Abstract
Purpose
The aim of this study was to retrospectively evaluate the association of need for early relaparotomy with clinical outcomes after elective open repair of abdominal aortic aneurysms (AAAs).
Methods
A total of 292 consecutive patients who underwent elective open AAA repair at Asan Medical Center from January 2001 to December 2010 were included in this study, and we compared the demographics, clinical characteristics, related risk factors, and clinical outcomes of early relaparotomy versus nonrelaparotomy patients.
Results
The incidence of early relaparotomy during a single hospital stay was 4.1% (n = 12), and the most common causes were bowel ischemia (n = 5, 41.7%) and postoperative bleeding (n = 3, 25.0%). Among the demographics and clinical characteristics significantly associated with relaparotomy were: age (P = 0.025), chronic obstructive pulmonary disease (COPD) (P = 0.010), number of RBC units transfused during the AAA repair (P = 0.022) and in the following week (P = 0.005), and length of intensive care (P < 0.001) and overall hospital stay (P < 0.001). On multivariate analysis, presence of COPD (P = 0.009) and number of RBC units transfused during the AAA repair (P = 0.006) were statistically significantly associated with relaparotomy. Furthermore, early relaparotomy was associated with perioperative (within 30 days) (P = 0.048) and overall in-hospital mortality (P = 0.001).
Abdominal aortic aneurysm (AAA) is a degenerative disease that becomes more prevalent with age. Due to the increase in overall life expectancy in developed countries, more and more elderly patients require AAA repair [1]. Open repair of an infrarenal AAA has a considerably higher perioperative mortality rate than endovascular aneurysm repair (EVAR), approximately 5% versus 1%-2% [2,3,4,5]. This has, naturally, increased the popularity of the endovascular approach to elective repair. However, it should be acknowledged that these procedures are performed for different indications (i.e., open AAA repair is performed for aneurysms which are far more anatomically complex), and even in this era of increasing endovascular procedures, most surgeons still perform open repair when the anatomy does not favor the use of EVAR [6,7,8,9]. Although there have been many studies of the factors associated with perioperative mortality in patients undergoing open AAA repair [7,8,9,10,11,12,13], very few have considered whether early relaparotomy is associated with the clinical outcomes.
The aim of our study was to retrospectively evaluate the risk factors and clinical outcomes of early relaparotomy after elective open repair of an AAA.
This was a retrospective, observational study, using data extracted from patients' medical records. The study protocol was approved Asan Medical Center Institutional Review Board (NO. 2014-0065). Between January 2001 and December 2010, a total of 511 consecutive patients underwent an AAA repair at our institution. Of these patients, 137 (26.8%) received EVAR and 374 (73.2%) received open AAA repair. The treatment modality for an AAA repair, whether EVAR or open AAA repair, was determined by the morphology of an AAA based on the preoperative computed tomography angiogram, the patient's comorbidities, and a thorough explanation of the risks and benefits of each treatment modality. Among the 374 patients undergoing open AAA repair, 82 patients (21.9%) with emergency repair of a ruptured AAA were excluded, and a total of 292 patients (78.1%) who underwent an elective open AAA repair were included in this study.
Elective open AAA repair was performed according to accepted guidelines with resection of the aneurysm and graft interposition. Patent internal iliac arteries were retained unless there was severe calcification or aneurysmal change. A patent inferior mesenteric artery was ligated, but it was anastomosed to the graft when ischemia of the sigmoid colon was suspected clinically (pale or pulseless sigmoid colon). The decision whether to give a blood transfusion during the repair was made by the anesthesiologist based on the volume of blood loss and the vital signs. Postoperatively, transfusion was performed when hemoglobin levels fell below 8 g/dL or if bleeding was suspected based on a consistent decrease in hemoglobin or blood pressure. Early relaparotomy was defined as the need for opening of the peritoneum due to any causes located in the abdominal cavity or on the abdominal wall during the patient's hospital stay after open AAA repair. The operating time was calculated from skin incision to closure, and the duration of hospital stay was defined as the time from surgery to discharge. Of the 292 patients, 12 (4.1%) had to undergo early relaparotomy after elective open AAA repair during the same hospital stay. We compared the demographics, clinical characteristics, related risk factors, and clinical outcomes between the early relaparotomy and nonrelaparotomy (control) patients.
We reported categorical data as counts and percentages, and continuous data as means and standard deviations. To compare continuous and categorical variables, we used the Mann-Whitney U test, the chi-square test, or Fisher exact test. Kaplan-Meier estimates of survival together with the log-rank test were used to compare overall survival between the two groups. All reported P-values were two-sided, and P-values <0.05 were considered statistically significant. Statistical analysis was performed with SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA).
Between January 2001 and December 2010, 292 patients underwent open repair of an intact AAA. Of these, 12 patients (4.1%) underwent relaparotomy during the same hospital stay. The patients' demographic and preoperative clinical characteristics are summarized in Table 1. Patient age was the only demographic factor that was significantly different in the relaparotomy and nonrelaparotomy groups (71.7 years vs. 66.9 years, respectively, P = 0.025). Of the preoperative clinical characteristics, only the presence of chronic obstructive pulmonary disease (COPD) was significantly different in the two groups (63.6% vs. 25.3%, relaparotomy vs. control, P = 0.010). Perioperative and postoperative clinical characteristics are summarized in Table 2. The mean number of RBC units transfused during the AAA repair and in the first 7 days after the repair, the mean lengths of intensive care unit (ICU) stay and overall hospital stay, and the perioperative (within 30 days) and overall in-hospital mortality rates were all significantly different between the two groups. The mean number of RBC units transfused during AAA repair was 7.50 in the relaparotomy patients and 3.75 in the nonrelaparotomy patients (P = 0.022), and in the first 7 days after AAA repair, it was 3.17 units vs. 1.02 units, respectively (P = 0.005). The mean length of stay in the ICU was 21.1 days in the relaparotomy patients and 2.6 days in the control group (P < 0.001), and the overall length of hospital stay was 51.6 days in the relaparotomy patients and 10.2 days in the control group (P < 0.001). The perioperative and overall in-hospital mortality rates among all 292 patients were 3.1% and 4.1%, respectively. The perioperative mortality rate was 16.7% in the relaparotomy patients and 2.5% in the controls (P = 0.048), and the overall in-hospital mortality rate was 41.7% in the relaparotomy patients and 2.5% in controls (P = 0.001).
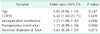
The difference in the mean operating times between the relaparotomy and nonrelaparotomy patients may be clinically significant, although it was not statistically significant (P = 0.092). Maximum diameter of the AAA, use of suprarenal clamping, and postoperative patency of the internal iliac arteries and the inferior mesenteric artery were not significantly different in the two groups. On univariate analysis of risk factors associated with early relaparotomy, increasing age, presence of COPD, and need for RBC transfusions were statistically significantly associated with early relaparotomy (data not shown). On multivariate analysis, presence of COPD (P = 0.009) and number of RBC units transfused during the AAA repair (P = 0.006) were statistically significantly associated with relaparotomy (Table 3).
In our study, two of the 12 patients received several relaparotomies during the patients' hospital stay after open AAA repair; one patient underwent two relaparotomies, and the other underwent three. The mean interval from the AAA repair to the first relaparotomy was 7 days. The causes of relaparotomy are given in Table 4. The most common were bowel ischemia (n = 5, 41.7%) and bleeding (n = 3, 25.0%). During the hospital stay after open repair, there were 5 deaths (41.7%) among the 12 relaparotomy patients and 7 deaths (2.5%) among the 280 control patients (Table 5). In the relaparotomy patients, the causes of death were sepsis (n = 4, 33.3%) and acute respiratory distress syndrome (n = 1, 8.3%). In the nonrelaparotomy group, the causes of death were acute respiratory distress syndrome (n = 3, 1.1%), myocardial infarction (n = 1, 0.4%), and others (n = 3, 1.1%). Patients requiring early relaparotomy had an increased rate of intraoperative and postoperative RBC transfusion, increased length of ICU and hospital stay, and increased mortality.
The Kaplan-Meier analysis showed that the survival rates were significantly different in the two groups (P < 0.001) (Fig. 1). Cumulative patient survival at 1, 2, and 5 years was 50.0%, 40.0%, and 30.0%, respectively, in the relaparotomy patients and 94.3%, 92.0%, and 81.1%, respectively, in the nonrelaparotomy patients.
Open repair of an infrarenal AAA is associated with considerably higher perioperative mortality than EVAR, which has increased the popularity of the endovascular approach for these aneurysms. In our institution, there has also been a dramatic evolution of elective AAA repair from open to EVAR over the course of the study period (from January 2001 to December 2010). During the early study period (from January 2001 to December 2006), only 18 patients received EVAR for an elective AAA repair, whereas 119 patients received EVAR during the late study period (from January 2007 to December 2010). However, open AAA repair is still performed when the anatomy does not favor the use of EVAR. In this study, we evaluated the causes and risk factors of need for early relaparotomy and investigated whether early relaparotomy had any effect on clinical outcomes. We found that increasing age, presence of COPD, number of RBC units transfused during AAA repair and for the first 7 days afterwards, and lengths of ICU stay and overall hospital stay were associated with early relaparotomy after open AAA repair. Furthermore, early relaparotomy was significantly associated with perioperative and overall in-hospital mortality rates.
In previous studies, both patient age and COPD have been linked to poor prognosis after open AAA repair [10,13,14]. Our findings suggest that they could also be risk factors of early relaparotomy. Considering that the relaparotomy patients had higher perioperative and overall mortality rates, it is possible that increasing age and COPD play a role in both. The two groups did not differ significantly in terms of factors that raise the level of difficulty of AAA repair, including maximal AAA diameter, use of suprarenal clamping, and obesity. However, the mean operating time was longer in the relaparotomy patients (not significantly so, but the difference may have had clinical significance). When we compared the numbers of RBC units transfused during and after the AAA repair in the two groups, it was higher in the relaparotomy patients, and it may not be incorrect to assume that relaparotomy is associated with more bleeding complications. Although the exact etiology of postoperative ischemic colitis is not fully understood, it is known that long operating times and large volumes of blood loss are related risk factors [15], and ischemic colitis and bleeding were the main causes of early relaparotomy in our study. Additionally, a much longer ICU and hospital stay was a natural outcome for the relaparotomy patients.
The incidence of ischemic colitis after open repair of an intact AAA varies from 0.6% to 3% [16,17,18], and the perioperative mortality rate due to ischemic colitis is reported to be 40%-60% [15,19,20]. In this study, ischemic colitis, diagnosed by clinical suspicion, computed tomographic scan and/or endoscopic evaluation, was the most common cause of early relaparotomy (n = 6, 50%). Three of the six patients died, mainly of sepsis resulting from ischemic colitis. Postoperative bleeding, the second most common cause of relaparotomy, may be preventable in some cases, and it is critical to minimize such complications to improve the clinical outcomes of open AAA repair.
Although many studies have attempted to identify factors associated with mortality in patients undergoing open AAA repair, and various risk assessment tools have been used to predict perioperative mortality [10,11,12,13], there are few studies investigating whether early relaparotomy can be a significant risk factor to affect the clinical outcome in these patients. In our study, patients requiring relaparotomy had a much higher overall in-hospital mortality rate (41.7% vs. 2.5%, P = 0.001), and lower five-year survival (30.0% vs. 81.1%, P < 0.001) than the control group. Therefore, these findings seem to confirm that need for early relaparotomy has a negative impact on short- and long-term prognosis.
The main limitation of our study was that the relaparotomy group was small and heterogeneous. Relaparotomy has many indications, and the number of cases associated with each of these indications was very small. Further studies with larger numbers and with a multicenter design might be required to confirm our findings.
In summary, early relaparotomy has an adverse effect on clinical outcomes after open repair of intact AAAs: increased mortality and hospital length of stay. Presence of COPD and need for RBC transfusion are associated with early relaparotomy.
Figures and Tables
Fig. 1
Survival of relaparotomy and nonrelaparotomy patients after elective open abdominal aortic aneurysm repair.
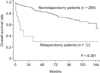
Table 1
Demographic and preoperative clinical characteristics associated with early relaparotomy after open repair of abdominal aortic aneurysm

Table 2
Perioperative and postoperative clinical characteristics associated with early relaparotomy after open repair of abdominal aortic aneurysm

References
1. Henebiens M, Vahl A, Koelemay MJ. Elective surgery of abdominal aortic aneurysms in octogenarians: a systematic review. J Vasc Surg. 2008; 47:676–681.
2. Grant SW, Grayson AD, Purkayastha D, Wilson SD, McCollum C. participants in the Vascular Governance North West Programme. Logistic risk model for mortality following elective abdominal aortic aneurysm repair. Br J Surg. 2011; 98:652–658.
3. Schermerhorn ML, O'Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med. 2008; (358):464–474.
4. Lederle FA, Freischlag JA, Kyriakides TC, Padberg FT Jr, Matsumura JS, Kohler TR, et al. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA. 2009; 302:1535–1542.
5. Mani K, Lees T, Beiles B, Jensen LP, Venermo M, Simo G, et al. Treatment of abdominal aortic aneurysm in nine countries 2005-2009: a vascunet report. Eur J Vasc Endovasc Surg. 2011; 42:598–607.
6. Ramanan B, Gupta PK, Sundaram A, Gupta H, Johanning JM, Lynch TG, et al. Development of a risk index for prediction of mortality after open aortic aneurysm repair. J Vasc Surg. 2013; 58:871–878.
7. Stanley BM, Semmens JB, Mai Q, Goodman MA, Hartley DE, Wilkinson C, et al. Evaluation of patient selection guidelines for endoluminal AAA repair with the Zenith Stent-Graft: the Australasian experience. J Endovasc Ther. 2001; 8:457–464.
8. de la Motte L, Jensen LP, Vogt K, Kehlet H, Schroeder TV, Lonn L. Outcomes after elective aortic aneurysm repair: a nationwide Danish cohort study 2007-2010. Eur J Vasc Endovasc Surg. 2013; 46:57–64.
9. Lo RC, Bensley RP, Hamdan AD, Wyers M, Adams JE, Schermerhorn ML, et al. Gender differences in abdominal aortic aneurysm presentation, repair, and mortality in the Vascular Study Group of New England. J Vasc Surg. 2013; 57:1261–1268. 1268.e1–1268.e5.
10. Dimick JB, Stanley JC, Axelrod DA, Kazmers A, Henke PK, Jacobs LA, et al. Variation in death rate after abdominal aortic aneurysmectomy in the United States: impact of hospital volume, gender, and age. Ann Surg. 2002; 235:579–585.
11. Norman PE, Powell JT. Abdominal aortic aneurysm: the prognosis in women is worse than in men. Circulation. 2007; 115:2865–2869.
12. Dimick JB, Cowan JA Jr, Stanley JC, Henke PK, Pronovost PJ, Upchurch GR Jr, et al. Surgeon specialty and provider volumes are related to outcome of intact abdominal aortic aneurysm repair in the United States. J Vasc Surg. 2003; 38:739–744.
13. Koskas F, Kieffer E. Association for Academic Research in Vascular Surgery (AURC). Long-term survival after elective repair of infrarenal abdominal aortic aneurysm: results of a prospective multicentric study. Ann Vasc Surg. 1997; 11:473–481.
14. Stone DH, Goodney PP, Kalish J, Schanzer A, Indes J, Walsh DB, et al. Severity of chronic obstructive pulmonary disease is associated with adverse outcomes in patients undergoing elective abdominal aortic aneurysm repair. J Vasc Surg. 2013; 57:1531–1536.
15. Biros E, Staffa R. Incidence and risk factors of ischemic colitis after AAA repair in our cohort of patients from 2005 through 2009. Rozhl Chir. 2011; 90:682–687.
16. Van Damme H, Creemers E, Limet R. Ischaemic colitis following aortoiliac surgery. Acta Chir Belg. 2000; 100:21–27.
17. Papia G, Klein D, Lindsay TF. Intensive care of the patient following open abdominal aortic surgery. Curr Opin Crit Care. 2006; 12:340–345.
18. Bjorck M, Bergqvist D, Troeng T. Incidence and clinical presentation of bowel ischaemia after aortoiliac surgery--2930 operations from a population-based registry in Sweden. Eur J Vasc Endovasc Surg. 1996; 12:139–144.
19. Conrad MF, Crawford RS, Pedraza JD, Brewster DC, Lamuraglia GM, Corey M, et al. Long-term durability of open abdominal aortic aneurysm repair. J Vasc Surg. 2007; 46:669–675.
20. Kim H, Kwon TW, Cho YP, Moon KM. Report of a case of ischemic colitis with bilaterally patent internal iliac arteries after endovascular abdominal aneurysm repair. J Korean Surg Soc. 2012; 82:200–203.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download