Abstract
Purpose
The purpose of this study was to analyze the risk factors for delayed graft function (DGF) and determine its impact on the outcomes of deceased donor (DD) kidney transplantation (KT).
Methods
Between January 2000 and December 2011, we performed 195 DD renal transplants. After the exclusion of primary nonfunctional grafts (n = 4), the study recipients were divided into two groups-group I, DGF (n = 31, 16.2%); group II, non-DGF (n = 160, 83.8%). The following variables were compared: donor and recipient characteristics, patient and graft survival, postoperative renal function, acute rejection (AR) episodes, and the rates of surgical and infectious complications.
Results
Donor-related variables that showed significant differences included hypertension (P = 0.042), diabetes (P = 0.025), and prerecovery serum creatinine levels (P < 0.001). However, there were no significant differences in recipient-related factors. One significantly different transplant-related factor was positive panel reactive antibody (PRA > 20%, P = 0.008). On multivariate analysis, only the prerecovery serum creatinine level (P < 0.001; hazard ratio [HR], 1.814) was an independent risk factor for the development of DGF. A Cox multivariate analysis of risk factors for graft survival identified these independent risk factors for graft survival: nephron mass (donor kidney weight to recipient body weight ratio) index (P = 0.026; HR, 2.328), CMV infection (P = 0.038; HR, 0.114), and AR episode (P = 0.038; HR, 0.166).
Delayed graft function (DGF), defined as the need for dialysis within the first week posttransplantation, occurs in approximately 25% of deceased donor (DD) renal transplantation cases [123]. DGF is a well-known complication associated with increased risk of acute rejection (AR) and poor long-term graft survival, but the impact of DGF on posttransplant outcomes is not yet entirely clear. Recent studies provide conflicting conclusions regarding the impact of DGF on the outcome of renal transplantation [4567]. The purpose of this study was to analyze risk factors for DGF and determine its impact on the outcomes of DD kidney transplantation (KT).
In this retrospective study, we reviewed the medical records and electronic transplant registry of KT recipients at Seoul St. Mary's Hospital, The Catholic University of Korea, from January 2000 to December 2011. During that period, 786 KTs were performed. Specific exclusion criteria included pediatric recipients (<18 years of age), simultaneous kidney-pancreas transplant recipients, all living donor KT, and primary nonfunctional grafts. A consecutive series of 191 DD kidney transplants were studied. DGF was defined as the need for dialysis within 1 week postrenal transplantation [8]. The study recipients were divided into two groups-group I, DGF (n = 31, 16.2%); group II, non-DGF (n = 160, 83.8%).
The anti-interleukin 2 receptor antagonist (basiliximab) was administered intravenously for induction therapy. Cyclosporine or FK 506, mycophenolate mofetil or mycophenolate sodium, and steroids were used as primary immunosuppressive agents. The following variables were compared: donor and recipient characteristics, patient and graft survival, postoperative renal function (mean creatinine and Modification of diet in renal disease [MDRD]-Glomerular Filtration Rates [GFR] levels at 1 and 6 months, and 1-, 3-, 5-, and 7-year posttransplant), AR episodes, and the rates of surgical and infectious complications. Renal allograft loss was defined as resumption of ongoing dialysis. Patient deaths with functioning grafts were censored. Cytomegalovirus (CMV) infection was defined based on a positive real-time PCR test.
No specific DD upper age limit was excluded from consideration, and these series included 12 transplants from DD ≥ 60 years old. All DDs older than 60 years and DDs 50 to 59 years of age that met two of the following criteria: (1) history of hypertension, (2) cerebrovascular accident as a cause of brain death, (3) final preprocurement serum creatinine (SCr) level > 1.5 mg/dL were classified as expanded criteria donors (ECDs) based on United Network for Organ Sharing definitions. At the time of transplantation, patients were selected on the basis of blood type compatibility, waiting time, HLA matching, and a negative cross-match in accordance with Korean Network for Organ Sharing guidelines [9].
The unpaired t-test for continuous variables and the chi-square test for categorical variables were used to compare data between the two groups. All data were expressed as the mean ± standard deviation. The Kaplan-Meier method was used to compare patients and graft survival rates between the two groups. Data were censored at the time of death or at the last available follow-up. Graft survival was also evaluated by multivariate analyses according to Cox regression with an entered-fashion of variables. Statistical significance was defined as P < 0.05. All statistical analyses were carried out with PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA).
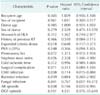
During that period, we performed 195 DD renal transplants on adult recipients. We excluded primary nonfunction grafts (n = 4), the overall prevalence of DGF was 16.2% (n = 31). Of the 191 KTs, 51.8% were male recipients and 65.6% received a kidney from a male donor. The average recipient age was 45.1 ± 9.6 years, and the mean follow-up duration was 43.7 ± 34.3 months. Donors and Recipients characteristics are provided in Table 1.
DGF recipients had a higher proportion of panel reactive antibody (PRA > 20%) (P = 0.008), with a low number of 0% PRA (P = 0.004), but other baseline characteristics (age, gender, body mass index, cause of end-stage renal disease, type of renal replacement therapy, number of antigen mismatches, history of pregnancy and transfusions) were not significantly different between the two recipient groups.
In the multivariate analysis, only the prerecovery SCr level (P < 0.001; HR, 1.814) was an independent risk factor for the development of DGF (Table 2).
The SCr levels, mean MDRD GFR levels, and incidence of AR episodes were compared between the two groups as a measure of graft function. The SCr levels and mean MDRD GFR level at 7 days, 1 month, and 6 months after transplantation were significantly lower in the non-DGF group but did not differ significantly after 12 months (Table 3). The incidence of an AR episode within 3 months posttransplant was 32.3% in the DGF group and 16.3% in the non-DGF group. This difference was significant (P = 0.037).
The incidence of CMV infection was significantly higher in the DGF group (77.8% in the DGF vs. 55.6% in the non-DGF, P = 0.032). Other infections did not differ remarkably between the two groups. When analyzing surgical complications types, the majority of complications in both groups were early (within 30 days after the KT) operative complications that were vascular, urologic, and wound-related (Table 4). The overall surgical complication rate between the groups was not different (P = 0.606).
Graft survival rates at 1 year, 3 years, 5 years, and 10 years posttransplantation were 83.7%, 79.1%, 79.1%, and 79.1%, respectively, in the DGF group, and 97.3%, 92.2%, 90.6%, and 81.5%, respectively, in the non-DGF group. Patient survival rates at 1 year, 3 years, 5 years, and 10 years posttransplantation were 96.7%, 96.7%, 96.7%, and 77.3%, respectively, in the DGF group, and 98.1%, 96.3%, 96.3%, and 90.9%, respectively, in the non-DGF group. There was a significant difference between the two groups in graft survival (P = 0.020) but no difference between the two groups in patient survival (P = 0.502). The overall cumulative grafts and patient survival rates in these groups are shown as Kaplan-Meier curves in Fig. 1.
Using Cox logistic regression analysis, graft survival was clearly associated with nephron mass index (donor kidney to recipient body weight; Kw/Rw) at the time of transplantation, CMV infection, and AR episodes (Table 5).
DGF is a common immediate postoperative complication following deceased-donor KT. DGF is primarily a result of ischemic-reperfusion injury to the graft that is characterized by postischemic acute tubular necrosis and interstitial inflammation [10]. Ischemic injury to allografts is the sum of possible transient warm ischemic intervals before or during removal from the donor and cold ischemia associated with preservation and storage. The prolonged exposure of the donor kidney to warm and/or cold ischemia increases the incidence of DGF and leads to a programmed process within the kidney, which may lead to chronic and progressive lesions [1112].
In this study, the incidence of DGF was 16.2%, which was lower compared to what has been reported in recent studies [41314]. In one US study, the reported incidence of DGF in DDs increased over time despite progress in AR treatment, translating into a 40% decrease in long-term graft survival. Between 1985 and 1992, the rate of DGF in US scientific registries was 14.7%, but the incidence rose to 23% in 1998-2004 [215]. In the most recent reports, DGF occurred in all 2,409 US patients who underwent transplantation in 2008 (21.3%) [16]. In another recent study in Korea, the incidence of DGF was 17.6%, which was relatively similar to ours [7]. Two reasons for the low DGF incidence in Korea could be the short cold ischemic time (CIT), with a mean CIT of 4.05 ± 2.18 hours in the present study, and the population of Korea, which is comparatively homogeneous in race and ethnicity. According to the findings of previous studies, the risk factors of DGF were high levels of PRA, retransplantation, recipient and donor age, and CIT [21718]. Despite the importance of CIT as a risk factor for DGF, the CIT was not different between the two groups in this study. The short ischemic time at our center is due to the fact that many of our recipients received kidneys from DDs managed in our hospital without the need for organ transport.
The purpose of this study was to analyze the risk factors of DGF and determine its impact on the outcomes of DD KT. We confirmed that the DGF rate correlates with the prevalence of diabetes mellitus in donors, ECD, a high level of PRA in the recipients (PRA > 20%), and prerecovery SCr level. However, using multivariate analysis, the preretrieval SCr (P < 0.001) was the only significant risk factor for DGF. It was considered that a short CIT and a homogeneity of races and ethnicities could offset the risk of other donors, recipients, and immunologic factors for DGF.
This study evaluated the effect of DGF on clinical outcomes, long-term graft function, and survival. Some earlier studies suggested that the degree of DGF may be associated with worse graft outcomes [5619]. Moreira et al. [6] reported that there was initially a significant difference regarding SCr, but this disappeared at 10 years. In this study, the SCr levels and mean MDRD GFR levels at 7 days, 1 month, and 6 months after transplantation were significantly lower in the non-DGF group but did not significantly differ 1 year later. This effect was due to not only an adaptive ability, but also the removal from the data set of DGF recipients with a high creatinine level and grafts that failed beyond 1 year.
In addition to the SCr and MDRD GFR of graft function, the effect of DGF on long-term graft survival is more debatable. An earlier study reported that DGF was an independent risk factor for AR episodes, but had no independent effect on graft survival [17]. These data are similar to ours. In our study, graft survival rates at 1-, 5-, and 10-year posttransplantation were 83.7%, 79.1%, and 79.1%, respectively, in the DGF group, and 97.3%, 90.6%, and 81.5%, respectively, in the non-DGF group. There was a significant difference between the two groups in graft survival (P = 0.020). It was considered that a higher incidence of an AR episode impacted on the long-term graft survival since AR episode was a clear risk factor for graft survival in our study, although rejection-free graft survival was not significantly different between two groups.
However, on multivariate logistic regression analysis, DGF was not an independent risk factor of long-term graft survival. Based on our results, (1) there was significant difference in graft function (SCr and MDRD GFR) between the two groups (DGF vs. non-DGF), but it disappeared at 1-year posttransplantation, and (2) although there was a significant difference in graft survival between the two groups, DGF was not an independent risk factor for long-term graft failure. This is attributable to the fact that although DGF may affect early graft function, after recovering from DGF, it no longer becomes a significant independent risk factor of graft survival.
Our results are subject to the limitations inherent in observational and small population data in single center study. In addition, there are many combinations between transplantation factors that influence clinical outcomes but are not recognized in our study. Lastly, potential issues relating to the determination of AR, CIT, and graft loss include missing or incomplete data, sampling and technique errors, and subjective interpretation.
Figures and Tables
Fig. 1
Graft (A, P = 0.020) and patient survival (B, P = 0.502) in both groups. DGF, delayed graft function.

Table 1
Characteristics of study population according to delayed graft function (DGF)

Values are presented as mean ± SD or number (%).
CVA, cerebrovascular accident; HTN, hypertension; DM, diabetes; Scr, serum creatinine; ICU, intensive care unit; ESRD, end-stage renal disease; GN, glomerulonephritis; PN, pyelonephritis; PCKD, adult polycystic kidney disease; RRT, renal replacement therapy; HD, hemodialysis; PD, peritoneal dialysis; KT, kidney transplantation; HLA, human leukocyte antigen; PRA, panel reactive antibody; SD, standard deviation; IQR, interquartile range.
References
1. Koning OH, Ploeg RJ, van Bockel JH, Groenewegen M, van der Woude FJ, Persijn GG, et al. European Multicenter Study Group. Risk factors for delayed graft function in cadaveric kidney transplantation: a prospective study of renal function and graft survival after preservation with University of Wisconsin solution in multiorgan donors. Transplantation. 1997; 63:1620–1628.
2. Ojo AO, Wolfe RA, Held PJ, Port FK, Schmouder RL. Delayed graft function: risk factors and implications for renal allograft survival. Transplantation. 1997; 63:968–974.
3. Yarlagadda SG, Coca SG, Garg AX, Doshi M, Poggio E, Marcus RJ, et al. Marked variation in the definition and diagnosis of delayed graft function: a systematic review. Nephrol Dial Transplant. 2008; 23:2995–3003.
4. Miglinas M, Supranaviciene L, Mateikaite K, Skebas K, Kubiliene A. Delayed graft function: risk factors and the effects of early function and graft survival. Transplant Proc. 2013; 45:1363–1367.
5. Grosso G, Corona D, Mistretta A, Zerbo D, Sinagra N, Giaquinta A, et al. Delayed graft function and long-term outcome in kidney transplantation. Transplant Proc. 2012; 44:1879–1883.
6. Moreira P, Sa H, Figueiredo A, Mota A. Delayed renal graft function: risk factors and impact on the outcome of transplantation. Transplant Proc. 2011; 43:100–105.
7. Jung GO, Yoon MR, Kim SJ, Sin MJ, Kim EY, Moon JI, et al. The risk factors of delayed graft function and comparison of clinical outcomes after deceased donor kidney transplantation: single-center study. Transplant Proc. 2010; 42:705–709.
8. Perico N, Cattaneo D, Sayegh MH, Remuzzi G. Delayed graft function in kidney transplantation. Lancet. 2004; 364:1814–1827.
9. Kim MS, Kim SI, Kim YS. Current status of deceased donor organ recovery and sharing in Korea. J Korean Med Assoc. 2008; 51:685–691.
10. Siedlecki A, Irish W, Brennan DC. Delayed graft function in the kidney transplant. Am J Transplant. 2011; 11:2279–2296.
11. Schroppel B, Legendre C. Delayed kidney graft function: from mechanism to translation. Kidney Int. 2014; 86:251–258.
12. Menke J, Sollinger D, Schamberger B, Heemann U, Lutz J. The effect of ischemia/reperfusion on the kidney graft. Curr Opin Organ Transplant. 2014; 19:395–400.
13. Ditonno P, Impedovo SV, Palazzo S, Bettocchi C, Gesualdo L, Grandaliano G, et al. Effects of ischemia-reperfusion injury in kidney transplantation: risk factors and early and long-term outcomes in a single center. Transplant Proc. 2013; 45:2641–2644.
14. Premasathian N, Avihingsanon Y, Ingsathit A, Pongskul C, Jittiganont S, Sumethkul V. Risk factors and outcome of delayed graft function after cadaveric kidney transplantation: a report from the Thai Transplant Registry. Transplant Proc. 2010; 42:4017–4020.
15. Tapiawala SN, Tinckam KJ, Cardella CJ, Schiff J, Cattran DC, Cole EH, et al. Delayed graft function and the risk for death with a functioning graft. J Am Soc Nephrol. 2010; 21:153–161.
16. Ommen ES, LaPointe Rudow D, Medapalli RK, Schroppel B, Murphy B. When good intentions are not enough: obtaining follow-up data in living kidney donors. Am J Transplant. 2011; 11:2575–2581.
17. Boom H, Mallat MJ, de Fijter JW, Zwinderman AH, Paul LC. Delayed graft function influences renal function, but not survival. Kidney Int. 2000; 58:859–866.
18. Humar A, Ramcharan T, Kandaswamy R, Gillingham K, Payne WD, Matas AJ. Risk factors for slow graft function after kidney transplants: a multivariate analysis. Clin Transplant. 2002; 16:425–429.
19. Giral-Classe M, Hourmant M, Cantarovich D, Dantal J, Blancho G, Daguin P, et al. Delayed graft function of more than six days strongly decreases long-term survival of transplanted kidneys. Kidney Int. 1998; 54:972–978.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download