gynecological surgery in 2 patients, and hematoma evacuation in 2 patients.
Sixty-one patients underwent follow-up CT around 2 weeks after filter placement. The mean interval between filter placement and follow-up CT was 13 days (median, 12 days; range, 6-28 days). Nine patients did not have follow-up CT because of death (n = 3), poor general condition (n = 4), and follow-up loss (n = 2). In these 61 patients, new or aggravated PE was not detected in any patient. Of 24 patients presenting with PE on initial CT, resolution of PE was detected in 15 on follow-up CT. Eight patients demonstrated improvement of PE. One patient showed no definite change of PE. Twelve patients demonstrated resolution of DVT, 28 with improvement, 11 without definite change. DVT was aggravated or newly developed in another site in 10 patients. The status of PE and DVT on follow-up CT was not related to the subsequent anticoagulant therapy (P = 0.747 for DVT, P = 0.699 for PE).
Of the 61 patients who underwent a follow-up CT scan, filter thrombosis was detected in 14 (23%). Of these 14 patients, 11 had an isolated trapped embolus in the IVCF, and 3 had total IVC occlusion distal to the IVCF (Fig. 1). In univariate risk factor analysis for filter thrombosis, DVT progression on follow-up CT was demonstrated as a significant risk factor for filter thrombosis (P = 0.007). ICVT tended to be a negative predictor of filter thrombosis (P = 0.079). There was no filter thrombosis in patients with ICVT at initial presentation (Table 2). Multivariate analysis for filter thrombosis using logistic regression revealed that DVT progression on follow-up CT was the only significant independent risk factor for filter thrombosis (P = 0.007; OR, 8.750; 95% CI, 1.794-42.673).
The IVCF was successfully retrieved from 40 of the 70 patients. The rate of filter retrieval as intention to treat was 57%. The mean interval from filter placement to retrieval was 19 days (median, 14 days; range 7-108 days). There was no complication during filter retrieval except for two cases of failed retrieval because of an embedded filter. There were many reasons for nonretrieval, the main ones being: poor general condition followed by permanent use of the retrievable IVCF in 9 patients (poor medical condition in 6, continuous risk of bleeding that limited use of anticoagulant drugs in 2, quadriplegia in 1); patient death (n = 3); large trapped embolus or IVC thrombosis (n = 9); follow-up loss (n = 5); failed retrieval (n = 2); and aggravation of DVT (n = 2). Of 14 patients with filter thrombosis on follow-up CT, filter retrieval was performed in 5 after an additional period of anticoagulant therapy. Follow-up status of IVCF after placement was summarized in Fig. 2.
Our present study demonstrated a possible beneficial role of retrievable IVCF considering no aggravation or new development of PE with 23% (14/61) having a filter thrombus as a surrogate marker of PE protection in patients with an absolute indication for IVCF. All patients included in the present study had DVT and transient contraindication for anticoagulant therapy. Most patients (87%) underwent follow-up CT at around 2 weeks after IVCF placement for PE and filter thrombosis evaluation because this period was considered as the most important for PE protection [13].
With the recent development of retrievable IVCFs, filters are increasingly being placed in patients who are able to tolerate anticoagulant drugs or used prophylactically in DVT-free patients considered at high risk of PE [14]. However, as described in the guidelines of the American College of Chest Physicians in 2012 [7], the main indication and purpose of retrievable IVCFs are to prevent PE in patients with VTE and contraindication for anticoagulant therapy. Retrieval is necessary after the high-risk period for bleeding to avoid any long-term adverse effect of a retained filter. Currently, reports regarding the efficacy of retrievable IVCFs are somewhat confusing because the indications are mixed, including absolute, relative, and prophylactic use. In the PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) study, permanent IVCF was effective in the prevention of PE as an adjunct to anticoagulant therapy in patients with acute DVT who were considered to be at high risk of PE [15]. Moreover, in patients for whom anticoagulant therapy was contraindicated, the relative risk of PE may have been higher compared with PREPIC study participants because anticoagulant therapy was not possible.
The incidence of filter thrombus is known to vary depending on indwelling time and detection method [11]. The total incidence of filter thrombus in the cavogram during filter retrieval was 6.5% in 440 patients with mean indwelling time of 95 days and the incidence was highest for an indwelling interval of 0-30 days with a rate of 8% [11]. A higher incidence (17%-19%) of filter thrombus in other series with a relatively short IVCF indwelling time has been reported [11,16,17]. The rate of filter thrombus found in the present study was 23% with a mean indwelling time of 13 days, which is higher than the rate published for other studies. This discrepancy could be the result of a difference in the indication for IVCF. Our present study included patients with an absolute indication for IVCF (demonstrated DVT and contraindication for anticoagulant therapy). Therefore, relative indication with possible use of anticoagulant drugs or prophylactic use without VTE was excluded. In addition, majority of patients in our study did not receive any anticoagulant drugs in the early period after filter insertion because of the risk of bleeding. Three patients with filter thrombus in our study showed IVC occlusion distal to the IVCF. These cases may be considered to result from complications of IVCF placement. However, it is difficult to demonstrate the exact cause of IVC occlusion because it can be caused by a complication of the IVCF or by a sequence of large trapped emboli followed by a distal thrombosis within the IVC distal to the filter. After consideration of these three cases as complications of IVCF, 18% of patients (11/61) in our study had a trapped thrombus. Therefore, our findings can be considered to provide supportive evidence for the use of a retrievable IVCF in patients with DVT and contraindications for anticoagulant therapy.
In the present study, we attempted to find strong risk factors for filter thrombus before the placement of IVCF because this knowledge may be helpful in consideration of IVCF placement in patients with DVT. However, progression of DVT on follow-up CT after IVCF placement was the only independent risk factor for filter thrombus. We could not find any risk factors at initial presentation. Interestingly, 9 patients included in our study received IVCF because of ICVT. The reason for IVCF placement in these patients was combined PE in 4 patients and 5 patients were anticipated to major orthopedic surgery. However, we could not find any filter thrombus in these patients on follow-up CT. It is well known that ICVT rarely causes clinically important PE, although ICVT can involve the proximal vein in one-quarter of patients without treatment [18,19]. In the present study, it was difficult to determine the necessity of IVCF in patients with ICVT and contraindication for anticoagulant therapy because of their relatively small number. A study including a larger number of these patients is necessary to confirm our findings. A limitation of our study is that CT venography was used for evaluation of calf vein thrombosis. Although CT venography for diagnosis of proximal DVT demonstrated high sensitivity (95.9%) and specificity (95.2%) in a meta-analysis [20], it was not well studied for acute calf vein thrombosis. The majority of our patients presented with traumatic injury such as pelvic and long bone injury. Therefore, our main method for VTE evaluation consisted of one-stage indirect CT venography after completion of CT pulmonary angiography because it added only 3-5 minutes to the evaluation of DVT and duplex ultrasonography was not possible in many patients [21].
The rate of complications following filter insertion may be considered as low, but the risk is likely to increase if IVCFs are left in place. The PREPIC study showed an increased absolute risk of DVT of nearly 10% following filter insertion [3]. Other complications associated with IVCFs such as vena cava perforation, filter migration with or without embolization, and cardiac tamponade have been reported [22,23,24]. Importantly, the retrieval rate in one meta-analysis of 37 studies was also low (34%) [10]. Our filter retrieval rate of 57% was higher than that reported elsewhere. The most common reasons for nonretrieval in patients included in our study were poor general condition and filter thrombosis. The higher rate of retrieval in the patients included in our study may be because most suffered from trauma and the retrieval was performed during the same admission period. Therefore, follow-up loss of these patients was minimal.
A major limitation of the present study is its retrospective nature and the small patient sample that was monitored over a long period, which may result in possible patient selection and treatment bias. Among the 130 patients who received an IVCF, we excluded 58 with relative or prophylactic indications for IVCF placement. The outcomes of IVCFs in this group of patients allow us to understand the advantages and disadvantages from a rather liberal use of IVCFs. However, the primary outcome assessment was the changes in PE and filter thrombosis after IVCF placement. As described in the Methods section, especially in patients with high-risk medical conditions, filter thrombosis and PE were not evaluated radiologically in most patients because of their poor general condition and the filter was used permanently. Follow-up was difficult in most of these patients. Moreover, 9 patients did not undergo follow-up CT for various reasons. This particular limitation prohibits us from assessing the exact status of filter thrombosis or PE in these patients, and there is the possibility of under- or overestimating the actual events, because of incomplete follow-up imaging.
In conclusion, in our study, retrievable IVCFs could prevent aggravation or the new development of PE in patients with DVT and transient contraindication for anticoagulant therapy. DVT progression on follow-up CT was associated with filter thrombosis and ICVT was not related to filter thrombosis. A large-scale study is necessary to confirm these findings.
Figures and Tables
Fig. 1
Examples of filter thrombus on follow-up CT. (A) Image from a 57-year-old man with a pelvic bone fracture and femoropopliteal deep vein thrombosis who had a Celect filter inserted preoperatively. After 14 days, follow-up CT scan showed filter thrombus within inferior vena cava filter (arrow). (B) Image from a 51-year-old woman with cerebral hemorrhage and popliteal vein thrombosis who received a Celect filter inserted for prevention of further pulmonary embolism. After 11 days, follow-up CT scan showed filter thrombus with total thrombotic occlusion of inferior vena cava filter distal to the filter (arrow).
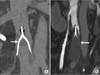
Fig. 2
Flow chart of IVC filters in patients with DVT and transient contraindication for anticoagulation. IVC, inferior vena cava; DVT, deep vein thrombosis.

References
1. Anderson FA Jr, Wheeler HB, Goldberg RJ, Hosmer DW, Patwardhan NA, Jovanovic B, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med. 1991; 151:933–938.
2. Mobin-Uddin K, McLean R, Bolooki H, Jude JR. Caval interruption for prevention of pulmonary embolism. Long-term results of a new method. Arch Surg. 1969; 99:711–715.
3. PREPIC Study Group. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study. Circulation. 2005; 112:416–422.
4. Malgor RD, Labropoulos N. A systematic review of symptomatic duodenal perforation by inferior vena cava filters. J Vasc Surg. 2012; 55:856–861.e3.
5. Sella DM, Oldenburg WA. Complications of inferior vena cava filters. Semin Vasc Surg. 2013; 26:23–28.
6. Zhou D, Moon E, Bullen J, Sands M, Levitin A, Wang W. Penetration of Celect inferior vena cava filters: retrospective review of CT scans in 265 patients. AJR Am J Roentgenol. 2014; 202:643–647.
7. Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141:2 Suppl. e419S–e494S.
8. Kaufman JA, Kinney TB, Streiff MB, Sing RF, Proctor MC, Becker D, et al. Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference. J Vasc Interv Radiol. 2006; 17:449–459.
9. Rogers FB, Cipolle MD, Velmahos G, Rozycki G, Luchette FA. Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group. J Trauma. 2002; 53:142–164.
10. Angel LF, Tapson V, Galgon RE, Restrepo MI, Kaufman J. Systematic review of the use of retrievable inferior vena cava filters. J Vasc Interv Radiol. 2011; 22:1522–1530.e3.
11. Teo TK, Angle JF, Shipp JI, Bluett MK, Gilliland CA, Turba UC, et al. Incidence and management of inferior vena cava filter thrombus detected at time of filter retrieval. J Vasc Interv Radiol. 2011; 22:1514–1520.
12. Loud PA, Katz DS, Bruce DA, Klippenstein DL, Grossman ZD. Deep venous thrombosis with suspected pulmonary embolism: detection with combined CT venography and pulmonary angiography. Radiology. 2001; 219:498–502.
13. Kakkar VV, Corrigan TP, Fossard DP, Sutherland I, Thirwell J. Prevention of fatal postoperative pulmonary embolism by low doses of heparin: reappraisal of results of international multicentre trial. Lancet. 1977; 1:567–569.
14. Smouse B, Johar A. Is market growth of vena cava filters justified? A review of indications, use, and market analysis. Endovasc Today. 2010; 2:74–77.
15. Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prevention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998; 338:409–415.
16. Wicky S, Doenz F, Meuwly JY, Portier F, Schnyder P, Denys A. Clinical experience with retrievable Gunther Tulip vena cava filters. J Endovasc Ther. 2003; 10:994–1000.
17. Millward SF, Oliva VL, Bell SD, Valenti DA, Rasuli P, Asch M, et al. Günther Tulip Retrievable Vena Cava Filter: results from the Registry of the Canadian Interventional Radiology Association. J Vasc Interv Radiol. 2001; 12:1053–1058.
18. Lagerstedt CI, Olsson CG, Fagher BO, Oqvist BW, Albrechtsson U. Need for long-term anticoagulant treatment in symptomatic calf-vein thrombosis. Lancet. 1985; 2:515–518.
19. Kearon C, Julian JA, Newman TE, Ginsberg JS. Noninvasive diagnosis of deep venous thrombosis. McMaster Diagnostic Imaging Practice Guidelines Initiative. Ann Intern Med. 1998; 128:663–677.
20. Thomas SM, Goodacre SW, Sampson FC, van Beek EJ. Diagnostic value of CT for deep vein thrombosis: results of a systematic review and meta-analysis. Clin Radiol. 2008; 63:299–304.
21. Yun WS, Lee KK, Cho J, Kim HK, Kyung HS, Huh S. Early treatment outcome of isolated calf vein thrombosis after total knee arthroplasty. J Korean Surg Soc. 2012; 82:374–379.
22. Caplin DM, Nikolic B, Kalva SP, Ganguli S, Saad WE, Zuckerman DA, et al. Quality improvement guidelines for the performance of inferior vena cava filter placement for the prevention of pulmonary embolism. J Vasc Interv Radiol. 2011; 22:1499–1506.
23. Rogers NA, Nguyen L, Minniefield NE, Jessen ME, de Lemos JA. Fracture and embolization of an inferior vena cava filter strut leading to cardiac tamponade. Circulation. 2009; 119:2535–2536.
24. Tam MD, Spain J, Lieber M, Geisinger M, Sands MJ, Wang W. Fracture and distant migration of the Bard Recovery filter: a retrospective review of 363 implantations for potentially life-threatening complications. J Vasc Interv Radiol. 2012; 23:199–205.e1.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download