Abstract
Purpose
Management of appendicitis in children has always been an issue in pediatric surgery. Both diagnostic methods and treatment vary significantly among medical centers, and little consensus exists in many aspects of the care for patients with appendicitis. Here, we assessed the value of drain insertion after appendectomy in children.
Methods
This study is a retrospective review of pediatric patients who underwent appendectomy for perforated appendicitis at a tertiary medical center between 2003 and 2012. Patients who had a peritoneal drain inserted after appendectomy were compared with patients without drains regarding preoperative features and postoperative outcomes. Statistical analyses included a 2-tailed Student t-test and a chi-square or Fisher exact test.
Results
In total, 958 patients were reviewed. Of 342 patients with perforated appendicitis, 108 (31.6%) had Jackson-Pratt (JP) drains inserted. The JP group had a longer hospital stay compared with the non-JP group (6.38 ± 3.59 days vs. 3.87 ± 2.38 days, P < 0.001). The JP group also had higher complication rates (22.2% vs. 6.8%, P = 0.003), including the formation of intra-abdominal abscesses.
Acute appendicitis is one of the most common causes of surgical abdomen in children, accounting for more than 20% of visits to the Emergency Department for abdominal pain. Perforated appendicitis is most common in younger children, with incidence rates as high as 66% in those under the age of 5 years [1]. Perforation is commonly associated with abscess formation before and after appendectomy. Perforated appendicitis may be treated with antibiotics alone, without the need for percutaneous drainage [2,3]. In a prospective randomized trial, St. Peter et al. [4] found that there is no advantage to the irrigation of the peritoneal cavity compared with suction alone during laparoscopic appendectomy in children.
Similarly, the use of drains in abdominal surgery remains a controversial subject. Indications for abdominal drainage after appendectomy for perforated appendicitis may include the presence of necrotic or infected tissue, doubtful hemostasis, and insecure closure of the stump. However, various authors have presented uncertainties regarding peritoneal drains [5,6]. The majority of reports evaluating the effects of peritoneal drainage conclude that abandoning the drains resulted in a decrease in both wound infections and intra-abdominal abscesses. Prophylactic drainage requires caution because drains seem to cause more problems than they prevent [7].
The diagnosis-related groups (DRG) system has recently been incorporated in South Korea for certain diseases, including appendicitis, for which a cost-effective treatment guideline can be useful. However, definitive evidence is lacking for the development of such guidelines. "Standardized" clinical practice protocols that have been reported in the past certainly seem to be outdated [8,9], and a new evidence-based guideline is required. Traditional concepts, unsupported by scientific data, have determined the use of surgical drainage. A survey of pediatric surgeons in North America revealed that 51% of surgeons still use peritoneal drains during appendectomy if an abscess is found [10]. In this study, we assessed the value of peritoneal drain insertion after appendectomy in children.
A retrospective review was conducted at Seoul National University Bundang Hospital, a tertiary medical center and the leading referral hospital in the southeast of Seoul, South Korea. All the children under 18 years old who were diagnosed with acute appendicitis and underwent appendectomy between March 2003 and September 2012 were included in this study. Electronic medical records were reviewed for each patient. The following data were gathered: demographics, initial physical findings, and laboratory and radiological results. The diagnostic imaging methods included either ultrasonography or computed tomography. The Alvarado score [11] was calculated for all the patients. The type of operation, the findings of the appendix during the operation, the pathology report, and the postoperative outcomes, including the duration of use of antibiotics, the length of hospital stay, and complications, were also recorded.
The appendectomies were performed by on-duty surgeons in the department of general surgery. Inclusion criteria included either an open appendectomy or laparoscopic appendectomy. A normal saline irrigation of the peritoneal cavity was performed at the will of the surgeon. In the cases of perforated appendicitis, however, all the surgeons performed a peritoneal irrigation with normal saline. Only closed-suction drains (Jackson-Pratt, JP) were inserted according to the surgeon's judgment. Perioperative intravenous antibiotics were used in all cases. Oral antibiotics were sometimes administered, depending on the patient's condition at discharge.
The appendix was classified postoperatively into 1 of 5 categories after pathological confirmation: normal, hyperemic, suppurative, gangrenous, or perforated. Surgical complications other than abscess formation, including wound infection and small bowel obstruction, were also identified. Postoperative abscess was diagnosed through imaging studies, such as computed tomography or ultrasound, performed by radiologists. Small bowel obstruction was clinically identified in patients with bowel distension with no movement and no bowel sound for more than 3 days after surgery, and in those that showed air-fluid levels in abdominal x-rays.
The children who were diagnosed with perforated appendicitis during the pathological analysis were grouped into 2 groups according to whether a JP drain was inserted during surgery. Both groups were then compared regarding the preoperative features and postoperative outcomes, including complications. All other pathological categories, including gangrenous appendicitis, were excluded from analysis.
All the data were collected by a single individual who had no role in clinical care. The continuous data were compared using an independent sample, 2-tailed Student t-test. The nominal data were analyzed with the chi-square test or Fisher exact test. A P-value < 0.05 defined statistical significance. PASW Statistics ver. 18 (SPSS, Inc., Chicago, IL, USA) was used for all the statistical analyses.
Between March 2003 and September 2012, 342 children were treated for perforated appendicitis. The mean patient age was 10.6 ± 4.1 years (range, 1 to 18 years); 201 (58.8%) were male, and 141 were female. Patients who presented with abdominal pain accounted for 92.4% of the sample (316 of 333) and had a mean onset time of 1.2 ± 1.4 days (range, 0 to 9 days). At the initial visit, the patients' mean temperature was 37.4℃ (range, 36℃ to 41℃), and the mean white blood cell count was 16,080 ± 5,070/mm3 with segmented neutrophils accounting for 82.3%. One hundred sixty-one patients (47.1%) underwent laparoscopic appendectomy. JP drains were placed in 108 cases (31.6%) and were removed an average of 7.1 ± 9.7) days after surgery. Postoperative complications included intra-abdominal abscess formation (n = 13, 3.8%), wound infection (n = 15, 4.4%), small bowel obstruction (n = 11, 3.2%), and pneumonia (n = 1, 0.3%). The mean length of hospitalization was 4.7 ± 3.0 days.
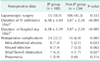
There were no statistically significant differences in gender, body mass index or Alvarado score between the patients with JP drains and those without (Table 1). The type of surgery (laparoscopic or not) did not differ between the groups. The patients with JP drains had longer hospital stays and higher complication rates, including the formation of postoperative abscesses, compared with the patients with no drains. Regarding each type of complication, the rates of intraabdominal abscess formation and small bowel obstruction were significantly higher in the JP group. There were no significant differences between the groups concerning wound infection or pneumonia (Table 2).
Appendicitis is a very common cause for surgery in children [3]. However, the signs and symptoms vary considerably, and the management of appendicitis and its complications has not yet been standardized. As mentioned above, saline irrigation is not beneficial to patients with perforated appendicitis, although there have been debates on this subject [4]. Nonetheless, few studies have examined peritoneal drain insertion after appendectomy in children with perforated appendicitis, including a large number of patients.
Intra-abdominal abscess is one of the major postoperative complications in children undergoing appendectomy. The usual incidence of postoperative abscess formation in children with acute appendicitis is 0% to 2.2% [12,13,14]. When confined to perforated appendicitis, the rate of abscess formation is higher. Intraabdominal abscess was reported to occur at the rate of 1.3% to 12.8% in patients who had a drain inserted and at the rate of 1.7% to 8% in those without drains [5]. In our study, the abscess rate was 7.4% for the JP group and 2.1% for the non-JP group (P = 0.023). Although there were no statistically significant differences in the development of a postoperative abscess and wound infection between the groups, one group underwent both irrigation and drainage, while the other group received neither irrigation nor drainage. Akkoyun and Tuna [5] reported that the incidence of postoperative abscess was lower in the nondrainage, nonirrigation group. They suggested that keeping the drain tube in the peritoneal cavity increased discharge, as well as cause foreign body reactions and tract infections. Moreover, the drain would not be able to cover the entire peritoneal cavity because the tip is localized in the pelvis. Additionally, communication between the peritoneal cavity and the extraperitoneal environment can impair the natural immune defense mechanism [6,15].
Small bowel obstruction is another serious complication that can occur after appendectomy for perforated appendicitis. Although it is rarely addressed in the literature, the rates of prolonged ileus have been reported to be 1.5% to 14.2% in some studies [5]. In this study, 6.5% of the patients in the JP group developed small bowel obstruction compared with 1.7% of the patients in the non-JP group (P = 0.027). Similar to postoperative abscess formation, foreign-body reactions and inflammation could aggravate bowel movement and lead to the symptoms of small bowel obstruction.
Regarding wound infection, the rate was 7.4% in the patients with drainage and 3.0% in the cases in which no drains were inserted. This difference was only a trend and was not statistically significant (P = 0.062).
In this study, there was a statistically significant difference in the duration of the use of antibiotics between the two groups. However, the Pearson correlation coefficient was 1.0 between hospital stay and the duration of treatment with intravenous antibiotics. In fact, the duration of these 2 factors was in complete accord. In cases of the use of antibiotics, these results were expected because all surgeons use antibiotics for acute appendicitis, and most surgeons predetermine the duration of postoperative intravenous antibiotics [10]. The prolonged use of antibiotics in patients with complications such as intraabdominal abscess formation and wound infection indicates that antibiotics have no preventative effects against such complications. As Memon et al. [7] state in their report, "drains are not a substitute for meticulous surgical technique".
Our study addresses the efficacy of drain placement by comparing the length of hospital stay between patients who had a JP drain placed and those who did not. Although hospital stay is not a direct measure of recovery, the length of hospital stay can correlate with recovery time because patients must meet certain clinical criteria before discharge. We found that the children in the JP group needed 2 additional hospital days for recovery compared with the children in the non-JP group. (6.38 ± 3.59 vs. 3.87 ± 2.38, P < 0.001). Some of the obvious advantages to a shorter postoperative hospital stay include reduced in-hospital costs, fewer hospital-acquired infections, more available beds for other patients, and the conservation of hospital resources [16].
The limitations of this study include its retrospective design and the absence of randomization between patient cohorts. It is also likely that drains were inserted in the most severe cases, based on the discretion of the surgeon on-duty. We intended to minimize differences between the JP group and the non-JP group by including only pathologically perforated patients, and as can be seen in Table 1, preoperative features do not differ between both groups. Nevertheless, our study provides the beginnings of a framework to examine the value of drain insertion after appendectomy for perforated appendicitis. In the near future, we expect to perform a prospective randomized controlled trial comparing the use and abandonment of postoperative drains after appendectomy to inform an evidencebased practice. We hope that this cost-effective treatment guideline will be useful in treating children with perforated appendicitis under the DRG system.
References
1. Newman K, Ponsky T, Kittle K, Dyk L, Throop C, Gieseker K, et al. Appendicitis 2000: variability in practice, outcomes, and resource utilization at thirty pediatric hospitals. J Pediatr Surg. 2003; 38:372–379.
2. Gasior AC, Marty Knott E, Ostlie DJ, St Peter SD. To drain or not to drain: an analysis of abscess drains in the treatment of appendicitis with abscess. Pediatr Surg Int. 2013; 29:455–458.
3. Okoye BO, Rampersad B, Marantos A, Abernethy LJ, Losty PD, Lloyd DA. Abscess after appendicectomy in children: the role of conservative management. Br J Surg. 1998; 85:1111–1113.
4. St Peter SD, Adibe OO, Iqbal CW, Fike FB, Sharp SW, Juang D, et al. Irrigation versus suction alone during laparoscopic appendectomy for perforated appendicitis: a prospective randomized trial. Ann Surg. 2012; 256:581–585.
5. Akkoyun I, Tuna AT. Advantages of abandoning abdominal cavity irrigation and drainage in operations performed on children with perforated appendicitis. J Pediatr Surg. 2012; 47:1886–1890.
6. Narci A, Karaman I, Karaman A, Erdogan D, Cavusoglu YH, Aslan MK, et al. Is peritoneal drainage necessary in childhood perforated appendicitis? A comparative study. J Pediatr Surg. 2007; 42:1864–1868.
7. Memon MA, Memon B, Memon MI, Donohue JH. The uses and abuses of drains in abdominal surgery. Hosp Med. 2002; 63:282–288.
8. Helmer KS, Robinson EK, Lally KP, Vasquez JC, Kwong KL, Liu TH, et al. Standardized patient care guidelines reduce infectious morbidity in appendectomy patients. Am J Surg. 2002; 183:608–613.
9. Lund DP, Murphy EU. Management of perforated appendicitis in children: a decade of aggressive treatment. J Pediatr Surg. 1994; 29:1130–1133.
10. Chen C, Botelho C, Cooper A, Hibberd P, Parsons SK. Current practice patterns in the treatment of perforated appendicitis in children. J Am Coll Surg. 2003; 196:212–221.
11. Singh K, Gupta S, Pargal P. Application of Alvarado scoring system in diagnosis of acute appendicitis. JK Sci. 2008; 10:84–86.
12. Pearl RH, Hale DA, Molloy M, Schutt DC, Jaques DP. Pediatric appendectomy. J Pediatr Surg. 1995; 30:173–178.
13. Gorenstein A, Gewurtz G, Serour F, Somekh E. Postappendectomy intra-abdominal abscess: a therapeutic approach. Arch Dis Child. 1994; 70:400–402.
14. Putnam TC, Gagliano N, Emmens RW. Appendicitis in children. Surg Gynecol Obstet. 1990; 170:527–532.
15. Heel KA, Hall JC. Peritoneal defences and peritoneum-associated lymphoid tissue. Br J Surg. 1996; 83:1031–1036.
16. Whyte C, Tran E, Lopez ME, Harris BH. Outpatient interval appendectomy after perforated appendicitis. J Pediatr Surg. 2008; 43:1970–1972.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download