Abstract
Purpose
Methods
Results
Conclusion
Figures and Tables
Fig. 1
Arterial phase in contrast-enhanced abdominal CT of representative case who received DP-CAR. (A) The common hepatic artery, spleneic artery, and celiac artery (CA) are involved with low-density mass in body and tail of pancreas (6 cm × 4 cm), (B-D) Proper hepatic artery (PHA), gastroduodenal artery (GDA), superior mesenteric artery (SMA), superior mesentric vein, and portal vein were spared. DP-CAR, distal pancreatectomy with en bloc celiac axis resection; PHA, proper hepatic artery; CA, celiac axis.

Fig. 2
Schematic showing distal pancreatectomy with en bloc celiac axis resection. (A) White dotted line indicates dissection plane, (B) shematic drawing collateral arterial circulation via pancreaticoduodenal arcades from superior mesenteric artery (SMA) after DP-CAR. DP-CAR, distal pancreatectomy with en bloc celiac axis resection; CA, celiac axis; CHA, common hepatic artery; SA, splenic artery; LGA, left gastric artery; PHA, proper hepatic artery; RGA, right gastric artery; GDA, gastroduodenal artery; RGEA, right gastroepiploic artery; IPDA, inferior pancreaticoduodenal artery; PV, portal vein; SV, splenic vein; SMV, superior mesenteric vein; IMV, inferior mesenteric vein.

Fig. 3
Intraoperative view after completion of DP-CAR. The cut end of celiac axis is shown (white circle). (A) CHA was clearly divided with sufficient tumor free margin. The cut end of common hepatic artery is shown (Forcep). (B) The body and tail of the pancreas and spleen were dissected free from the left adrenal gland and Gerota's fasica. The left renal vein and SMA were exposed. DP-CAR, distal pancreatectomy with en bloc celiac axis resection; CHA, common hepatic artery; SMV, superior mesenteric vein; SMA, superior mesenteric artery.

Fig. 4
Comparision of the survival curves according to different surgical type. There was no significant difference in the survival rate between DP-CAR and DP groups (p=0.681). DP-CAR, distal pancreatectomy with en bloc celiac axis resection; DP, distal pancratectomy; NR, no resection.
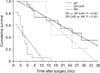
Table 2
Preoperative imaging findings and postoperative pathologic findings for patients who underwent DP-CAR

DP-CAR, distal pancreatectomy with en bloc celiac axis resection; LVI, lymphovascular invasion; PNI, perineural invasion; CA, celiac axis; SA, splenic artery; LGA, left gastric artery; SV, splenic vein; GB, gallbladder, SMA, superior mesenteric artery; LAG, left adrenal gland; PV, portal vein; LRV, left renal vein; SMV, superior mesenteric vein; CHA, common hepatic artery.
Table 3
Morbidity and mortality profiles of 31 patients in DP group and 7 patients in the DP-CAR group

Values are presented as median (range) or number (%) unless otherwise indicated.
DP, distal pancratectomy, DP-CAR, distal pancreatectomy with en bloc celiac axis resection; EBS, estimated blool loss; PRBC, packed red blood cell; U, unit.
a)Postoperative pancreatic fistula, delayed gastric emptying, and postpancreatectomy hemorrhage are defined according to the International Study Group of Pancreatic Surgeons.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download