Abstract
Purpose
Laparoscopic sleeve gastrectomy (LSG) has been gaining marked popularity as a stand-alone treatment for morbid obesity. This study aimed to evaluate the midterm outcomes and efficacy of LSG performed at a single center in Korea.
Methods
The records of 192 consecutive patients who underwent LSG between April 2009 and December 2012 were retrospectively reviewed. The patients' demographics and surgical outcomes including anthropometric data were analyzed.
Results
The mean preoperative body mass index was 40.0 ± 7.2 kg/m2, and 120 patients (62.5%) had at least one obesity-related comorbidity. Three patients (1.6%) required endoscopic or surgical intervention to manage postoperative bleeding or leakage. At the postoperative 1-, 2-, 3-, and 4-year follow-ups, the mean percent of excess weight loss (%EWL) values were 72.6%, 80.6%, 71.1%, and 57.8%, respectively, with follow-up rates of 81%, 56%, 58%, and 30% respectively. The overall mean %EWL reached 68.3% ± 27.2% at a mean follow-up of 25 months. Obesity-related comorbidities were resolved in >70% of the patients after surgery. Twelve months after LSG, 25 patients (13.0%) showed a %EWL of <50%; 9 (4.7%) required conversion to gastric bypass due to inadequate weight loss, intolerable reflux symptoms, or intractable diabetes.
Sleeve gastrectomy, a vertical gastrectomy that leaves a gastric tube along the lesser curvature of the stomach, was first described by Marceau et al. [1] in the early 1990s. The procedure was devised as a substitute for distal gastrectomy of existing biliopancreatic diversion (BPD), proposed by Scopinaro et al. [2], to preserve physiologic gastric functioning. The sleeve gastrectomy procedure was performed as the restrictive part of BPD with duodenal switch (DS), and facilitated preserved regulation of gastric emptying and the gastroduodenal contribution to satiety. This was accomplished through retention of vagal innervation along the lesser curvature and reduction of the parietal cell mass to minimize the incidence of marginal ulcers. BPD-DS was reported to provide excellent long-term results, even up to 15 years of follow-up [3].
With the advancement of laparoscopic skills, laparoscopic sleeve gastrectomy (LSG) was adopted as a component of laparoscopic BPD in the early 2000s. Laparoscopic BPD, however, was regarded as being too complicated and was associated with a high risk of surgical complications when performed as a single-stage procedure in extremely heavy patients in the early laparoscopic era [4]. Therefore, a two-stage operative approach gained popularity, in which LSG was performed as a bridging procedure to facilitate subsequent gastric bypass or BPD surgeries, 6-12 months later, in superobese patients or in those with high surgical risk [5,6]. LSG gradually became a stand-alone procedure following several reports of excellent weight loss outcomes after only LSG [5,7,8].
This study aimed to evaluate the efficacy and midterm outcomes of LSG in morbidly obese patients at a single specialized center in Korea.
The medical records of all consecutive patients undergoing LSG at Soonchunhyang University Seoul Hospital (Korea), between April 2009 and December 2012, were retrospectively reviewed. Baseline, operative, and follow-up data from a prospectively established database were thoroughly reviewed and summarized. Approval for this review of hospital records was obtained from the Institutional Review Board (SCHUH 2014-06-003-001); the need for patient informed consent was waived.
Bariatric surgery candidates were selected according to the 2011 International Federation for the Surgery of Obesity-Asia Pacific Chapter Consensus statement [9]. As such, patients with a body mass index (BMI) of ≥30 kg/m2 and inadequately controlled obesity-related comorbidities (e.g., diabetes, obstructive sleep apnea, hypertension, and obesity-related arthropathy) or those with a BMI of ≥35 kg/m2 were considered for bariatric surgery. The choice between LSG and Roux-en-Y gastric bypass (RYGB) was made on an individual basis, in discussion with the patient. Patients received interdisciplinary education about potential surgical and nonsurgical options, possible outcomes, possible complications, and necessary postoperative lifestyle changes, at which point each provided informed consent for the chosen operation.
All procedures were performed laparoscopically by a single surgeon with sufficient experience in upper gastrointestinal surgeries. Six trocars were used to perform LSG: one 11-mm port for a camera at the umbilicus, two 12-mm ports for stapling in the right lower and left upper quadrants, and three 5-mm ports for assistance and liver retraction. The first trocar was usually placed in the left upper quadrant, using the optical access method, to establish a pneumoperitoneum. Gastric resection was performed using laparoscopic linear staplers to create a staple line parallel to the lesser curvature of the stomach, under the guidance a 34-Fr bougie dilator. The initial stapling started at the antrum, approximately 4 cm from the pyloric ring. Care was taken during stapling to maintain a sufficient distance from incisura angularis and the angle of His to prevent strictures or high leak after surgery. The staple line was selectively reinforced with either an interrupted or continuous oversewing method, especially where bleeding persisted or the staples overlapped.
Patients initiated oral intake in the morning of the first postoperative day and were discharged once they achieved adequate oral intake, their pain was controlled, and they were ambulating without difficulty. The postoperative nutritional regimen consisted of a liquid or soft diet for the first 3 weeks with gradual increases in food texture, thereafter. Patients returned to the outpatient clinic 2 weeks after surgery and then every 3 months for the first postoperative year for monitoring of weight loss, appetite, dysphagia or food intolerance, eating behavior, comorbidity status, and the presence of any complications. Follow-up was decreased to every 12 months after the first year. Telephone interviews were used to monitor patients who could not visit the outpatient clinic.
The degree of weight loss was assessed using percent excess weight loss (%EWL) and percent excess BMI loss (%EBMIL), which were calculated using the following formulas:
The ideal weight was calculated using a formula corresponding to the midpoint of the medium frame of the Metropolitan Tables [10]. The %EBMIL was calculated using a BMI of 23 kg/m2 as the upper limit of normal, according to the World Health Organization (WHO) recommended definition of obesity among Asians [11].
The diagnosis of type 2 diabetes was made according to the criteria established by the American Diabetes Association (fasting blood glucose [FBS] ≥ 126 mg/dL or hemoglobin A1c [HbA1c] level ≥ 6.5%), whereas the criteria for diabetic remission were defined as FBS < 126 mg/dL and HbA1c < 6.5% without the postoperative use of any antidiabetic medications (oral hyperglycemic agents or insulin). We defined dyslipidemia as the presence of one or more abnormalities in serum triglyceride (≥150 mg/dL) or high-density lipoprotein (<40 mg/dL) levels or treatment for the condition. Hypertension was diagnosed when the patient was receiving treatment for the condition. Remission of dyslipidemia and hypertension were defined, respectively, as normal lipid panel results and normal blood pressure values without medication. Sleep apnea was considered to belong to one of two groups: treatment for the condition, including overnight continuous positive airway pressure support (confirmed diagnosis), or subjective symptoms strongly suggestive of sleep apnea, but not yet treated (suspicious diagnosis).
All statistical analyses were performed using PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA). Means with standard deviations or medians with ranges were calculated. The chi-square test or Fisher exact test was used to analyze categorical variables, whereas the Mann-Whitney U-test was used for continuous variables. All tests were two-tailed and P-values < 0.05 were considered significant.
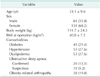
A total of 192 patients underwent LSG during the study period. The patient population comprised 61 men (31.8%) and 131 women (68.2%). Their mean preoperative BMI was 40.0 ± 7.2 kg/m2 and most of the patients (120/192, 62.5%) had one or more obesity-related comorbidities. The most common comorbid conditions were hypertension (27.6%) and dyslipidemia (27.6%), followed by diabetes (21.4%); detailed preoperative demographic data are shown in Table 1.
The mean operative time was 104.4 ± 28.1 minutes and an average of seven laparoscopic linear stapler cartridges was consumed to complete each gastric resection (Table 2). Eight patients (4.2%) underwent concomitant cholecystectomy due to concurrent gallbladder stones detected during preoperative evaluations. Although intraoperative bleeding was noted in two patients, one from a splenic injury and the other from a trocar insertion site, they were well managed, laparoscopically; neither required conversion to open surgery. Patients were discharged on the second postoperative day on average; surgical mortalities did not occur.
Surgical complications developed in 24 patients (12.5%; Table 3). Most (19/192, 9.9%) were related to surgical wound or stasis symptoms and were successfully managed with conservative treatment. Two patients developed moderately severe complications, one patient who required prolonged proton pump inhibitor use due to persistent reflux symptoms and one who was readmitted on postoperative day 9 with a chief complaint of persistent vomiting. A contrast upper gastrointestinal study in the patient with persistent vomiting revealed passage disturbance attributable to kinking of the gastric tube; this distal obstruction, in turn, resulted in a microleak at the proximal end of the staple line. The patient was managed with fasting and a 3-week course of antibiotic therapy; the patient was subsequently discharged without further events. Three patients (1.6%) required invasive intervention for severe complications. Two developed postoperative bleeding with deteriorating vital signs that required emergent reoperations. The bleeding foci were the staple line in one patient and the trocar insertion site in the other patient. Successful laparoscopic hemostasis was accomplished in both patients and they were discharged, without further complications, on postoperative day 4. The third patient developed a staple line leak on postoperative day 1, and required two reoperations and further endoscopic interventions. The patient was discharged on postoperative day 82, after confirming the absence of further leakage.
The patients' mean BMI decreased from 40.1 ± 7.2 to 29.0 ± 5.5 kg/m2 during a mean follow-up period of 25 months. The postoperative BMI and %EWL at each follow-up time point are shown in Table 4. The mean 1-year %EWL and %EBMIL values were 72.6% ± 25.1% and 74.6% ± 26.7%, respectively. The %EWL peaked 24 months postoperatively at 80.6% ± 19.8%, and gradually decreased thereafter. Twenty-six patients (13.5%) failed to achieve a %EWL of ≥50% within the first postoperative year, and 3 (1.6%) showed %EWL of <30% at that time point.
The resolution of weight-associated comorbidities was observed in most patients after a mean follow-up period of 25 months (Table 5). Diabetes was resolved in 81.9% of the patients, with these patients being able to maintain HbA1c levels <6.5%, without the use of any antidiabetic medications. More than 70% of the patients with hypertension and dyslipidemia also discontinued their medications after the surgery.
Nine patients (4.7%) required revisional surgery for several reasons (Table 6). Four reported persistent reflux symptoms requiring prolonged proton pump inhibitor use; endoscopic evaluation revealed severe reflux esophagitis. One patient suffered from intractable diabetes, despite sufficient post-LSG weight loss (111.8% of EWL) and decided to undergo revisional surgery with a malabsorptive component. RYGB was adopted as a revisional procedure in all patients and all revisional procedures were successfully performed laparoscopically.
This study included a relatively large number of Korean patients who underwent LSG at a single specialized center and demonstrated outcomes after up to 4 years of follow-up. Since bariatric surgery in Asian countries is relatively new, there are only a few literatures available that evaluated the medium-term outcomes of LSG in obese patients from Far East Asia [12]. We believe that this study would provide valuable information on the efficacy of LSG in Asian obese patients.
Since LSG has become a stand-alone procedure for weight loss, the number of annual LSG procedures performed, world-wide, has exponentially increased over the last few years [13]. This can be mostly attributed to the decrease the in number of adjustable gastric banding procedures, which are associated with frequent long-term complications. Buchwald and Oien [13] also speculated that the global popularity of LSG might be faddism, with surgeons gravitating towards the latest surgical option.
The trend towards LSG is more pronounced in the Asia-Pacific region, where these procedures have increased more than 20 folds from 2008 to 2011, with LSG now accounting for >50% of all bariatric procedures [13]. Several reasons may account for this enthusiasm, particularly in Asian countries. First, LSG is a less demanding surgical technique than RYGB or BPD/DS, and it requires a shorter learning curve [14]. Because the incidence of morbid obesity is much lower in Asian countries than in Western countries, surgeons are less experienced with bariatric procedures. The risk of surgical complications following LSG is also reported to be lower than the risk associated with RYGB or BPD/DS [15]. Therefore, this less aggressive approach has been widely advocated in Asian countries. Further, Asian patients seem to have relatively low BMI values; hence, stand-alone LSG is considered to be sufficient to achieve satisfactory weight loss outcomes. Furthermore, the high incidence of gastric cancer in Asian countries makes surgeons and patients hesitate to choose RYGB because regular endoscopic surveillance of the excluded stomach would be impossible following RYGB. The patients enrolled in the current study chose to undergo LSG for various reasons, including as part of a staged operation in superobese patients or as a stand-alone procedure in relatively low BMI patients. In contrast, a family history of gastric cancer, a fear of gastric cancer, liver cirrhosis in hepatitis virus carriers who might be eligible for liver transplantation, and other reasons were stated by patients not choosing LSG. As mentioned above, regional characteristics have a large influence on the selection of LSG.
Surgical complications occurred in 12.5% of patients in the current study. Among these, severe complications requiring invasive intervention comprised 1.6% of the complications (leakage, 0.5%; bleeding, 1.0%), comparable to rates reported in previous LSG studies and slightly lower than those associated with RYGB [15,16,17]. Short-term complications are relatively infrequent after LSG because of the procedure's technical simplicity, compared with RYGB or BPD, but risks of surgical complications involving the long stapler line remain. Most of all, leakage at the staple line near the esophagogastric junction, the so-called high leak, is very difficult to manage. According to the published literature, leaks occur in 0%-7% of LSG cases, and the risk seems to increase in super-obese patients [16]. One patient in our study developed a high leak in the early postoperative period and required two reoperations for primary repair with external drainage and repeated endoscopic stent insertions due to persistent leakage from the uppermost end of the stapler line. The leakage was successfully controlled following approximately 3 months of in-hospital treatment, but the required prolonged fasting and parenteral nutrition resulted in a thiamine deficiency and subsequent long-term neurologic sequelae (Wernicke syndrome). This patient's detailed clinical course is described elsewhere [18]. An endoscopically placed stent, which is reported to achieve successful outcomes in some carefully selected patients with leakage, was ineffective in this patient due to repeated migration. If the migration issue can be overcome, stenting might provide the advantage of allowing patients to resume oral intake while the leak heals. Otherwise, patients benefit nutritionally from a surgically inserted feeding jejunostomy when lengthy fasting is anticipated [19].
Kinking of the gastric tube could be another staple line-associated problem that results in a functional distal obstruction. This presents as persistent dysphagia with nausea and vomiting associated with consumption of either solids or liquids. In the current study, this functional obstruction in one patient eventually led to a delayed microleak from the proximal staple line. A bare staple line, adhering to the surrounding tissue, or an inadequately narrow lumen at the incisura could have resulted in angulation of the staple line.
In the current study, the entire staple line of each patient was reinforced with continuous oversewing further to complications encountered in earlier patient series. However, recent studies suggest that oversewing, or buttressing, of the staple line does not have a clinically significant effect on postoperative complications [20]. Given the recent advancements in laparoscopic stapling instruments, the proper utilization of staplers becomes important, through the proper choice of staple height, ensuring good staple formation, allowing time for tissue compression, avoiding a stricture by not stapling too close to the incisura, and avoiding a high leak by stapling away from the gastroesophageal junction [16,21].
The most commonly used metric for measuring weight loss is %EWL, calculated from the ideal body weight based on the Metropolitan Life Insurance Company height/weight table [22]. However, this table is based on several-decades-old data from North American populations and does not consider racial differences. The WHO suggested that a lower cutoff value should be adopted for the diagnosis of obesity for the Asia-Pacific region [11]. Therefore, we presented our outcomes as %EWL, based on the Metropolitan Life table using a mean medium-frame weight for determining the ideal body weight; %EBMIL was calculated using a benchmark BMI of 23 kg/m2 as the upper limit of normal. Based on these calculations, the mean %EWL and %EBMIL in the present study were 66.5% and 68.3% at a mean follow-up time of 25 months; these values are comparable to previously published results. The current study showed that patients who underwent LSG were susceptible to weight regain after more than 2 years, although the number of patients continuing in the follow-up study had decreased markedly, and became too small, by year 4, to draw definitive conclusions. However, this finding is consistent with those of previous studies on LSG or other purely restrictive procedures; most consistently report that weight regain might eventually be observed after LSG [23,24]. Himpens et al. [24] suggested that dilatation of the sleeved stomach along with neo-fundus formation allows the patient to consume larger meals and induces weight regain. Gradual loss of the "appetite suppression effect" following fundic resection has also been cited as being partly responsible for the delayed weight regain after LSG [25]. The patients in the present study need to be followed up for much longer periods to determine whether a tendency to regain weight persists.
As previously published studies have already demonstrated, gastroesophageal reflux disease (GERD) is a major concern after LSG. Four of our 192 patients (2.1%) requested revisional surgery due to intolerable reflux symptoms requiring prolonged proton pump inhibitor use or due to poor responses to other acid suppression therapies. Two patients showed severe (grade C or worse, based on the Los Angeles classification) reflux esophagitis. Although the overall incidence of de novo, post-LSG GERD was not precisely evaluated in the current study, incapacitating GERD seems to be a major reason for LSG revision following insufficient weight loss. The Fourth International Consensus Summit for Sleeve Gastrectomy surveyed attendees on the prevalence of postoperative GERD and found that it was 0%-30% [26]. LSG might promote or worsen GERD in various ways. Reduced pressure on the lower esophageal sphincter could be caused by excessive dissection around the angle of His. This could also result from reduced gastric compliance and increased gastric pressure [27]. Furthermore, crus repair was not routinely performed in the current study cohort. When LSG is planned as a stand-alone procedure, the possibility of new or recurrent reflux symptoms should be considered. Hiatal hernias should be identified intraoperatively and the crus should be appropriately closed to minimize de novo GERD-induced surgical failure [21].
Recently, numerous studies have demonstrated promising results for stand-alone LSG-derived EWL and resolution of comorbid conditions during the short to medium term [12,14,17,23,24]. The present study also demonstrated promising midterm outcomes in terms of both weight loss and comorbidity resolution. The associated revision rate of 4.7% is considered acceptable. However, the tendency for weight regain after 2 years and the development of de novo GERD casts doubt on the durable efficacy of LSG. In addition, 13.5% of the patients did not achieve successful weight loss, defined as %EWL ≥50% within 1 year. Since the rate of weight loss markedly decreases and plateaus after 1 year, and given the possibility of weight regain after 2 years, this population might require revisional procedures for weight loss failure. A recently published systematic review also concluded that LSG results in satisfactory long-term weight loss, but the number of analyzed patients was small [28]. A larger cohort of patients is necessary to validate the effectiveness of LSG compared to other well established bariatric procedures, 10 or more years postoperatively. Whether the current popularity of LSG will endure or whether the procedure will be relegated to the status of a surgical fad remains to be seen.
In conclusion, LSG can be performed safely, with an acceptable risk of surgical complications, and provides effective weight loss and considerable comorbidity resolution at midterm follow-ups. However, longer follow-up periods are necessary to elucidate whether LSG achieves sustainable weight loss outcomes, comparable to those of more aggressive procedures.
Figures and Tables
Table 4
Anthropometric outcomes following sleeve gastrectomy at each time point

Values are presented as mean ± standard deviation unless otherwise indicate.
BMI, body mass index; EWL, excess weight loss; EBMIL, excess BMI loss.
a)A BMI of 23 kg/m2 was adopted as the upper limit of normal to calculate %EBMIL according to the World Health Organization recommended definition of obesity for Asians.
ACKNOWLEDGEMENTS
Min Ju Soh supported this study as a research coordinator. This research was supported by the Soonchunhyang University Research Fund.
References
1. Marceau P, Biron S, Bourque RA, Potvin M, Hould FS, Simard S. Biliopancreatic Diversion with a New Type of Gastrectomy. Obes Surg. 1993; 3:29–35.
2. Scopinaro N, Gianetta E, Civalleri D, Bonalumi U, Bachi V. Two years of clinical experience with biliopancreatic bypass for obesity. Am J Clin Nutr. 1980; 33:2 Suppl. 506–514.
3. Marceau P, Biron S, Hould FS, Lebel S, Marceau S, Lescelleur O, et al. Duodenal switch: long-term results. Obes Surg. 2007; 17:1421–1430.
4. Ren CJ, Patterson E, Gagner M. Early results of laparoscopic biliopancreatic diversion with duodenal switch: a case series of 40 consecutive patients. Obes Surg. 2000; 10:514–523.
5. Regan JP, Inabnet WB, Gagner M, Pomp A. Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg. 2003; 13:861–864.
6. Cottam D, Qureshi FG, Mattar SG, Sharma S, Holover S, Bonanomi G, et al. Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity. Surg Endosc. 2006; 20:859–863.
7. Mognol P, Chosidow D, Marmuse JP. Laparoscopic sleeve gastrectomy as an initial bariatric operation for high-risk patients: initial results in 10 patients. Obes Surg. 2005; 15:1030–1033.
8. Baltasar A, Serra C, Perez N, Bou R, Bengochea M, Ferri L. Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg. 2005; 15:1124–1128.
9. Kasama K, Mui W, Lee WJ, Lakdawala M, Naitoh T, Seki Y, et al. IFSO-APC consensus statements 2011. Obes Surg. 2012; 22:677–684.
10. 1983 Metropolitan height and weight tables. New York: Metropolitan Life Insurance Company;1983.
11. World Health Organization Western Pacific Region, IASO International Association for the Study of Obesity, International Obesity Taskforce. The Asia-Pacific perspective: redefining obesity and its treatment. Geneva: World Health Organization;2000.
12. Zachariah SK, Chang PC, Ooi AS, Hsin MC, Kin Wat JY, Huang CK. Laparoscopic sleeve gastrectomy for morbid obesity: 5 years experience from an Asian center of excellence. Obes Surg. 2013; 23:939–946.
13. Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013; 23:427–436.
14. Prevot F, Verhaeghe P, Pequignot A, Rebibo L, Cosse C, Dhahri A, et al. Two lessons from a 5-year follow-up study of laparoscopic sleeve gastrectomy: persistent, relevant weight loss and a short surgical learning curve. Surgery. 2014; 155:292–299.
15. Boza C, Gamboa C, Salinas J, Achurra P, Vega A, Perez G. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy: a case-control study and 3 years of follow-up. Surg Obes Relat Dis. 2012; 8:243–249.
16. Aurora AR, Khaitan L, Saber AA. Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc. 2012; 26:1509–1515.
17. Trastulli S, Desiderio J, Guarino S, Cirocchi R, Scalercio V, Noya G, et al. Laparoscopic sleeve gastrectomy compared with other bariatric surgical procedures: a systematic review of randomized trials. Surg Obes Relat Dis. 2013; 9:816–829.
18. Jeong HJ, Park JW, Kim YJ, Lee YG, Jang YW, Seo JW. Wernicke's encephalopathy after sleeve gastrectomy for morbid obesity: a case report. Ann Rehabil Med. 2011; 35:583–586.
19. Tan JT, Kariyawasam S, Wijeratne T, Chandraratna HS. Diagnosis and management of gastric leaks after laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010; 20:403–409.
20. Chen B, Kiriakopoulos A, Tsakayannis D, Wachtel MS, Linos D, Frezza EE. Reinforcement does not necessarily reduce the rate of staple line leaks after sleeve gastrectomy. A review of the literature and clinical experiences. Obes Surg. 2009; 19:166–172.
21. Rosenthal RJ. International Sleeve Gastrectomy Expert Panel. Diaz AA, Arvidsson D, Baker RS, Basso N, et al. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of > 12,000 cases. Surg Obes Relat Dis. 2012; 8:8–19.
22. Deitel M, Gawdat K, Melissas J. Reporting weight loss 2007. Obes Surg. 2007; 17:565–568.
23. Eid GM, Brethauer S, Mattar SG, Titchner RL, Gourash W, Schauer PR. Laparoscopic sleeve gastrectomy for super obese patients: forty-eight percent excess weight loss after 6 to 8 years with 93% follow-up. Ann Surg. 2012; 256:262–265.
24. Himpens J, Dobbeleir J, Peeters G. Longterm results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010; 252:319–324.
25. Karamanakos SN, Vagenas K, Kalfarentzos F, Alexandrides TK. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg. 2008; 247:401–407.
26. Gagner M, Deitel M, Erickson AL, Crosby RD. Survey on laparoscopic sleeve gastrectomy (LSG) at the Fourth International Consensus Summit on Sleeve Gastrectomy. Obes Surg. 2013; 23:2013–2017.
27. Chiu S, Birch DW, Shi X, Sharma AM, Karmali S. Effect of sleeve gastrectomy on gastroesophageal reflux disease: a systematic review. Surg Obes Relat Dis. 2011; 7:510–515.
28. Diamantis T, Apostolou KG, Alexandrou A, Griniatsos J, Felekouras E, Tsigris C. Review of long-term weight loss results after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2014; 10:177–183.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download