Abstract
Benign cystic mesothelioma is an uncommon tumor arising from the peritoneal mesothelium. It is characterized by multilocular grapelike, thin-, and translucent-walled cysts, or a unilocular cyst lined by benign mesothelial cells. It occurs predominantly in women of reproductive age, and shows a predilection for the surface of the pelvic peritoneum or visceral peritoneum. Patients usually present abdominal pain and palpable mass, but many cases have been found incidentally during laparotomy. Definite preoperative diagnosis is known to be difficult. Benign cystic mesothelioma has a tendency towards local recurrence, although the gross microscopic features are benign. Moreover, there is controversy over whether this disease is neoplastic or reactive. Initial complete surgical resection and cytoreductive surgery for recurred cases are standard treatments. In the following report, we describe a case of complicated benign cystic mesothelioma in a postpartum woman, involving the pelvic peritoneum and mesoappendix, which was initially misdiagnosed as a periappendiceal abscess.
Benign cystic mesothelioma (BCM) is a rare tumor arising from endothelial cells of the visceral or parietal peritoneum [1]. The most common sites of the disease are serosal surfaces of the ovary, uterus, rectum and pelvic peritoneum [2]. BCM occurs more frequently in young to middle-aged women, with 17% of cases found in men [1,3,4]. Most patients are diagnosed without specific symptoms, but some patients have a palpable abdominal mass, pain, urinary urgency, and/or uterine bleeding [1,2]. Once diagnosed, the tumor should be surgically removed completely, because the recurrence rate is known to be high, although the tumor has a benign nature. However, it is difficult to make an initial diagnosis, and this diagnosis is usually not conclusive with routine pathological examination [1]. Although the tumor is benign, it has the potential for malignant transformation, and there has been a report of death from the disease in an untreated patient, 12 years after diagnosis [4]. Furthermore, there have only been a few cases reported of this rare disease that involved the appendix [1,5,6]. In the following study, we report a case of BCM in a 27-year-old patient, involving the mesoappendix and pelvic parietal peritoneum, which were misdiagnosed as a periappendiceal abscess during the postpartum period.
A 27-year-old female was referred to Eulji General Hospital with right lower quadrant abdominal pain, tenderness, and fever for two days. Two weeks prior to her visit, she had delivered a healthy baby after an intrauterine period of 40 weeks. She had no past medico-surgical history. Due to the above symptoms, an abdomino-pelvic CT scan was taken at the previous hospital. She was referred to us with the possible diagnosis of a periappendiceal abscess or a ruptured mucocele of the appendix.
On examination, her vital signs were normal, except for a mild fever of 37.9℃. A physical examimation revealed tenderness in the right iliac fossa, with slightly distended abdomen. No serological abnormalities, including white blood cell count (9,690/mm3), were noted before the operation. Urine analysis was also negative. A CT scan showed complicated fluid collection or early abscess formation in the cecum base, but no definite evidence of an inflamed appendix and mesenteric lymphadenopathy (Fig. 1A, B). The uterus was heterogeneously enhanced, probably due to the recent delivery. In addition, numerous variable-sized (maximum 5 mm in diameter) low attenuation lesions in both lobes of the liver were found, which were suspicious for biliary hamartomas. Multiple small cysts in both kidneys were also noted. Emergency diagnostic laparoscopy and appendectomy were performed on the day of admission.
For the surgery, the patient was placed in the supine position. Three trocars were used; a 12-mm port for the camera was placed below the umbilicus, and two 5-mm trocars were used at the left lower quadrant and suprapubic area. After pneumoperitoneum was established, the whole abdomen was thoroughly inspected, and a multiloculated, translucent, cystic mass was found around the cecal base (Fig. 2A). The cecum and appendix were mildly inflamed and adhered to this cystic mass. The mass was easily separated from the cecum and was found to involve the parietal peritoneum and mesoappendix (Fig. 2B). The involved peritoneal wall and appendix were resected en bloc to remove the whole lesion (Fig. 2C-E). However, the margin was not distinct from normal tissue, so complete excision was not possible. Fig. 2F shows that the lesion was connected to the mesoappendix of the tip of the appendix after peritoneal excision. During dissection, the cysts were inevitably ruptured. The content of the cysts, which seemed to be clear lymphatics, was drained into the pelvic cavity. The size of the appendix was 7.5 cm in length and 0.7 cm in external diameter, with attached pinkish-gray fibroadipose tissue, 6.0 cm × 3.5 cm × 1.5 cm in size, at the tip of the mesoappendix.
On microscopic examination, there were multiple cystic spaces containing semitransparent watery fluid, with fibrous walls, including chronic inflammatory cells (Fig. 3A, B). The differential diagnosis was cystic lymphangioma, endometriosis, and cystic mesothelioma. Immunohistochemical analyses were positive for Calretinin and D2-40 (a marker of lymphatic endothelium), but negative for CD10 and estrogen receptor, which excluded endometriosis and cystic lymphangioma, and the disorder was diagnosed as BCM (Fig. 3C). The appendix showed serositis with congestion and previous hemorrhaging. The postoperative course was uneventful, and the patient was discharged five days after surgery. She refused further surgical treatment and remained free of recurrence during the 18 months of follow-up.
BCM is a rare but well-known disease. It has also been referred to as multicystic peritoneal mesothelioma, multilocular cysts of the peritoneum, multicystic mesothelioma, and multicystic peritoneal inclusion cysts [1,2]. Mesothelioma is a neoplasm that originates from the mesothelial cell lining of the serosal membranes of body cavities [2]. It mainly arises from the serosal surface of the ovary, uterus, bladder, rectum, and pelvic peritoneum, and can also develop from the pleura, spermatic cord, tunica vaginalis, and pericardium [2]. Cystic mesothelial proliferation was first described by Plaut (quoted from [5]) in 1928, but could only be pathologically differentiated from other diseases after its ultrastructure was characterized by electron microscopy [1]. Recently, BCM has been accurately diagnosed using immunohistochemical staining [4].
Its etiology is presently unclear, and its pathogenesis as a reactive or neoplastic disease is still controversial. It is usually considered an inflammatory process, because most common predisposing factors involve a previous history of pelvic inflammatory disease, endometriosis, and abdominal surgery, which could result in inhibition of peritoneal reabsorption [2]. However, because of its recurrence, some clinicians consider it a neoplastic disease. In this regard, several malignant transformations have been described in the literature [2,3,4,5]. A recent case study reported seven recurrences, which finally resulted in malignant transformation after repeated surgical removal [4]. In addition, a study showed that 45%-50% of cases involving BCM had local recurrences with a mean interval of 32 months (4 months-7 years) after the initial surgical treatment [7].
BCM occurs five times more often in women than in men [5]. The mean age of patients is 37-38 years at the time of diagnosis [5]. Most patients present acute or chronic abdomen/pelvic discomfort, and palpable masses in the abdomen. However, BCM has also been found incidentally during imaging or laparotomy. Patients with BCM had a previous history of abdominal operations (42%), pelvic inflammatory disease (14%), or endometriosis (7%) [8].
BCM in the appendix or mesoappendix has been rarely reported [6]. As in the present case, only a few cases have reported a thin-walled, multiseptated serous cyst, which was grossly attached to the tip of the mesoappendix or involved visceral and parietal layers of the peritoneum in the appendiceal region, which were finally diagnosed as BCM by immunohistochemical staining [5,6]. Regarding the association with pregnancy, a study reported that BCM was found around the infundibulopelvic ligament during a cesarean section in a 26-year-old female [8]. BCM is believed to be hormone-sensitive, which is consistent with the predilection for the disease in reproductive age women [9].
As shown in the present case, preoperative imaging can show the lesions, but cannot discriminate them from other cystic lesions. Furthermore, aspiration biopsy of the lesion is not definitive. For accurate diagnosis, exploratory laparotomy or laparoscopy is required for the biopsy of the suspected tissues. As shown in the present case, a single layer of flattened mesothelial cells, often with a hobnail configuration, is a characteristic microscopic finding [1,3]. The walls of BCM are infrequently found in smooth muscle and in features of the lymphatic system [1,3]. However, because histolological findings as well as the clinical presentation are similar to other differential diagnoses, positive immunohistochemical staining of epithelial cells for calretinin, which is consistent with mesothelial differentiation and electron microscopy, is required for an accurate diagnosis [1,2,3]. Differential diagnosis among benign diseases includes lymphangioma, endometriosis, cystic adenomatoid tumors, and cystic mesonephric duct remnants. Furthermore, lymphangiomas are often confused on the basis of their gross appearance, but are correctly diagnosed based on their histology and ultrastructural characteristics [3,4].
There is no standard treatment for BCM. However, whenever possible, complete excision should be performed [1,2]. As shown in the present case, if curative resection is not possible for various reasons, an extensive curative second operation is needed to prevent transition of BCM to a malignant disease. Sclerotherapy, continuous hyperthermic peritoneal perfusion, and cytoreductive surgery with intraperitoneal chemotherapy have been shown to be effective [10]. In addition, there has been a report of positive reductions in tumor volume after treatment with tamoxifen and long-acting GnRH analogs [9]. Furthermore, because of the probable influence of female sex hormones in the etiology of this tumor, patients may benefit from a hypoestrogenic state [9].
In conclusion, BCM does not involve a standard treatment, and there is a lack of long-term outcomes of patients with this disorder. Because of its tendency to recur and because of its malignant potential, repeated and complete surgical removal together with a careful long-term follow-up, are required for the optimal prognoses of patients.
Figures and Tables
Fig. 1
Abdominopelvic CT scan showing lobulating contoured fluid collection, with high density and mild peripheral enhancement, abutting the cecal base (white arrow). The images involved possible complicated fluid collection or early abscess formation. (A) Axial image, (B) coronal image.
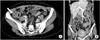
Fig. 2
Intraoperative findings by laparoscopy. (A) Inflamed, multiloculated, translucent cystic mass in the right iliac fossa. (B) Cystic mass was detached from the cecal base. The lesion is mainly located in the abdominal parietal peritoneum, and connected to the mesoappendix of the tip of the appendix. (C) The involved parietal peritoneum was excised with a monopolar energy device. (D) The lesion was not clearly separated from the normal peritoneal tissue. (E) The involved peritoneal wall in the right iliac fossa was excised. (F) The lesion including the appendix was resected en bloc.

Fig. 3
Pathologic findings of the biopsies. (A) The cysts were surrounded by a thick fibrous wall containing chronic inflammatory cells (H&E, ×40). (B) Thin-walled cysts showed flattened or activated mesothelial linings (H&E, ×200). (C) Thick-walled cyst was positive for calretinin immunostaining (×100).

Notes
References
1. O'Connor DB, Beddy D, Aremu MA. Benign cystic mesothelioma of the appendix presenting in a woman: a case report. J Med Case Rep. 2010; 4:394.
2. Ball NJ, Urbanski SJ, Green FH, Kieser T. Pleural multicystic mesothelial proliferation. The so-called multicystic mesothelioma. Am J Surg Pathol. 1990; 14:375–378.
3. Weiss SW, Tavassoli FA. Multicystic mesothelioma. An analysis of pathologic findings and biologic behavior in 37 cases. Am J Surg Pathol. 1988; 12:737–746.
4. Gonzalez-Moreno S, Yan H, Alcorn KW, Sugarbaker PH. Malignant transformation of "benign" cystic mesothelioma of the peritoneum. J Surg Oncol. 2002; 79:243–251.
5. Suh YL, Choi WJ. Benign cystic mesothelioma of the peritoneum: a case report. J Korean Med Sci. 1989; 4:111–115.
6. AbdullGaffar B, Keloth T. Mesoappendiceal and periappendiceal lesions. Pathol Res Pract. 2011; 207:137–141.
7. McFadden DE, Clement PB. Peritoneal inclusion cysts with mural mesothelial proliferation: a clinicopathological analysis of six cases. Am J Surg Pathol. 1986; 10:844–854.
8. Lim SC, Jeong YK, Lee MS, Kim YS, Park HJ, Choi SJ. Benign cystic mesothelioma. Korean J Pathol. 1997; 31:595–597.
9. Letterie GS, Yon JL. The antiestrogen tamoxifen in the treatment of recurrent benign cystic mesothelioma. Gynecol Oncol. 1998; 70:131–133.
10. Park BJ, Alexander HR, Libutti SK, Wu P, Royalty D, Kranda KC, et al. Treatment of primary peritoneal mesothelioma by continuous hyperthermic peritoneal perfusion (CHPP). Ann Surg Oncol. 1999; 6:582–590.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download