Abstract
Anastomotic leakage following rectal resection is a serious and fearful complication, and may cause presacral abscess and/or peritonitis. To our knowledge, massive hematochezia secondary to presacral abscess caused by anastomotic leakage has not yet been reported in the literature. We observed this rare and life-threatening complication in three patients who were successfully treated with a simple but effective transanal gauze packing technique.
Anastomotic leakage is a main cause of morbidity and mortality following rectal resection [1]. Presacral abscess is a well-known consequence of leakage. However, to our knowledge, massive hematochezia secondary to presacral abscess caused by anastomotic leakage has not yet been reported. Here, we report three patients who developed life-threatening hematochezia and were successfully treated with a simple but effective transanal gauze packing technique.
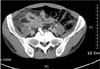
A 60-year-old man with rectal cancer located 10 cm from the anal verge (AV) underwent robotic low anterior resection (LAR) with double-stapled end-to-end anastomosis. On postoperative day (POD) 3, the patient developed fever (39.0℃), vague low abdominal pain, and the color of the pelvic drain changed. Abdominopelvic CT confirmed anastomotic leakage with perianastomotic abscess confined to the pelvic cavity (Fig. 1). CT-guided transgluteal percutaneous drainage was performed but fever and abdominal pain was not improved. On the following day, diverting ileostomy with peritoneal lavage was performed by a relaparoscopic approach and an additional pelvic drain was placed. Twelve days after the reoperation, the transgluteal drainage catheter was removed because the presacral abscess cavity shrunk on abdominopelvic CT. On POD 21, the patient suddenly developed massive hematochezia (900 mL). Sigmoidoscopy failed to identify the bleeding site because of a large amount of bleeding and hematoma.
The patient was urgently brought to an operating room and placed in the lithotomy position under local perianal block. When an anal retractor was inserted into the anal canal to expose the anastomotic site, a large amount of blood gushed out from the presacral space through a tissue disruption on the posterior anastomotic line. Even after evacuation of the hematoma and saline irrigation, individual clipping or suturing to control the bleeding was not possible because of diffuse and massive hemorrhage from the presacral space. Therefore, several pieces of Spongostan (an absorbable gelatin tissue hemosealant) and rolls of Vaseline-coated gauze (Fig. 2) were packed into the presacral space until hemostasis (Fig. 3). The tip of the rolled gauze was brought out through the anus for easy removal later. No further bleeding was noted in the anus after this procedure.
Five days later, the patient was brought to the operating room to remove the previously inserted rolled Vaseline gauze. However, after removal of the gauze, bleeding occurred again, and therefore, the same procedure of gauze packing was repeated. One week later, the Spongostan pieces and rolled Vaseline gauze were removed in the same manner, after which there was still oozy bleeding. The same procedure was followed again and no further bleeding was noted after one week. He was discharged on POD 49.
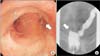
Three months later, the patient underwent sigmoidoscopy. The anastomotic site showed good healing without stricture, sinus, or fistula tract formation (Fig. 4). After closure of the stoma, the patient was stable with no recurrence of the presacral abscess.
A 34-year-old man was referred to our surgical department with a diagnosis of ileosigmoid fistula due to Crohn disease. Although colonic dilatation and accumulation of impacted feces in the colon were noted on abdominopelvic CT, mechanical bowel preparation was not possible because laxatives bypassed the colon through the fistula between the terminal ileum and sigmoid colon (Fig. 5). We performed a laparoscopic anterior resection with double-stapled end-to-end anastomosis and ileocecectomy with side-to-side anastomosis, rather than total abdominal colectomy, to improve functional outcomes.
Two days after the operation, the patient developed abdominal pain, and the color of the pelvic drain changed after loose stools occurred. He underwent an emergency laparoscopic exploration, which revealed dirty fluid collection in the whole abdomen, a distended proximal colon filled with feces, and a posterior defect on colorectal anastomosis. After copious peritoneal irrigation, on-table colonic lavage was performed through the anus after the defect was packed with gauze. Then a protective ileostomy was made and a sump drainage catheter was placed posterior to the anastomosis. The next day, the sump drainage catheter was plugged with feces, and the abdominal pain was aggravated. The patient underwent laparoscopic irrigation and colonic lavage once again.
On POD 8, active fresh bleeding developed from both the anus and the sump drainage. The patient was placed in the lithotomy position under local anesthesia, as described above in case 1. After transanal irrigation, Spongostan and rolled gauze were packed into the presacral space through the anastomotic defect. At the same time, the sump drainage was removed to make gauze packing more effective. After 6 days, the rolled gauze was removed at bedside, and no more bleeding was noted. He was discharged on POD 23. The patient showed good recovery except the development of an enterocutaneous fistula from the anastomotic defect to the sump drainage site on the low abdominal wall. After 14 months, he underwent reresection and reanastomosis to treat the enterocutaneous fistula.
A 75-year-old man with rectal cancer (6 cm from the AV) and early gastric cancer (antrum, greater curvature) underwent robotic ultra-LAR with diverting ileostomy and laparoscopic distal gastrectomy simultaneously. On POD 2, the patient developed abdominal pain and leukocytosis (23,800/µL), and the color of the pelvic drain changed. Digital rectal examination showed anastomotic disruption posteriorly. Because the patient showed no signs of generalized peritonitis, a rubber rectal tube was inserted into the presacral space through the defect under the guidance of the index finger. After the abscess was drained, abdominal pain and leukocytosis improved. A gentle saline irrigation through the rectal tube was performed twice per day till POD 7 when purulent content was no longer drained.
On POD 14, hypotension (80/60 mmHg) and massive hematochezia developed abruptly. The patient underwent emergency surgery under local anesthesia. Transanal irrigation and Spongostan and rolled gauze packing were performed sequentially. No further bleeding was noted after the packing was removed two days later. The patient was discharged on POD 53 because of poor oral intake due to delayed gastric emptying.
Six months later, sigmoidoscopy showed a small sinus at the disruption site with no stricture formation (Fig. 6). He underwent ileostomy closure and defecation was tolerable without recurrence of presacral abscess thereafter.
The presacral venous plexus courses into the pelvic fascia that covers the anterior aspect of the sacrum. During pelvic surgery, injury to the pelvic fascia may result in massive bleeding from the presacral venous plexus and sometimes it is fatal [2]. In the three cases of this report, mesorectal excision was performed along the avascular "holy plane," and presacral bleeding was not noted during the surgery. Therefore, we believe that pelvic fascia and vessel wall erosion due to presacral abscesses can cause massive bleeding. Vessel wall erosion due to intraabdominal abscess formation after pancreatic surgery is known to cause delayed massive bleeding [3].
Traditional methods for bleeding control include pelvic packing and the use of metallic thumbtacks [4,5]. Pelvic packing has the disadvantage of reoperation for removal of packing and risk of rebleeding. Thumbtacks are ineffective for diffuse bleeding and can be displaced resulting in chronic pain, anastomosis disruption, and anastomotic fistula [6]. Other methods include the use of bone wax and the coagulation or suturing of the bleeding focus with muscle fragments. We did not performed these methods for bleeding control because these methods require abdominal laparotomy under general anesthesia and access to the pelvic cavity after anastomotic leakage may cause additional damage to the anastomosis and the surrounding organs. Presacral abscesses secondary to low rectal anastomotic leakage are usually extraperitoneal and confined by the surrounding organs. Therefore, presacral bleeding does not accumulate in the intraperitoneal space, and transanal gauze packing can be a simple and effective technique for controlling bleeding in these cases. Moreover, this technique is safe and does not require general anesthesia and exploration of the abdominal cavity.
We used Spongostan and rolled Vaseline gauze for packing, and the tip of the gauze was brought out through the anus. By pulling the tip, the gauze was easily removed through the anus because the Vaseline prevented the gauze from adhering to the tissue. Spongostan, which may serve as a nidus of infection, was easily washed out during transanal irrigation.
Figures and Tables
References
1. Karanjia ND, Corder AP, Holdsworth PJ, Heald RJ. Risk of peritonitis and fatal septicaemia and the need to defunction the low anastomosis. Br J Surg. 1991; 78:196–198.
2. Wang QY, Shi WJ, Zhao YR, Zhou WQ, He ZR. New concepts in severe presacral hemorrhage during proctectomy. Arch Surg. 1985; 120:1013–1020.
3. de Castro SM, Kuhlmann KF, Busch OR, van Delden OM, Lameris JS, van Gulik TM, et al. Delayed massive hemorrhage after pancreatic and biliary surgery: embolization or surgery? Ann Surg. 2005; 241:85–91.
4. Zama N, Fazio VW, Jagelman DG, Lavery IC, Weakley FL, Church JM. Efficacy of pelvic packing in maintaining hemostasis after rectal excision for cancer. Dis Colon Rectum. 1988; 31:923–928.
5. Nivatvongs S, Fang DT. The use of thumbtacks to stop massive presacral hemorrhage. Dis Colon Rectum. 1986; 29:589–590.
6. Germanos S, Bolanis I, Saedon M, Baratsis S. Control of presacral venous bleeding during rectal surgery. Am J Surg. 2010; 200:e33–e35.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download