Abstract
Purpose
The use of hepatitis B core antibody (HBcAb)-positive grafts is increasing, especially where hepatitis B is endemic. However, this remains controversial because of the risk of development of de novo HBV infection.
Methods
We collected information obtained between January 2000 and December 2012 and retrospectively analyzed data on 187 HBsAg-negative donors and recipients were analyzed retrospectively. De novo HBV infection was defined as development of HBsAg positivity with or without detection of HBV DNA.
Results
Forty patients (21.4%) received HBcAb-positive grafts. Survival rate did not differ by donor HBcAb status (P = 0.466). De novo HBV infection occurred in five patients (12.5%) who were not treated with anti-HBV prophylaxis, and was significantly more prevalent in hepatitis B surface antibody (HBsAb)- and HBcAb-negative than HBsAb- and HBcAb-positive recipients (50% vs. 4.2%, P = 0.049). All patients except one were treated with entecavir with/without antihepatitis B immunoglobulin and four were negative in terms of HBV DNA seroconversion. No patient died.
It is difficult to find liver donors, and use of marginal donors is increasing [1]. Hepatitis B core antibody (HBcAb)-positive donors are considered marginal, but are often used particularly in Asia, where hepatitis B is endemic [2]. However, the use of HBcAb-positive grafts to treat HBsAg-negative recipients remains controversial, because of the possibility of development of de novo hepatitis B infection [3].
HBcAb-positive grafts are generally used to treat patients already infected with hepatitis B because antiviral treatment would be given after liver transplantation (LT) [4]. However, several reports have shown that outcomes do not differ between hepatitis B surface antibody (HBsAb)- and HBcAb-negative recipients if anti-HBV prophylaxis is prescribed [56]. Hepatitis B immunoglobulin (HBIG), and antiviral agents are generally recommended. However, some authors are of the view that antiviral agent monotherapy is adequate; HBIG is expensive and the use thereof is associated with side-effects [7].
It is becoming impossible to unconditionally refuse to use HBcAb-positive grafts, especially in HBV-endemic areas where many potential donors are HBcAb-positive. It is impractical to offer anti-HBV prophylaxis or vaccination to all recipients who will receive grafts from HBcAb-positive donors. Thus, in the present study, we evaluated the risk of development of de novo hepatitis B infection in the absence of HBV prophylaxis, and the outcomes of anti-HBV treatment in recurred hepatitis B patients.
We retrospectively analyzed the medical records of 191 HBsAg-negative recipients, and their donors, who underwent LT at our hospital between January 2000 and December 2012. We excluded 4 patients who died within 1 month of LT. The study was approved by the Institutional Review Board of Seoul St. Mary's Hospital and was conducted according to the guidelines of the Declaration of Helsinki. Mean donor age was 34.26 ± 11.50 years and 63.6% were males. Of all donors, 40 (21.4%) were HBcAb-positive. Mean recipient age was 50.10 ± 11.21 years and 57.8% were male. The most common indication for LT was alcoholic liver cirrhosis (39.0%). The living donor liver transplantation was 66.3%. The proportions of recipients who were HBsAb- and HBcAb-positive were 66.3% and 71.7%, respectively. De novo HBV virus infection was defined as development of serum HBsAg positivity with or without detection of HBV DNA. Donors and recipients were divided into two groups by donor HBcAb status: HBcAb-positive and -negative. We evaluated the characteristics of HBcAb-positive donor grafts, the incidence of and risk factors for de novo hepatitis B infection, and clinical outcomes after treatment of such infections. The mean follow-up duration after LT was 46.9 ± 34.4 months.
Anti-HBV prophylaxis was not given, and the levels of hepatitis B viral markers including serum HBsAg, HBsAb, and HBcAb; and hepatitis C antibody level, were routinely checked prior to surgery, as were antihuman immunodeficiency virus antibody levels, and cytomegalovirus titer and antiviral antibody levels. All patients were managed using a defined protocol. Hepatitis B viral markers including serum HBsAg, HBsAb, HBeAg, and hepatitis B envelop antibody were measured, using electrochemiluminescence immunoassays, at every follow-up visit to our outpatient Department. Such visits were made every month during the first year after surgery; every 2 months from years 2-5 after surgery; and every 3 months thereafter. Serum HBV DNA levels were measured every 6 months after surgery using the branched DNA assay (Siemens Healthcare Diagnostics, Eschborn, Germany; lower limit of detection: 2,000 copies/mL) prior to May 2006 and, thereafter, a highly sensitive real-time PCR assay (Abbott, Chicago, IL, USA; lower limit of detection: 34 copies/mL). If de novo hepatitis B infection developed, patients were treated with antiviral agents such as entecavir, with or without HBIG. Liver function tests (AST and ALT levels), the hepatitis B profile, HBV DNA level, and evaluation of drug-induced HBV mutations, were performed after treatment to evaluate the efficacy of treatment.
Means and standard deviations of numerical variables are presented. Between-group differences in the means of continuous variables were compared using Student t-test, and differences in categorical variables employing the chi-square test. The Kaplan-Meier method was used to calculate disease-free survival and overall survival rates. Survival time distributions were compared using the log-rank test. A P-value of <0.05 was considered to reflect statistical significance.
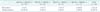
We studied 187 recipients. Of these, 40 (21.4%) received grafts from HBcAb-positive donors, and 24 (60%) were HBsAb- and HBcAb-positive whereas 4 (10%) were doubly negative. Of recipients who received grafts from HBcAb-negative donors (n = 147, 78.6%), 74 (50.4%) were HBsAb- and HBcAb-positive, and 23 (15.7%) doubly negative. The mean ages of HBcAb-positive and -negative donors were 36.68 ± 10.69 and 32.71 ± 11.05 years, respectively, thus significantly greater in the former group (P = 0.007). Significantly more HBcAb-positive than -negative donors were HBsAb-positive (90.0% vs. 71.4%, P = 0.006). None of MELD score, HBcAb or HBsAb status, or any operative parameter including operative time and transfusion volume differed among the two recipient groups. However, the rate of development of de novo hepatitis B infection was significantly higher in recipients receiving graft from HBcAb-positive donors (12.5% vs. 0.7%, P = 0.002) (Table 1). The mean survival periods after transplantation were 120.37 ± 3.57 and 117.73 ± 5.05 months in those whose donors were HBcAb-positive and -negative, respectively (P = 0.121). Only one death occurred (15 months after LT) in the former group. The 5-year survival rate of that group was 97.5%. The 1-, 3-, and 5-year survival rates of the other group were 96.9%, 94.5%, and 89.7%. No significant between-group difference was apparent (P = 0.235) (Fig. 1).
Five of the 187 patients (2.7%) developed de novo hepatitis B infections, of whom 5 were among the 40 (12.5%) who received grafts from HBcAb-positive donors. One patient developed de novo infection 119 months after surgery whereas the others all became infected within 3 years after LT (83.3%); 3 within 1 year. We subdivided recipients by their antibody status: 2 of 30 and 3 of 10 (6.7% and 30%) HBcAb-positive and -negative recipients, respectively, developed de novo infections (P = 0.096). From the perspective of recipient HBsAb status, 2 of 30 and 3 of 10 (6.7% and 30%) HBsAb-positive and -negative patients, respectively, developed de novo infections (P = 0.096). Of recipients who received grafts from HBcAb-positive donors, the rates of de novo infections were 50.0% (2 of 4) in those who were both HBsAb- and HBcAb-negative, and 4.2% (1 of 17) in those who were both HBsAb- and HBcAb-positive (P = 0.049) (Table 2). We sought factors associated with development of de novo hepatitis B infections in recipient of HBcAb-positive donor graft. More HBcAb- or HBsAb-positive patients did not than did experience recurrent infections (80.0% vs. 40.0%), but this difference was not significant (P = 0.096). Recipient age was significantly greater in the former group (P = 0.049). The mean survival durations were 40.19 ± 32.37 and 66.4 ± 46.75 months in the noninfected and infected groups; the figures did not differ significantly (P = 0.121) (Table 3).
All five patients who developed de novo hepatitis B infections were HBsAb-positive after transplantation but -negative at the times of recurrence, at which times all patients were HBsAg-positive, five HBV DNA-positive, and three HBeAg-positive. At recurrence, two patients (No. 3 and 4) had elevated ALT levels. Four patients were treated with an antiviral agent with or without HBIG. One patient (No. 1) refused treatment. Two patients were treated with both HBIG and entecavir, and two with entecavir only. The mean treatment period was 27.8 months (range, 5-71 months). Serum ALT levels returned to normal in all treated patients and, of the four HBV DNA-positive patients, three became DNA-negative. All patients remained HBsAb-negative, but HBsAg continued to be detected in all. No mortality or complication was noted in any of the five patients (Table 4).
Organ shortage is a major problem when LT is contemplated, and it is imperative to expand the donor pool. HBcAb-positive donors have not been preferred, particularly for recipients who do not have HBV infections. Many reports have suggested that de novo hepatitis B infections commonly develop after LT using HBcAb-positive grafts, especially in patients with no prior exposure to HBV. Overall and graft survival were reduced [8]. However, recent reports suggest that use of HBcAb-positive grafts may not be independently associated with poor outcomes. In HBV-endemic areas such as ours, it is necessary to carefully define the risk factors associated with use of HBcAb-positive donor, to develop safe treatment strategies. In the present study, 21.4% of donors were HBcAb-positive. Thus, the prevalence of such donors was much greater than that in areas where HBV is not endemic (4.75%-7%) [910]. The 5-year survival rate of recipients of HBcAb-positive graft was 97.5%, and 89.7% in those who received HBcAb-negative graft (P = 0.235). These figures are in line with those of previous studies, suggesting that survival did not differ significantly by donor HBcAb status [2]. Liver grafts from HBcAb-positive donors can transmit HBV to HBsAg-naïve recipients and occult HBV infection may be reactivated by posttransplantation immunosuppression in such patients [211]. The prevalence rates of de novo hepatitis B infections arising after transplantation varied among studies, being 18%-78% [21112] if no anti-HBV prophylaxis was prescribed, in either endemic or nonendemic areas. In the present study, the rate of de novo hepatitis B infection was 12.5% in the absence of prophylaxis, thus significantly lower than in previous studies.
We divided recipients who received HBcAb-positive grafts by HBV antibody status and analyzed de novo hepatitis B infection rates. Patients who were both HBcAb- and HBsAb-positive exhibited the lowest recurrence rate and those who were doubly negative the highest. Skagen et al. [12], in a systemic review, found that the recurrence rates of patients who were HBsAb-positive, HBcAb-positive, and doubly positive were 18%, 14%, and 4%, respectively, similar to what we found. Therefore, patients experiencing recurrence tend to have less HBsAb and HBcAb than do others (P = 0.096). The data strongly suggest that HBcAb and HBsAb exert protective effects, as has also been suggested in previous studies [12]. Also, patients who are HBcAb- and HBsAb-negative should receive anti-HBV prophylaxis. In the present study, all patients with recurrent infections, except for one, became infected within 36 months of surgery, strongly suggesting that short-term follow-up after LT is essential.
Some reports have described the successful use of antiviral agents and/or HBIG to treat patients with de novo infections [1013] and, recently, it has been suggested that antiviral agent monotherapy is adequate [7]. Five of our 6 patients received entecavir, with or without HBIG. Only two of the five patients thus treated had elevated ALT levels at the time of development of infection; these levels became normal after treatment. It is interesting that all of these patients were HBsAb-positive after surgery but HBsAb-negative at the time of recurrence and even after treatment. No patient died or developed morbidity. Our data are comparable to those of previous studies; no mortality or morbidity was associated with de novo infection [1013].
The present study had several limitations. This was not a controlled prospective work, being retrospective in nature, Follow-up and treatment strategies varied among patients. The mean follow-up duration was only 46.9 months; this is too short to evaluate the overall effect of HBcAb-positive grafting. Our small number of patients limits the statistical power afforded by our data. Large, prospective, multicenter studies with longterm follow-up are required.
In conclusion, HBcAb-positive grafts could be safely used to treat patients negative in terms of HBsAg status. The survival of such patients was not compromised. Patients lacking HBsAb or HBcAb were at high risk of de novo hepatitis B infection after LT. Such patients should pay attention to the development of de novo hepatitis B. It is possible to manage de novo hepatitis B infections well and severe morbidity can be avoided.
Figures and Tables
Table 2
Incidence of de novo hepatitis B infection by recipient antibody status in patients receiving HBcAb-positive graft
References
1. Montalti R, Nardo B, Bertelli R, Beltempo P, Puviani L, Vivarelli M, et al. Donor pool expansion in liver transplantation. Transplant Proc. 2004; 36:520–522.
2. Prieto M, Gomez MD, Berenguer M, Cordoba J, Rayon JM, Pastor M, et al. De novo hepatitis B after liver transplantation from hepatitis B core antibody-positive donors in an area with high prevalence of anti-HBc positivity in the donor population. Liver Transpl. 2001; 7:51–58.
3. Roche B, Samuel D, Gigou M, Feray C, Virot V, Schmets L, et al. De novo and apparent de novo hepatitis B virus infection after liver transplantation. J Hepatol. 1997; 26:517–526.
4. Angelico M, Nardi A, Marianelli T, Caccamo L, Romagnoli R, Tisone G, et al. Hepatitis B-core antibody positive donors in liver transplantation and their impact on graft survival: evidence from the Liver Match cohort study. J Hepatol. 2013; 58:715–723.
5. Celebi Kobak A, Karasu Z, Kilic M, Ozacar T, Tekin F, Gunsar F, et al. Living donor liver transplantation from hepatitis B core antibody positive donors. Transplant Proc. 2007; 39:1488–1490.
6. Hwang S, Moon DB, Lee SG, Park KM, Kim KH, Ahn CS, et al. Safety of anti-hepatitis B core antibody-positive donors for living-donor liver transplantation. Transplantation. 2003; 75:3 Suppl. S45–S48.
7. Chang MS, Olsen SK, Pichardo EM, Stiles JB, Rosenthal-Cogan L, Brubaker WD, et al. Prevention of de novo hepatitis B in recipients of core antibody-positive livers with lamivudine and other nucleos(t)ides: a 12-year experience. Transplantation. 2013; 95:960–965.
8. Douglas DD, Rakela J, Wright TL, Krom RA, Wiesner RH. The clinical course of transplantation-associated de novo hepatitis B infection in the liver transplant recipient. Liver Transpl Surg. 1997; 3:105–111.
9. Villamil I, Gonzalez-Quintela A, Aguilera A, Tome S, Otero E, Castroagudin FJ, et al. Truly de novo hepatitis B after liver transplantation. Am J Gastroenterol. 2004; 99:767–768.
10. Brock GN, Mostajabi F, Ferguson N, Carrubba CJ, Eng M, Buell JF, et al. Prophylaxis against de novo hepatitis B for liver transplantation utilizing hep B core (+) donors: does hepatitis B immunoglobulin provide a survival advantage? Transpl Int. 2011; 24:570–581.
11. Douglas DD, Rakela J, Taswell HF, Krom RA, Wiesner RH. Hepatitis B virus replication patterns after orthotopic liver transplantation: de novo versus recurrent infection. Transplant Proc. 1993; 25:1755–1757.
12. Skagen CL, Jou JH, Said A. Risk of de novo hepatitis in liver recipients from hepatitis-B core antibody-positive grafts: a systematic analysis. Clin Transplant. 2011; 25:E243–E249.
13. Dodson SF. Prevention of de novo hepatitis B infection after liver transplantation with allografts from hepatitis B core antibody positive donors. Clin Transplant. 2000; 14:Suppl 2. 20–24.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download