Abstract
Purpose
The assurance of a negative resection margin is significant in rectal cancer as it indicates a reduced risk of local recurrence; thus, sufficient length of the resection margin is strongly required. The purpose of this study was to analyze the relationship between the length of the distal resection margin (DRM) and local recurrence or survival rate and to evaluate the possibility of performing sphincter-conserving surgery.
Methods
The medical records of 218 rectal cancer patients were analyzed. Patients were classified into three groups according to the length of the DRM as follows: group 1, DRM < 1 cm; group 2, 1 cm ≤ DRM ≤ 2 cm; and group 3, DRM > 2 cm.
Results
Of 218 patients enrolled, 81 were in group 1, 66 in group 2, and 71 in group 3. The 5-year survival rates were 78.2%, 78.2%, and 76.8% for groups 1, 2, and 3, respectively, and there were no statistically significant differences in survival (P = 0.913). Local recurrence was found in 2 patients in group 1, 1 patient in group 2, and 1 patient in group 3; there were no statistically significant differences in local recurrence (P = 0.908).
Achieving a clear resection margin and performing en bloc resection are crucial in rectal cancer surgery. Thus, surgeons often attempt to perform total mesorectal excision (TME) [1,2,3,4] and obtain a minimum 2-cm distal resection margin (DRM) to prevent microscopic intramural spread. In cases of low rectal cancer, a DRM of at least 1 cm is commonly required [1,5]. When achieving a sufficient DRM is challenging, abdominoperineal resection (APR) is usually performed, resulting in a permanent stoma; this may negatively affect patients' quality of life and create an economic burden due to the need for stoma-related products. Additionally, such a consequence might also affect patients' pride.
However, as patients' quality of life is often prioritized in recent cancer treatment, and more studies have focused on other therapeutic modalities such as chemoradiation therapy, 'the 1-cm rule of distal bowel resection margin' might be controversial [6,7,8,9,10,11,12,13,14,15]. Nonetheless, surgeons, with skepticism towards insufficient DRMs, often prefer proctectomy. Therefore, the present study was conducted to identify the optimal DRM length and review the indication for APR by analyzing the correlation between DRM length and local recurrence or survival rates in rectal cancer patients who underwent low anterior resection (LAR).
We retrospectively analyzed the medical records of patients diagnosed with rectal cancer located within 12 cm from the anal verge. Tumor location was determined based on the results of a digital rectal examination, colonoscopy, and sigmoidoscopy conducted prior to surgery.
Patients with stage IV rectal cancer (cases for which synchronous distant metastasis was detected on preoperative radiologic evaluations such as chest radiography, abdominal CT, pelvic CT, and PET) were excluded from this study. Additionally, patients with tumors at the circumferential resection margin observable on permanent histopathologic examination and those undergoing APR for tumors that metastasized to the DRMs were also excluded. Finally, a total of 218 patients were enrolled in this study.
Preoperative radiotherapy was indicated for tumors of clinical stage T3 or T4 and lymph node positivity. The treatment course included 2-Gy three-field technique irradiation for a total dose of 50 Gy in combination with 5-fluorouracil (5-FU) and leucovorin (LV); this was 'long course' radiotherapy. Surgery was performed 6 weeks after treatment completion in patients receiving preoperative chemoradiation.
All surgical procedures were performed by 3 qualified, experienced colorectal surgeons. The standard surgical procedure of rectal cancer including TME was performed in all patients with an initial aim to achieve a 2-cm DRM. However, a resection margin of 1 or 2 cm was difficult to achieve when rectal cancer was located close to the anorectal junction. In such cases, a specimen was resected at the farthest possible location from the lower margin of the tumor. When a tumor was neither visibly detected nor observable on pathological examination of its frozen sections, LAR was performed regardless of the length. In particular, a double-stapling anastomotic instrument was safely placed in the anal canal so that a doughnut ring could be properly formed. In cases unsuitable for anastomosis with a double-stapling anastomotic instrument, intersphincteric anastomosis were performed. And diverting stomas were utilized either.
The DRM length was measured from the fresh specimen without formalin fixation. In this study, a DRM was defined as the distance between the inferior margin of a tumor and the distal inferior margin of the specimen, wherein the doughnut was not included.
The postoperative treatment and follow-up plans were designed in accordance with National Comprehensive Cancer Network (NCCN) guidelines and adapted to practical circumstances. CEA assays, colonoscopies, and abdominal CT were performed.
Adjuvant chemotherapy regimens with 5-FU/LV, FOLFOX4 (oxaliplatin with 5-FU and LV), FOLFIRI (irrinotecan with 5-FU and LV) were indicated. CEA level was measured every time chemotherapy was administered. Subsequently, a follow-up assessment with CEA assay and abdominal CT was performed when all treatments were completed. Thereafter, follow-up visits were conducted in accordance with NCCN guidelines.
A DRM of at least 2 cm has always been recommended for rectal cancer surgery, whereas a 1-cm DRM is required in cases of low rectal cancer. This study was conducted to investigate whether the safety of rectal cancer surgery could be ensured with a DRM of 1-2 cm. Thus, two cutoff values for DRM length, 1 cm and 2 cm, were used for patient stratification as follows: group 1, DRM < 1 cm; group 2, 1 cm ≤ DRM ≤ 2 cm; and group 3, DRM > 2 cm. Clinical features, overall survival (OS), and local recurrence-free survival (LRFS) were compared among the three groups of patients.
Continuous variables, such as the length of resected margin, age, the duration of follow-up, or time to recurrence, were compared using analysis of variance, whereas categorical variables, such as sex, stage and other pathologic results, death, or local recurrence, were analyzed using the chi-square test. OS and LRFS were compared using the Kaplan-Meier method. The Cox proportional hazard model was used for the adjustment of factors such as age, stage, and lymphatic invasion of tumor, which could influence OS and LRFS. All analyses were performed using the IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA).
There were 131 of men and 87 of women with an average age of 62.2 ± 11.76 years. Preoperative radiotherapy was administered to 55 patients (25.2%). All patients were diagnosed with rectal adenocarcinoma and underwent LAR.
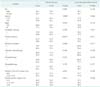
No significant differences were observed in patient demographics such as age and sex. Furthermore, the number of patients receiving pre- and postoperative radiotherapy or adjuvant chemotherapy did not significantly differ among the three groups (P > 0.050) (Table 1). Similarly, no significant intergroup differences in histopathologic results of stage, lymphatic invasion, venous invasion, and perineural invasion were observed (P > 0.050) (Table 1).
The mean DRM length in group 1 (n = 81, 32.1%) was 0.67 ± 0.30 cm, whereas that in groups 2 (n = 66, 30.3%) and 3 (n = 71, 32.6%) was 1.63 ± 0.30 cm and 3.76 ± 1.77 cm, respectively. The mean distance from the anal verge to the tumor in group 1 was 4.88 ± 3.75 cm, whereas that in groups and 3 was 6.53 ± 3.38 cm and 10.52 ± 3.41 cm in each (Table 1).
Eight patients experienced local recurrence in the pelvic cavity and anastomotic site. There were 4 cases of local recurrence in the pelvic cavity, including 1 patient in group 1 and 3 in group 2. Two patients in group 1 and 1 patient in both group 2 and group 3 had recurrence at the anastomotic site. There were no statistically significant intergroup differences (P = 0.769).
The mean follow-up periods were 37.3 ± 26.4 months for group 1, 37.8 ± 30.4 months for group 2, and 36.0 ± 27.4 months for group 3, with no significant intergroup difference (P = 0.927). The Cox proportional hazard model was employed to correct for age, stage, and microscopic lymphatic invasion, which could affect OS or LRFS. During the follow-up period, 31 patients died, including 11 in group 1, 10 in group 2, and 10 in group 3 (P = 0.955). The 5-year survival rates were 78.2%, 78.2%, and 76.8% for patients in groups 1, 2, and 3, respectively (P = 0.913) (Table 2, Fig. 1). The hazard ratios (HRs) estimated by a multivariate analysis of survival rates were 0.7 (95% confidence interval [CI], 0.2-2.0) for group 1 and 0.6 (95% CI, 0.2-1.9) for group 2, with no statistically significant differences (P = 0.660) (Table 3, Fig. 2). The LRFS rates for 5 years were 97.2%, 98.1%, and 98.2% for patients in groups 1, 2, and 3, respectively (P = 0.848) (Table 2, Fig. 1). The HRs were estimated as 1.6 (95% CI, 0.1-24.0) and 1.0 (95% CI, 0.1-18.5) for groups 1 and 2, respectively. No statistically significant differences in LRFS were observed among the three groups (P = 0.890) (Table 3, Fig. 2).
It has been reported that in many rectal cancer patients, intramural spread is observed at the distal part that is at most 1 cm from the tumor [6,16,17,18,19,20,21]. Thus, a clear margin can be secured only when a DRM of at least 1 cm is achieved [1]. Alternatively, APR is often performed when a sufficient DRM cannot be achieved in cases of low rectal cancer, leaving a patient with a lifetime stoma, which has been reported to deteriorate quality of life [22,23,24,25]. In particular, a prospective study by Gervaz et al. [23] reported deterioration in the quality of life of patients undergoing APR. Thus, surgeons need to consider patients' life quality, survival rate, and oncologic safety when choosing a surgical method for low rectal cancer.
As chemoradiation therapy and other therapeutic modalities have remarkably advanced, more recent reports have suggested that oncologic safety might not be negatively affected by a DRM of ≤1 cm. In addition, the improvement of surgical tools, such as the double-stapling anastomotic instrument, has made sphincter-conserving surgery safer; thus, it may be necessary to redefine the indication for APR.
Bujko et al. [6] comparatively analyzed many studies on survival and local recurrence rates according to DRM length and suggested that 'the 1-cm principle' had no clinical basis, as a DRM of ≤1 cm did not affect the recurrence rate at the anastomotic site, local recurrence rate, or survival rate. Furthermore, several studies have indicated that even a DRM of ≤5 mm might not affect local recurrence or survival rates [11,12,14].
Similarly, in this study, DRM length did not result in statistically significant differences in survival rate and rate of recurrence at the anastomotic site, in the pelvic cavity, or in distal organs. Thus, our results also indicated that DRM length might not affect oncologic safety. The OS and LRFS rates were analyzed according to tumor stage. Four deaths were observed among patients with stage I rectal cancer (2 each in groups 2 and 3), which may be statistically significant as the P-value was 0.028. However, it is problematic to assume that such a result was caused by differences in DRM length, as no death was observed among group 1 patients with the shortest margin, whereas those who died had margins of >1 cm (groups 2 and 3 patients).
Meanwhile, several hypotheses have been suggested for local recurrence, e.g., mucosal-based recurrence caused by microscopic intramural spread, recurrence in the perirectal fat or lymph nodes, and tumor cells shedding into the pelvic cavity [8]. As macroscopic radical resection cannot ensure the microscopic clearance of cancer cells, radiotherapy is required before and after surgery. In fact, two patients in our study who experienced local recurrence at the anastomotic site and in the pelvic cavity did not receive radiotherapy (P = 0.094). Moreover, all patients with recurrence, including recurrence in distal organs, did not receive radiotherapy (P = 0.036).
LAR was performed instead of APR in some low rectal cancer cases. Postoperative radiotherapy was indicated after LAR only when the surgeons decided that sphincter-saving resection was possible with more aggressive radiotherapy in patients with shorter resection margins before and after surgery. Such a treatment might be effective in preventing tumor cells from spreading to the muscularis layers or lymph nodes from the perirectal tissues. Previous reports have demonstrated better results with LAR than APR [26,27]. This might explain why group 1 patients seemed to have a slightly higher rate of recurrence in the pelvic cavity, although this was not statistically significant.
Many studies have been conducted to clarify whether oncologic results may be affected by DRM length. Those studies, as well as ours, had limitations due to the randomization of DRM lengths. Furthermore, we did not control for certain variables such as types of chemotherapy regimens, tumor stage, and tumor cell differentiation; this might affect survival rate and chemotherapy selection and inevitably create group bias. As a result, a multivariate analysis of OS and LRFS was performed. In the analysis of OS, 'age' and 'venous invasion on histopathologic examination' were identified as significant variables, although 'DRM length' and 'stage' that directly correlated with survival rate were also included.
The bowel constricts within 10-20 minutes after being removed from a patient, and again after a brief pause. DRM length is defined as the length of the margin of a fresh specimen restored under ex vivo conditions [1,6]. However, surgeons also visibly estimate the length during surgery, and it is worthy of note that in many cases, this estimated length tends to be shorter than that of the specimen. A previous report suggested that the shorter the resection margin, the further this influence was reduced [16].
Another limitation of this study was that histopathologic examination was not conducted properly on the circumferential resection margin in more than half of the enrolled patients. TME was performed in all patients, and those with tumors that tested positive on permanent histopathologic examination were excluded from this study. However, many patients were regretfully not checked for residual cancer at the circumferential resection margin. In this context, recent studies have reported that the local recurrence rate increases when the circumferential resection margin is less than 2 mm [8], suggesting that the missing data on the length of circumferential resection margin and residual cancer might create a bias against our local recurrence rate.
In the present study, DRM length did not statistically correlate with survival and local recurrence rates. In terms of oncologic safety, although it might be imperative to achieve a sufficient resection margin, it is important to consider conservation of the anal sphincter, as this directly influences patients' quality of life. Therefore, when operating on patients with low rectal cancer, surgeons should cautiously decide whether to perform APR and carefully consider adjuvant chemotherapy, combination radiotherapy, and sphincter-conserving surgery.
Figures and Tables
 | Fig. 1Univariate analysis of survival rate: (A) survival rate, (B) local recurrence-free survival rate. No statistically significant differences in 5-year overall survival and local recurrence-free survival were observed among the three groups in the univariate analysis. |
 | Fig. 2Multivariate analysis of survival rates in the three patient groups: (A) Survival rate, (B) local recurrence-free survival rate. No statistically significant differences in 5-year overall survival and local recurrence-free survival were observed among the three groups in the multivariate analysis. |
References
1. Nelson H, Petrelli N, Carlin A, Couture J, Fleshman J, Guillem J, et al. Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst. 2001; 93:583–596.
2. Lim SB, Kim JC. Surgical issues in locally advanced rectal cancer treated by preoperative chemoradiotherapy. J Korean Surg Soc. 2013; 84:1–8.
3. Scott N, Jackson P, al-Jaberi T, Dixon MF, Quirke P, Finan PJ. Total mesorectal excision and local recurrence: a study of tumour spread in the mesorectum distal to rectal cancer. Br J Surg. 1995; 82:1031–1033.
4. Cecil TD, Sexton R, Moran BJ, Heald RJ. Total mesorectal excision results in low local recurrence rates in lymph node-positive rectal cancer. Dis Colon Rectum. 2004; 47:1145–1149.
5. Van Cutsem E, Dicato M, Haustermans K, Arber N, Bosset JF, Cunningham D, et al. The diagnosis and management of rectal cancer: expert discussion and recommendations derived from the 9th World Congress on Gastrointestinal Cancer, Barcelona, 2007. Ann Oncol. 2008; 19:Suppl 6. vi1–vi8.
6. Bujko K, Rutkowski A, Chang GJ, Michalski W, Chmielik E, Kusnierz J. Is the 1-cm rule of distal bowel resection margin in rectal cancer based on clinical evidence? A systematic review. Ann Surg Oncol. 2012; 19:801–808.
7. Kiran RP, Lian L, Lavery IC. Does a subcentimeter distal resection margin adversely influence oncologic outcomes in patients with rectal cancer undergoing restorative proctectomy? Dis Colon Rectum. 2011; 54:157–163.
8. Nash GM, Weiss A, Dasgupta R, Gonen M, Guillem JG, Wong WD. Close distal margin and rectal cancer recurrence after sphincter-preserving rectal resection. Dis Colon Rectum. 2010; 53:1365–1373.
9. Vernava AM 3rd, Moran M, Rothenberger DA, Wong WD. A prospective evaluation of distal margins in carcinoma of the rectum. Surg Gynecol Obstet. 1992; 175:333–336.
10. Karanjia ND, Schache DJ, North WR, Heald RJ. 'Close shave' in anterior resection. Br J Surg. 1990; 77:510–512.
11. Kuvshinoff B, Maghfoor I, Miedema B, Bryer M, Westgate S, Wilkes J, et al. Distal margin requirements after preoperative chemoradiotherapy for distal rectal carcinomas: are < or = 1 cm distal margins sufficient? Ann Surg Oncol. 2001; 8:163–169.
12. Andreola S, Leo E, Belli F, Bonfanti G, Sirizzotti G, Greco P, et al. Adenocarcinoma of the lower third of the rectum surgically treated with a <10-MM distal clearance: preliminary results in 35 N0 patients. Ann Surg Oncol. 2001; 8:611–615.
13. Huh JW, Jung EJ, Park YA, Lee KY, Sohn SK. Sphincter-preserving operations following preoperative chemoradiation: an alternative to abdominoperineal resection for lower rectal cancer? World J Surg. 2008; 32:1116–1123.
14. Rutkowski A, Bujko K, Nowacki MP, Chmielik E, Nasierowska-Guttmejer A, Wojnar A, et al. Distal bowel surgical margin shorter than 1 cm after preoperative radiation for rectal cancer: is it safe? Ann Surg Oncol. 2008; 15:3124–3131.
15. Pricolo VE, Abodeely A, Resnick M. Distal margins in radical resections for rectal cancer after chemoradiation therapy: how short is long enough? Dig Surg. 2010; 27:185–189.
16. Williams NS, Dixon MF, Johnston D. Reappraisal of the 5 centimetre rule of distal excision for carcinoma of the rectum: a study of distal intramural spread and of patients' survival. Br J Surg. 1983; 70:150–154.
17. Madsen PM, Christiansen J. Distal intramural spread of rectal carcinomas. Dis Colon Rectum. 1986; 29:279–282.
18. Shirouzu K, Isomoto H, Kakegawa T. Distal spread of rectal cancer and optimal distal margin of resection for sphincter-preserving surgery. Cancer. 1995; 76:388–392.
19. Mezhir JJ, Smith KD, Fichera A, Hart J, Posner MC, Hurst RD. Presence of distal intramural spread after preoperative combined-modality therapy for adenocarcinoma of the rectum: what is now the appropriate distal resection margin? Surgery. 2005; 138:658–663.
20. Kwok SP, Lau WY, Leung KL, Liew CT, Li AK. Prospective analysis of the distal margin of clearance in anterior resection for rectal carcinoma. Br J Surg. 1996; 83:969–972.
21. Chmielik E, Bujko K, Nasierowska-Guttmejer A, Nowacki MP, Kepka L, Sopylo R, et al. Distal intramural spread of rectal cancer after preoperative radiotherapy: the results of a multicenter randomized clinical study. Int J Radiat Oncol Biol Phys. 2006; 65:182–188.
22. Ross L, Abild-Nielsen AG, Thomsen BL, Karlsen RV, Boesen EH, Johansen C. Quality of life of Danish colorectal cancer patients with and without a stoma. Support Care Cancer. 2007; 15:505–513.
23. Gervaz P, Bucher P, Konrad B, Morel P, Beyeler S, Lataillade L, et al. A Prospective longitudinal evaluation of quality of life after abdominoperineal resection. J Surg Oncol. 2008; 97:14–19.
24. Tsunoda A, Tsunoda Y, Narita K, Watanabe M, Nakao K, Kusano M. Quality of life after low anterior resection and temporary loop ileostomy. Dis Colon Rectum. 2008; 51:218–222.
25. Siassi M, Hohenberger W, Losel F, Weiss M. Quality of life and patient's expectations after closure of a temporary stoma. Int J Colorectal Dis. 2008; 23:1207–1212.
26. Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK. Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978-1997. Arch Surg. 1998; 133:894–899.
27. Wibe A, Rendedal PR, Svensson E, Norstein J, Eide TJ, Myrvold HE, et al. Prognostic significance of the circumferential resection margin following total mesorectal excision for rectal cancer. Br J Surg. 2002; 89:327–334.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download