Abstract
Purpose
This study was designed to determine the factors affecting completion of critical pathway for elective gastrectomy.
Methods
Since 2008, a critical pathway has been applied for elective gastrectomy at Chosun University Hospital. We retrospectively analyzed 252 patients who underwent elective gastrectomies from January 2009 to April 2013. The completion rate was determined, and risk factors for patient dropout were examined.
Results
The completion rate of the critical pathway was 45.6% (115/252). Mean length of stay was 11.7 ± 8.6 days (8-59 days). Readmission rates were 4.4% (11/252). Causes of failure for clinical pathway were systemic complications (21/137, 15.3%), intra-abdominal complications (44/137, 32.8%), patient factors (41/137, 29.9%), and wound complications (30/137, 21.9%). There were no significant differences between the two groups in age, sex, American Society of Anesthesiologists (ASA) score, operation time, readmission, and underlying disease (P > 0.05). Body mass index (P = 0.008) and pathologic stage (P = 0.001) were significantly different between the two groups. In multivariate analysis, the conventional approach (odds ratio, 2.0), and total gastrectomy (odds ratio, 5.3) were determined to be independent risk factors to drop the critical pathway. But there were no significant differences between total and distal gastrectomy groups in age, gender, underlying diseases, ASA score, readmission, operation time, and cause of dropout (P > 0.05).
The critical pathways (CPs), also known as clinical pathways, or integrated care pathways, are structured multidisciplinary care plans used by health providers to describe the essential steps in the care of patients with particular clinical problems. The use of CPs is associated with reduced incidence of inhospital complications and improved documentation [1]. Therefore, the CP is used for the treatment of many medical conditions across the continuum of care [2,3,4,5,6,7,8,9,10]. Specifically, CPs have been widely adopted in various surgical fields to improve the efficiency of postoperative recovery [2,3,4,5,6,7,8,10]. The CP for surgical patients is structured into three subtypes (preoperative management, intraoperative management, and postoperative management); preoperative and postoperative management have improved in numerous ways over the last decade.
Despite the theoretical advantages, the impact of clinical pathways on patients undergoing gastrectomy remains unclear. The outcome of patients who undergo gastrectomy varies greatly; factors such as the patient's age and comorbidities, the complexity of the surgical procedure, and the management of postoperative recovery, all influence the outcome [10,11,12,13].
This study was designed to determine the factors that affect completion of CP for elective gastrectomy.
We developed a CP for patients with resectable gastric cancer in 2008. A single, generalized CP has been applied for all elective gastrectomy procedures at our institution, regardless of surgical approach.
In 2008, we analyzed the effectiveness of our CP; 50 elective gastrectomy cases were divided into 2 groups (non-CP and CP). Our results showed that patients in the CP group felt more satisfaction than those in the non-CP group. There were no significant differences in surgical outcomes between the 2 groups (data not shown). After 2008, the CP for resectable gastric cancer has been fully adopted at our institution.
The CP was implemented for patients who were scheduled to undergo curative resection. Patients with the following characteristics were excluded from the CP: (1) patients with cancer-related complications such as perforation or bleeding, (2) patients with concomitant presence of other malignancies, (3) patients with severe comorbidities which were not feasible for general anesthesia, (4) patients with incurable characteristics, (5) patients who did not provide consent. Patients with concomitant resection of other organs (e.g., liver, spleen, pancreas, colon), which might have affected the course of recovery were also excluded.
This study was conducted with approval from the Institutional Review Board at Chosun University Hospital (IRB No. Chosun 2013-12-008). Patient data were retrospectively collected, for all patients who underwent an elective gastrectomy for gastric cancer between January 2009 and April 2013. Demographic, operative, and postoperative data were collected for each patient, including discharge and readmission data.
The CP included staging work-up, preoperative management and postoperative management. Staging work-up (e.g., abdominal computed tomography, endoscopic examination, and basic serum chemistry) was evaluated in the outpatient clinic, before surgery. After admission, patients were instructed on surgical procedures (distal gastrectomy [DG], total gastrectomy [TG]), postoperative complications, and received detailed information on the hospital course of gastrectomy (from admission to discharge) with a timetable (Fig. 1).
Neither drains nor nasogastric tubes were left after a surgery. Patient-controlled analgesia was used to assist with postoperative analgesia. During the postoperative period, each patient was placed on a CP, which aimed at discharge by postoperative day (POD) 8. At POD 1, after removal of urethral catheter, the patient is expected to ambulate with assistance. At POD 3, a patient was allowed sips of water. At POD 5, the patient is advanced to a soft meal and educated by a dietitian. At POD 8, the discharge is recommended.
We applied laparoscopic gastrectomy (distal or TG) for earlystage (cT1N0, cT1N1, and cT2N0) tumors. Our indications for discharge as follows: afebrile for 3 days, ability to eat soft meals, and no need of intensive treatment (e.g., reoperation and intervention by radiologist). The completion of CP was attained when a patient was discharged as per schedule (at POD 8). A dropout in CP was defined as a patient who could or would not be discharged at POD 8. There were two causes of patient dropout: postoperative complications and patient's will. A complication was an unexpected event during recovery. Patient's will refers to cases where a surgeon recommended the patient's discharge, but the patient would not comply, without any medical issue. Readmission was defined as patient hospitalization within POD 30 (patients who were hospitalized to receive adjuvant chemotherapy were excluded). In order to determine the factors that could influence CP, we divided patients into 2 groups (completion CP vs. dropout CP).
All statistical analyses were conducted using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). All parameters of the two groups were compared with the two-tailed chi-square test, or Fisher exact test and a two-tailed T-test. To test differences between two or more means, analysis of variance was used. To predict the drop in CP, the binary logistic regression test for multivariate analysis was performed. In all statistical analyses, a P-value of <0.05 was considered significant. Data are provided as means ± standard deviation.
From January 2009 to April 2013, 252 patients undergoing elective radical gastrectomy with curative intent at Chosun University Hospital were enrolled in the study.
Mean age was 62.4 ± 12.2 years (30-87 years); 166/252 patients (65.9%) were male, while 86/252 patients (34.1%) were female. Mean body mass index (BMI) was 23.3 ± 3.2 kg/m2 (14.5-38.2 kg/m2). Mean length of stay was 11.7 ± 8.6 days (8-59 days). In all, 91/252 laparoscopic gastrectomies (36.1%), and 161/252 conventional gastrectomies (63.9%) were performed; 200 subtotal gastrectomies (79.4%) and 52 total gastrectomies (20.6%) were performed.
In all, 11/252 patients (4.4%) were readmitted to our hospital. There were no significant differences in readmission rates between the two groups (4 cases in completion group vs. 7 cases in dropout group, P = 0.759). The causes of readmission were determined to be ascites (n = 1), intra-abdominal abscess (n = 5), delayed gastric emptying (n = 3), anastomotic stricture (n = 1), and general weakness (n = 1).
In all, 137/252 patients (54.5%) dropped out from CP. The causes of "dropout" included wound complications (30/137, 21.9%), intra-abdominal complications (45/137, 32.8%), systemic disease (21/137, 15.3%), and patient's will (41/137, 29.9%) (Table 1).
There were no significant differences between the two groups in terms of age, sex, American Society of Anesthesiologists (ASA) score, operation time, readmission, and underlying diseases (P > 0.05). There were no significant differences between the two groups in terms of the number of harvested lymph nodes and nodal metastases (P > 0.05). However, the pathologic stages (P = 0.001) and BMI (P = 0.008) were found to be significantly different between the two groups.
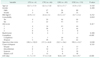
We performed univariate analyses to determine which variables were associated with dropout (Table 2). The type of approach (laparoscopic or conventional gastrectomy, P < 0.001), and extent of resection (subtotal or TG, P < 0.001) were revealed as factors that influenced the dropout.
Upon multivariate analysis, TG (P < 0.001; odds ratio, 5.3), and a conventional gastrectomy (P = 0.017; odds ratio, 2.0) were determined to be the independent risk factors associated with dropout (Table 2).
We detected no significant difference between any subgroups for age, gender, BMI, cause of dropout, readmission rate, ASA score, and underlying diseases (P > 0.05). But the completion rate, operation time and length of stay were significantly different between 4 subgroups (P < 0.05) (Table 3).
Compared to a DG, the TG was significantly associated with low completion rate, low BMI, and long length of stay (P < 0.05) (Table 4). But there were no significant differences between 2 groups in age, gender, underlying diseases, ASA score, readmission, operation time, and cause of dropout (P > 0.05).
Recent pressures to reduce the costs of health care have compelled many health care organizations to implement procedures to reduce the use of resources and decrease the lengths of hospital stay [9]. Systematized CP allows health-care teams to standardize patient management, and improve the quality and efficiency of patient care.
Despite the rapid dissemination of CP programs throughout hospitals, their development, implementation, and evaluation remain uncertain. While CPs have been adopted in many surgical procedures [2,3,4,5,6,7,8], their effectiveness for gastrectomy is still unclear [5,6,7].
We initially evaluated the efficacy of CP in our institution in 2008. Our results indicate that patients in the CP group were generally more satisfied and easily understood their hospital course (data not shown). However, the length of stay and medical costs were not analyzed in 2008. After this analysis, we have revised and entirely adapted the CP for elective gastrectomy.
Completion rates of CP (115/252, 45.6%) were higher in our study than in Jeong et al. [6]'s study (19%), but lower than in other studies (Seo et al. [5], 85.4%; Choi et al. [7], 62.4%). Unfortunately, we were unable to obtain detailed results from the 3 studies mentioned above; consequently, an accurate analysis of the factors affecting the completion of CP. However, we could assume the possible factors.
First, the underlying causes influencing the rates of patient dropout differed in 4 studies (the patient's will was regarded as a cause in our study, and in studies by Jeong et al., and Seo et al., but not in the study by Choi et al.); of the 3 studies that included patient's will as a factor, the proportions of patient's will varied in each study.
Second, in comparison to conventional gastrectomy, laparoscopic gastrectomy was associated with significantly shorter lengths of hospital stay, and lower postoperative morbidity rates [14,15,16,17]. Patient dropouts had more late-stage tumors than patients in the completion CP group (P = 0.001). Most of the early-stage (clinical stage I, II) patients underwent laparoscopic gastrectomy, whereas late-stage (clinical stage III) patients underwent conventional gastrectomy. Conventional gastrectomy was more frequently performed than laparoscopic gastrectomy (P < 0.001) in the dropout CP group. Differences in the proportion of laparoscopic gastrectomy carried out in each institution might underlie these discrepancies.
Coincidentally, we found the significant difference of BMI between the two groups (P = 0.008). But there was not much difference (23.9 ± 3.0 vs. 22.9 ± 3.2) in mean BMI between the two groups. Based on World Health Organization definition, the means of BMI in two groups were regard as normal range [18]. In order to find the cause, I divided each group into two subgroups according to their BMI (>18.5 and ≤18.5 kg/m2 group). There was significant difference between two groups (1/115 patient in completion and 12/137 patients in drop, P = 0.004). In addition, we found the reverse correlation between BMI and pathologic stage (P = 0.003). The difference of mean BMI between two groups resulted from their different stage. As was stated above, different stages might affect BMI and surgical approach.
Third, the proportions of TG may be different between each study. In our results, the completion of TG (1/6, 16.7% in laparoscopic; 7/46, 15.2% in conventional TG) were too low. We found a similar result from the study by Choi et al. [7]. They reported that the completion rate of TG (48/99, 48.5%) was lower than those of DG (217/326, 66.6%). Unfortunately, in subgroup analyses for completion of CP, there was not significantly different between subgroups for cause of dropout (Tables 3, 4).
Fourth, demographic characteristics might affect these differences.
The mean age of patients in our study was higher than that in other studies (62.4 years vs. 58.0 years, 59.2 years); older age is associated with greater mortality and morbidity after gastrectomy [12,13]. In general, senior citizens present with one or more comorbidities. While the other institutions were located within capital territory of Korea, our institution is located within an agricultural region of Korea.
Most senior citizens in these areas live without their children, on a small income; they have difficulty receiving proper medical care, and these factors may influence their discharge rates.
By excluding instances of patient noncompliance, the completion rate of CPs was found to increase from 45.6% (115/252) to 61.9% (156/252) in our study.
In this study, seromas formed a majority of the wound complications. The mean length of stay for a patient with wound complications was 16.6 ± 8.0 days (10-47 days). While a wound seroma does not require intensive care, most of these patients refused to be discharged even though they were progressing favorably, because they lived alone in a rural area. This indicates the need to reduce the incidence of wound complications.
In order for a strict discharge pathway to be successful, several factors are absolutely critical. There must be an effort to educate each patient on what to expect during the postoperative period, including a thorough explanation of all steps of the pathway [8].
Complications are directly associated with the length of stay and medical costs; therefore, a healthcare team should consider the patient's susceptibility to complications (e.g., malnutrition, diabetes) prior to surgery.
At our institution, patient education begins in the clinic preoperatively, and continues in the preoperative area on the day of surgery, into the postoperative period. Our healthcare team is composed of surgeons, specialized nurses, and dieticians. After gastrectomy, patients receive a timetable detailing the course of recovery, and it is attached to the bedside (Fig. 1).
Only a single, generalized CP has been adapted for elective gastrectomy at our institution. On multivariate analysis, we found that the surgical approach (laparoscopic vs. conventional gastrectomy, P = 0.017), and extent of resection (subtotal or TG, P < 0.001) were independent risk factors that could influence the completion of CP. While completion rate of CP in DG patients was 53.5% (107/200), completion rate in TG patients was 15.4% (8/52).
It suggested that our CP might have its own fault and TG might not be suitable for CP. A different procedure may require different medical care. But, unfortunately, our single CP did not provide the proper medical care. We concluded that TG may not be suitable for the CP. We suggest that the CP for elective DG is divided 2 subgroups, according to the surgical approach.
Figures and Tables
 | Fig. 1Critical pathway for elective gastrectomy. Preop., preoperative; Postop., postoperative; POD, postoperative day; NPO, non per os; OR, operating room; PRN, pro re nata; UGI, upper gastrointestinography; TG, total gastrectomy. |
Table 2
Univariate and multivariate analysis of risk factors for dropout

Values are presented as mean ± standard deviation or number unless otherwise indicated.
OR, odds ratio; CI, confidence interval; BMI, body mass index; ASA, American Society of Anesthesiologists; CG, conventional gastrectomy; LG, laparoscopic gastrectomy; TG, total gastrectomy; DG, distal gastrectomy.
Pathologic stages are as described in the seventh edition of American Joint Committee on Cancer TNM classification.
References
1. Rotter T, Kinsman L, James E, Machotta A, Willis J, Snow P, et al. The effects of clinical pathways on professional practice, patient outcomes, length of stay, and hospital costs: Cochrane systematic review and meta-analysis. Eval Health Prof. 2012; 35:3–27.
2. Zhang M, Zhou SY, Xing MY, Xu J, Shi XX, Zheng SS. The application of clinical pathways in laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int. 2014; 13:348–353.
3. Saint S, Hofer TP, Rose JS, Kaufman SR, McMahon LF Jr. Use of critical pathways to improve efficiency: a cautionary tale. Am J Manag Care. 2003; 9:758–765.
4. Nussbaum DP, Penne K, Stinnett SS, Speicher PJ, Cocieru A, Blazer DG 3rd, et al. A standardized care plan is associated with shorter hospital length of stay in patients undergoing pancreaticoduodenectomy. J Surg Res. 2015; 193:237–245.
5. Seo HS, Song KY, Jeon HM, Park CH. The impact of an increased application of critical pathway for gastrectomy on the length of stay and cost. J Gastric Cancer. 2012; 12:126–131.
6. Jeong SH, Yoo MW, Yoon HM, Lee HJ, Ahn HS, Cho JJ, et al. Is the critical pathway effective for the treatment of gastric cancer? J Korean Surg Soc. 2011; 81:96–103.
7. Choi JW, Xuan Y, Hur H, Byun CS, Han SU, Cho YK. Outcomes of critical pathway in laparoscopic and open surgical treatments for gastric cancer patients: patients selection for fast-track program through retrospective analysis. J Gastric Cancer. 2013; 13:98–105.
8. Walters DM, McGarey P, LaPar DJ, Strong A, Good E, Adams RB, et al. A 6-day clinical pathway after a pancreaticoduodenectomy is feasible, safe and efficient. HPB (Oxford). 2013; 15:668–673.
9. Pearson SD, Goulart-Fisher D, Lee TH. Critical pathways as a strategy for improving care: problems and potential. Ann Intern Med. 1995; 123:941–948.
10. Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009; 361:1368–1375.
11. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009; 360:1418–1428.
12. Lee KG, Lee HJ, Yang JY, Oh SY, Bard S, Suh YS, et al. Risk factors associated with complication following gastrectomy for gastric cancer: retrospective analysis of prospectively collected data based on the Clavien-Dindo system. J Gastrointest Surg. 2014; 18:1269–1277.
13. Bartlett EK, Roses RE, Kelz RR, Drebin JA, Fraker DL, Karakousis GC. Morbidity and mortality after total gastrectomy for gastric malignancy using the American College of Surgeons National Surgical Quality Improvement Program database. Surgery. 2014; 156:298–304.
14. Cheng Q, Pang TC, Hollands MJ, Richardson AJ, Pleass H, Johnston ES, et al. Systematic review and meta-analysis of laparoscopic versus open distal gastrectomy. J Gastrointest Surg. 2014; 18:1087–1099.
15. Li HT, Han XP, Su L, Zhu WK, Xu W, Li K, et al. Short-term efficacy of laparoscopyassisted vs open radical gastrectomy in gastric cancer. World J Gastrointest Surg. 2014; 6:59–64.
16. Kim YW, Baik YH, Yun YH, Nam BH, Kim DH, Choi IJ, et al. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg. 2008; 248:721–727.
17. Viñuela EF, Gonen M, Brennan MF, Coit DG, Strong VE. Laparoscopic versus open distal gastrectomy for gastric cancer: a meta-analysis of randomized controlled trials and high-quality nonrandomized studies. Ann Surg. 2012; 255:446–456.
18. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995; 854:1–452.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download