Abstract
Purpose
The aim of this study was to investigate the impact of the visceral fat area (VFA) of patients with gastric cancer undergoing laparoscopic surgery on operative outcomes such as number of retrieved lymph nodes (LNs) and operative time.
Methods
We retrospectively reviewed the medical records and the CT scans of 597 patients with gastric cancer who underwent laparoscopy assisted distal gastrectomy (LADG) with partial omentectomy and LN dissection (>D1 plus beta). Patients were stratified by gender, VFA, and body mass index (BMI), and the clinicopathologic characteristics and operative outcomes were evaluated. Multiple linear regression analysis was used to assess the effects of VFA and BMI on the number of retrieved LNs and operative time in male and female patients.
Results
The mean number of retrieved LNs was significantly decreased for both male and female patients with high VFA. The operative time was significantly longer for both male and female patients with high VFA. The number of retrieved LNs had a statistically significant negative correlation with VFA in both men and women, but not with BMI. The operative time had a statistically significant positive correlation with VFA in men, whereas the operative time had a statistically significant positive correlation with BMI in women.
According to World Health Organization, gastric cancer is one of the most common cancers worldwide. In Korea, the use of laparoscopy has led to the majority of the patients being diagnosed as early gastric cancer (EGC), which can be successfully treated using surgical resection alone [1,2]. Surgeons have noticed that surgical outcomes are associated with the quality of life after gastrectomy [3]. Because laparoscopic surgery has improved operative outcomes, such as shorter convalescent time, less postoperative pain, and faster return to social life, it has become popular for treating gastric cancer [4].
The increasing prevalence of obesity has also become an important problem worldwide [5]. Obesity initially was a relative contraindication for laparoscopic surgery. However, with the refinement of laparoscopic technology and the increasing experience of surgeons, the use of laparoscopic surgery for obese patients has been widely accepted. There have been several randomized clinical trials examining surgical outcomes that have verified its safety for these patients [6,7].
However, surgeons still find that laparoscopic surgery for obese patients is challenging. The retrieval of lymph nodes (LNs) is difficult because they are embedded in thick fat tissue and are hard to distinguish surrounding fat [8]. Therefore, the operative time is prolonged. Some studies have investigated that the association between obesity and operative outcomes [8,9,10,11,12,13]. Surgical procedures performed on patients with high body mass index (BMI) have been found to be of longer duration [9,10]. Other studies have reported that the visceral fat area (VFA) was a better predictor of surgical outcomes than a BMI indicating obesity [11,12,13].
There have been few large studies investigating the impact of VFA on the outcome of laparoscopy-assisted distal gastrectomy (LADG). The aim of our retrospective study was to investigate the impact of VFA on the operative outcomes of LADG performed on a large number of gastric cancer patients who, for purposes of analysis, were divided into 4 subgroups based on gender and 2 parameters of obesity, BMI and VFA.
The medical records and CT scans of 597 patients with gastric cancer who underwent LADG with partial omentectomy and LN dissection (>D1 plus beta), between March 2003 and July 2013 were retrospectively reviewed. These patients included our initial cases of LADG. We excluded patients who underwent robotic surgery or combined surgery during LADG and patients whose CT scans could not be to measure the VFA. All of the operations were performed by a single surgeon.
All patients underwent abdominal CT scans before surgery to assess the extent of disease. The CT scanner was linked to a medical imaging network, through which images could be electronically transferred to a centralized data system and retrieved at a workstation. Imaging software, Aquarius iNtuition, TeraRecon (TeraRecon Inc., Foster City, CA, USA), was used to acquire the preprocessed images. The CT scan at the umbilical level was used to measure VFA [14]. The contours of the subcutaneous layer of fat and the VFA were defined automatically by the fat scan, and then we can obtain VFA through fat analysis. To elaborate, the process of drawing the contour manually was added before fat analysis.
The patients were divided into 4 subgroup based on gender and obesity criteria from the Japan Society for the Study of Obesity [15]. Patients with a VFA ≥ 100 cm2 were classified as high VFA and patients with a VFA < 100 cm2 were low VFA. Likewise, patients with a BMI ≥ 25 kg/m2 were classified as high BMI and patients with a BMI < 25 kg/m2 were classified as low BMI.
We analyzed retrospectively the complications from prospectively designed gastric cancer database. We classified by our list of complications list (17 lists): 1. wound problems (infection, seroma, bleeding, evisceration); 2. intraabominal fluid collection or abscess; 3. intra-abdominal bleeding; 4. intraluminal bleeding; 5. intestinal obstruction; 6. Ileus; 7. Stenosis; 8. Leakage; 9. Fistula; 10. Pancreatitis; 11. pulmonary disease; 12. urinary complications; 13. renal complications; 14. hepatic complications; 15. cardiac complications; 16. endocrine complications; 17. others.
All statistical analyses were performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). The Pearson chi-square test was used to compare categorical variables. An independent t-test or analysis of variance were used for continuous variables if the data for groups satisfied the criteria for normality; otherwise, the Mann-Whitney U-test or Kruskal-Wallis test were used. Multiple-linear regression analysis was used to assess the effects of visceral fat on operative outcomes. P-values less than 0.05 were considered to indicate statistical significance. All reported P-values are two-tailed and have not been adjusted for multiple comparisons.
Fig. 1 depicts the distribution of VFA in male patients and female patients. The VFA values of both men and women were normally distributed. The mean VFA values for men and women were 100.3 cm2 and 78.9 cm2, respectively.
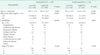
All patients were assigned to one of 4 groups according to gender and high and low VFA. Table 1 lists the clinicopathological characteristics of the patients divided into subgroups. For both men and women, increased age tended to associate with high VFA women, the difference in age between low and high VFA was significant (P < 0.001). BMI was significantly higher in both male and female patients with high VFA than in patients with low VFA (both P < 0.001). Of the male and female patients with high BMI, 86 men (80.4%, n = 107) and 43 women (63.2%, n = 68) also had high VFA. Of male patients with low BMI, 97 (35.8%, n = 271) had high VFA whereas of female patients with high BMI, 25 (36.8%, n = 68) had low VFA. Significantly more male and female patients with high VFA had comorbid conditions than those with low VFA (both P < 0.001).
The total number of retrieved LNs was significantly decreased in both male and female patients with high VFA (men, P < 0.001; women, P = 0.001). The operative time was significantly longer for both men and women with high VFA (men, P < 0.001; women; P = 0.033). The time to first flatus was significantly longer in male patients with high VFA (P = 0.013) (Table 2). There were no significant differences in length of postoperative hospital stay and complication rate based on VFA values of either men or women.
When the male patients and female patients were each divided into 4 subgroups (low BMI/low VFA, low BMI/high VFA, high BMI/low VFA, high BMI/high VFA), there was a statistically significant difference in the mean number of retrieved LNs between the subgroups of both men and women (men, P < 0.001; women, P = 0.013) (Fig. 2). Post hoc analysis found that a statistically significant difference in the number of retrieved LNs between the low BMI/low VFA and high BMI/high VFA groups of both the men and women (men, P = 0.005; women; P = 0.028). There was also a statistically significant difference in the number of retrieved LNs between the male patient with low BMI/low VFA and low BMI/high VFA (P < 0.001).
When the male patients and female patients were each divided into 4 subgroups (low BMI/low VFA, low BMI/high VFA, high BMI/low VFA, and high BMI/high VFA) there was a statistically significant difference in the mean operative times between the 4 subgroups of men (P = 0.001) (Fig. 3). Although for women there seemed to be an obvious difference for the patients with high BMI/high VFA, post hoc analysis did not find statistical significance. For men, although the VFA seemed to affect the operative time regardless of BMI level, post hoc analysis found that there was a statistically significant difference in operative time between those with low BMI/low VFA and high BMI/high VFA (P = 0.004).
Table 3 shows the results of multiple regression analysis of BMI and VFA on the number of retrieved LNs and operative time. The number of retrieved LNs had a statistically significant negative correlation with VFA in both men and women (men, P < 0.001; women, P = 0.010), but not with BMI. The operative time had a statistically significant positive correlation with VFA in men (P < 0.001), whereas the operative time had a statistically significant positive correlation with BMI (P = 0.031) in women.
In Korea and Japan, gastric cancer is now detected in the early stages because of the expansion of their National Health Screening Systems and advanced endoscopic techniques [2]. EGC is usually treated using laparoscopic subtotal gastrectomy [1]. Laparoscopic surgery is now popular because it is minimally invasive surgery and has been proven by several clinical studies to be safe, compared with open surgery for gastric cancer [3]. Now, also obese patients undergo LADG. It is widely known that laparoscopic surgery for obese patients is difficult, and there have been many studies evaluating the surgical outcomes of laparoscopic surgery for these patients. The safety and feasibility of laparoscopic surgery for these patients are proven to be no different from open surgery [6,7], but the surgical outcomes of obese patients undergoing LADG remains debatable.
Some studies of LADG have used BMI as the indicator of obesity. Kim et al. [10] reported that male patients with a BMI ≥ 23 kg/m2 had longer operative time. Ojima et al. [12] found that the operative time of male patients with a large fat volume and high abdominal shape index was longer. Both studies confirmed significant correlations for obese male patients, but not for female patients.
There have been some studies on VFA. Yoshikawa et al. [11] reported that the rate of postoperative complications was higher, the mean volume of blood loss was larger, and the mean number of retrieved LNs was smaller all significantly in patients was high VFA value suggesting that VFA might be a useful parameter for predicting the risks of LADG. Miyaki et al. [13] reported that the operative time was significantly longer and volume of blood loss was significantly larger in patients with high VFA value, but that stratification base on BMI did not show significant differences. Hence, they concluded that VFA was a more accurate predictor of operative time and postoperative complications. Although the reports by Yoshikawa et al. [11] and Miyaki et al. [13] concluded that VFA reflected surgical outcomes better than BMI, they only evaluated small numbers of patients, 64 and 84, respectively.
Ishii et al. [16] evaluated the effect of visceral obesity on surgical outcomes of patients with rectal cancer, and reported that patients with high VFA had a longer operative time and high frequency of complication. By univariate analysis, male gender and visceral obesity, but not general obesity, were significant independent factors associated with complications. Matsumoto et al. [17] reported that VFA did affect significantly intraoperative bleeding, the number of retrieved LNs, and postoperative complications, whereas BMI did not. They also described that both BMI and VFA were not related to surgical outcomes, such as operative time, intraoperative bleeding, retrieved LNs and postoperative surgical complications in rectal cancer.
Length of operation could be overcome as the surgical experiences increased even in the high VFA cases. In our study, both male and female patients with high VFA value had significantly decreased mean numbers of retrieved LNs and prolonged operative times. Men with high VFA value had a smaller number of retrieved LNs and longer operative time than men with low VFA by multiple regression analysis. Women with high VFA had a smaller number of retrieved LNs, but operative time was longer in women with high BMI. These results suggest that LN retrieval is affected by VFA regardless of gender, whereas the operative time was longer in the female patients, whose overall fat volume was large, regardless of visceral obesity. This can be accounted for by the fact that women have more subcutaneous fat than visceral fat compared with men, and therefore VFA cannot be an independent predictive factor of the operative time in female patients.
We performed subgroup analysis according to gender, BMI, and VFA for surgical outcome. Regarding LN retrieval, the numbers of retrieved LNs between 4 subgroups of men and women were significantly different. There were significant differences in the operative time of male patients only. In female patients, the difference of operation time between high BMI and high VFA group and the other groups was not statistically significant, but operation time itself differ each other distinctly.
This was a large, single-center retrospective study evaluating the VFA of patients with gastric cancer who underwent LADG. The results of the gender, VFA, and BMI subgroup analyses of the operative outcomes might, in practice, be helpful in practice for inexperienced surgeons.
In conclusion, the preoperative VFA of male patients with gastric cancer who undergo LADG may affect the number of retrieved LNs and operative time. The preoperative VFA of female patients with gastric cancer did not appear to affect operative time. However, VFA was more useful than BMI in predicting operative outcomes.
Figures and Tables
 | Fig. 1Distribution of the values of the visceral fat area of gastric cancer patients (n = 597) according to gender. Both genders have normal distribution, with mean values in men (A) and women (B) of 100.3 cm2 and 78.9 cm2, respectively (Axis x = distribution of the values of the visceral fat area, axis y = number of patients). |
 | Fig. 2The mean number of retrieved lymph nodes (LNs) according to gender, body mass index (BMI), and visceral fat area (VFA) of patients with gastric cancer undergoing laparoscopic surgery. There was a statistically significant difference in the mean number of retrieved lymph nodes between the 4 subgroups of both men and women (men, P < 0.001; women, P = 0.013). BMI_L, low BMI; BML_H, high BMI; VFA_L, low VFA; VFA_H, high VFA. |
 | Fig. 3The mean operative time according to gender, body mass index (BMI), and visceral fat area (VFA) of patients with gastric cancer undergoing laparoscopic surgery. There was a statistically significant difference between 4 subgroups in men, only. BMI_L, low BMI; BML_H, high BMI; VFA_L, low VFA; VFA_H, high VFA. |
Table 1
The clinicopathological characteristics of patients with gastric cancer who underwent LADG according to gender and visceral fat area
References
1. van de Velde CJ, Peeters KC. The gastric cancer treatment controversy. J Clin Oncol. 2003; 21:2234–2236.
2. Hyung WJ, Kim SS, Choi WH, Cheong JH, Choi SH, Kim CB, et al. Changes in treatment outcomes of gastric cancer surgery over 45 years at a single institution. Yonsei Med J. 2008; 49:409–415.
3. Koeda K, Nishizuka S, Wakabayashi G. Minimally invasive surgery for gastric cancer: the future standard of care. World J Surg. 2011; 35:1469–1477.
4. Hur H, Xuan Y, Ahn CW, Cho YK, Han SU. Trends and outcomes of minimally invasive surgery for gastric cancer: 750 consecutive cases in seven years at a single center. Am J Surg. 2013; 205:45–51.
5. Perez Rodrigo C. Current mapping of obesity. Nutr Hosp. 2013; 28:Suppl 5. 21–31.
6. Ohno T, Mochiki E, Ando H, Ogawa A, Yanai M, Toyomasu Y, et al. The benefits of laparoscopically assisted distal gastrectomy for obese patients. Surg Endosc. 2010; 24:2770–2775.
7. Yamada H, Kojima K, Inokuchi M, Kawano T, Sugihara K. Effect of obesity on technical feasibility and postoperative outcomes of laparoscopy-assisted distal gastrectomy: comparison with open distal gastrectomy. J Gastrointest Surg. 2008; 12:997–1004.
8. Lee JH, Paik YH, Lee JS, Ryu KW, Kim CG, Park SR, et al. Abdominal shape of gastric cancer patients influences short-term surgical outcomes. Ann Surg Oncol. 2007; 14:1288–1294.
9. Shim JH, Song KY, Kim SN, Park CH. Laparoscopy-assisted distal gastrectomy for overweight patients in the Asian population. Surg Today. 2009; 39:481–486.
10. Kim KH, Kim MC, Jung GJ, Kim HH. The impact of obesity on LADG for early gastric cancer. Gastric Cancer. 2006; 9:303–307.
11. Yoshikawa K, Shimada M, Kurita N, Iwata T, Nishioka M, Morimoto S, et al. Visceral fat area is superior to body mass index as a predictive factor for risk with laparoscopy-assisted gastrectomy for gastric cancer. Surg Endosc. 2011; 25:3825–3830.
12. Ojima T, Iwahashi M, Nakamori M, Nakamura M, Takifuji K, Katsuda M, et al. The impact of abdominal shape index of patients on laparoscopy-assisted distal gastrectomy for early gastric cancer. Langenbecks Arch Surg. 2012; 397:437–445.
13. Miyaki A, Imamura K, Kobayashi R, Takami M, Matsumoto J. Impact of visceral fat on laparoscopy-assisted distal gastrectomy. Surgeon. 2013; 11:76–81.
14. Sottier D, Petit JM, Guiu S, Hamza S, Benhamiche H, Hillon P, et al. Quantification of the visceral and subcutaneous fat by computed tomography: interobserver correlation of a single slice technique. Diagn Interv Imaging. 2013; 94:879–884.
15. Examination Committee of Criteria for 'Obesity Disease' in Japan. Japan Society for the Study of Obesity. New criteria for 'obesity disease' in Japan. Circ J. 2002; 66:987–992.
16. Ishii Y, Hasegawa H, Nishibori H, Watanabe M, Kitajima M. Impact of visceral obesity on surgical outcome after laparoscopic surgery for rectal cancer. Br J Surg. 2005; 92:1261–1262.
17. Matsumoto N, Shimada M, Kurita N, Iwata T, Nishioka M, Morimoto S, et al. The role of body mass index and visceral fat area in colorectal cancer patients treated with laparoscopic-assisted surgery [abstract]. In : Society of American Gastrointestinal and Endoscopic Surgeons 2010; 2010 Apr 14-17; Los Angeles (CA): Society of American Gastrointestinal and Endoscopic Surgeons;2010.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download