Abstract
Purpose
Preformed circulating donor-specific antibodies (DSAs) immunologically challenge vascular endothelium and the bile duct. However, the liver is an immune-tolerant organ and can avoid immunological challenges. This study was undertaken to analyze the effects of DSAs after adult living donor liver transplantation (LDLT).
Results
Of the 219 patients, 32 (14.6%) were DSA (+) and 187 (85.4%) were DSA (-). Class I DSAs were present in 18 patients, class II in seven patients, and both in seven patients. Seven patients (3.2%) showed DSA to HLA-A, four (1.8%) to HLA-B, seven (3.2%) to HLA-DR, and 14 (6.4%) to two or more HLAs. More DSAs were observed in female recipients than male recipients in the DSA (+) group. The DSA (+) group showed significantly higher levels of class I and II panel reactive antibody (PRA) than did the DSA (-) group. No significant intergroup differences were found between incidences of primary nonfunction, acute rejection, vascular complication, or biliary complication. There were no significant differences in graft survival rates between the two groups. However, the recipients with multiple DSAs tended to have more acute rejection episodes and events of biliary stricture and lower graft survival rates than did patients in the DSA (-) group.
Highly sensitized organ recipients are at greater risk of acute rejection, vascular complications, and poor graft survival [1,2,3]. Circulating donor-specific antibodies (DSAs) immunologically challenge the vascular endothelium and bile duct [4], but the liver is uniquely able to neutralize antibodies and escape from immunologic challenges [5,6]. However, the effects of DSAs on graft function and survival after liver transplantation remains controversial. Some authors suggest that a positive T lymphocyte cross match results in poor graft survival and more acute rejection [7,8], whereas others conclude that a positive T lymphocyte cross match has no effect on graft outcome [9,10]. Additionally, the role of circulating preformed DSAs before liver transplantation is unclear. Consequently, the aim of this study was to determine if preformed circulating DSAs negatively affect graft outcome after living donor liver transplantation (LDLT).
The medical records of 219 adult LDLT patients that underwent treatment at Yonsei University College of Medicine between June 2006 and August 2012 were retrospectively reviewed. Pediatric and second transplant cases were excluded. Patients were allocated to two groups according to the presence of DSA. DSAs were identified by panel reactive antibody (PRA) identification conducted by ELISA using the Lambda Cell Tray lymphocytotoxicity assay (One Lambda Inc., Canoga Park, CA, USA). Records were reviewed for clinical and immunological characteristics, acute rejection episodes, complications, and graft survival.
The primary immunosuppressive therapy used posttransplant was a tacrolimus-based agent. Induction therapy with interleukin-2 receptor antibody (basiliximab) was used, except in cases with identical HLA matching. Antimetabolite was used depending on patient condition and side effects after transplantation.
Continuous variables are presented as mean ± standard deviation and were analyzed using the two-tailed Student t-test or analysis of variance. Categorical variables, presented as proportions, were analyzed using Fisher exact test. Graft survival rates were calculated using the Kaplan-Meier method and compared among the groups using the log-rank test. Cox regression analysis was used to evaluate risk factors for graft survival. P-values of <0.05 were considered significant.
The mean follow-up time for the 219 study subjects was 28.3 ± 23.6 months posttransplantation. Mean patient age was 52.4 ± 7.7 years and there were 170 male and 49 female recipients. Liver transplantation indications consisted of 60 cases of B-viral cirrhosis (27.4%), 4 of C-viral cirrhosis (1.8%), 16 of alcoholic cirrhosis (7.3%), 4 of autoimmune cirrhosis (1.8%), 3 of cryptogenic cirrhosis (1.4%), 1 of primary biliary cirrhosis (0.5%), 1 of primary sclerosing cholangitis (0.5%), 2 of metabolic liver disease (0.9%), 6 of acute liver failure (2.7%), 1 of other cirrhosis (0.5%), and 121 cases of hepatocellular carcinoma (55.3%).
Among the 219 recipients, 32 recipients (14.5%) were positive for DSAs against donor HLAs by PRA. Of these 32 DSA positive (DSA (+)) recipients, DSAs for HLA class I (HLA A- or B-) were detected in 25 patients, DSAs for HLA class II (HLA DR-) in 14 patients, and DSAs for both HLA class I and II in seven recipients. Of the 32 DSA (+) patients, 7 recipients had a single DSA for HLA-A (21.9%), 4 showed a single DSA for HLA-B (12.5%), 7 showed a single DSA for HLA-DR (21.9%), and 14 showed two or more DSAs (43.7%), referred to as multiple DSA.
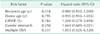
According to the presence of DSAs, patients were divided into two groups, DSA (+) and DSA (-). There were more female patients in the DSA (+) group than in the DSA (-) group (59.4% vs. 16.0%). T lymphocyte cross match positivity was more common in the DSA (+) group (28.1% vs. 3.2%), and the proportions of PRA class I and II were higher in the DSA (+) group. Other nonimmunologic factors, such as recipient age, model for endstage liver disease score, and donor-recipient relationship were similar between the two groups. In reviewing posttransplant complications, no significant intergroup differences were found for acute rejection episodes, primary non-function, vascular complications, or biliary complications (Table 1).
Recipients were subdivided into the following subgroups by type of DSA for HLA; the DSA (-) group, single DSA groups for HLA-A, -B, or -DR, and a multiple DSA group. Acute rejection, vascular complications, and biliary complications occurred at similar levels in these groups. However, the multiple DSA group had more acute rejection episodes and biliary anastomotic strictures than the other groups (Table 2); although, this was not statistically significant.
Graft survival rates were not significantly different between the DSA (-) and (+) groups. One-year survivals in the DSA (-) and DSA (+) groups were 97.9 and 90.4%, respectively. Three-year survival rates between DSA (-) and DSA (+) were 86.5% and 85.7%, respectively (Fig. 1A). However, in the subgroup analysis, the multiple DSA group showed a lower graft survival rate than the DSA (-) or single DSA group, although this result was not statistically significant. One-year survival rates in the DSA free or single DSA group and multiple DSA group were 91.4% and 85.7%, respectively, and corresponding 3-year survival rates were 85.8% and 75.0%, respectively (Fig. 1B). We divided all recipients into three groups; PRA < 10%, PRA 10%-30%, and PRA ≥ 30%. PRA class II ≥ 30% group showed worse graft survival rate than other groups but there was no significant difference among the group according to PRA class I and II. However, if the PRA percentages of class I and II were summed, PRA ≥ 30% group showed poorer graft survival rates than PRA 10%-30% group (Fig. 2).
Recipient and donor age, graft to recipient weight ratio, gender mismatch, and multiple DSAs were analyzed as the risk factors for long-term graft survival. Cox regression analysis showed that there was no significant hazard ratio among the parameters (Table 3).
The liver is well known for its immune tolerance [11], and as such, liver transplantations have been performed on patients positive with a T lymphocyte cross match, with a HLA mismatch, and even patients with multiple DSAs [2,9]. Recently, Taner et al. [6] reported that DSA levels decreased at 1 week after liver transplantation in 17 of 20 recipients with pretransplant DSAs. Furthermore, they indicate that transaminase and bilirubin levels remain comparable during the first post-transplant year despite the presence of DSAs.
Conversely, some reports show that HLA mismatch and DSAs cause poor graft survival and more acute rejection episodes [12,13]. Everly [14] suggested that all patients need to be monitored for DSA to identify new onset DSA or DSA clearance, and stressed that in all DSA scenarios, the treatment of persistent DSA is important, as it can improve allograft survival. In the current study, although statistical significance was not obtained, our results suggest that recipients with pretransplant multiple DSAs tend to have poorer graft outcomes than those with absent or single DSA, and that highly sensitized recipients should be monitored for antibody status after transplantation. Furthermore, we found that patients who had high class II PRA (≥30%) showed worse graft survival rates than those with lower class II PRA. Recent studies demonstrate that class II DSAs are associated with an increased risk of early rejection [15,16]. Our results suggest that class II DSAs may be more potent than class I DSAs.
Given that this is a retrospective study, there are several limitations inherent to this work. In particular, a relatively small number of patients were enrolled and no data was available regarding DSA status after liver transplantation. Because of the small number of patients, there were no significant risk factors for long-term graft survival in Cox regression analysis. Taner et al. [6] reported that the preformed DSA decreased after liver transplantation but remaining DSA affected the graft liver to a poor graft survival; however, this study did not show any posttransplant change of DSAs. Further study is needed to clarify the findings reported herein.
We did not perform a single antigen assay for detecting DSA and measurement of mean fluorescence intensity. Recent studies regarding DSA in liver transplantation show that high mean fluorescence intensity is related to poor graft outcomes and early acute rejection after liver transplantation [15,16]. The present study had no data regarding the mean fluorescence intensity of the DSA but showed that the number of DSAs is related with acute rejection and poor graft survival after liver transplantation. We suggest that not only the mean fluorescence intensity of DSA, but also the number of DSAs can be an important prognostic factor in LDLT.
Despite the limitations, this current study is important because it is the first to focus on DSA numbers in LDLT. Furthermore, the study was conducted on LDLTs from strictly selected donors who exhibited relatively homogenous nonimmunologic conditions. The study design excluded various deceased donor factors such as ischemic time, steatosis, and age, which could themselves cause poor graft outcomes.
A recent study showed that de novo DSA development after liver transplantation was an independent risk factor for poor graft outcomes [17]. They found that 8.1% of patients developed de novo DSA 1 year after transplantation, and almost all de novo DSAs were HLA class II antibodies. This result implies that we should carefully monitor not only pretransplant DSA but also DSA development status after liver transplantation. However, there was no definite follow-up protocol for de novo DSA after liver transplantation. In the current study, we showed multiple DSAs and high PRA over 30% could make for a worse prognosis than in other recipients. We carefully suggest that this kind of highly-sensitized recipient should be monitored for de novo DSA development within one year after transplantation. To make evidences, further studies will be needed.
The present study showed that in LDLT, the presence of multiple DSAs and high PRA seem to be associated with poor graft outcomes, although our results did not reach statistical significance. Large cohort studies including mean fluorescence intensity (MFI) strength of each DSA are needed to clarify the role of pretransplant DSAs and PRA after LDLT.
Figures and Tables
Fig. 1
Graft survival rates according to the presence of donor-specific antibodies. (A) No difference in graft survival rates was found between the DSA (-) and (+) groups. (B) However, patients with multiple DSAs had a lower graft survival rate than patients in none or single DSA group. DSA, donor-specific antibody.

Fig. 2
Graft survival rates according to the percentage of panel reactive antibody (PRA). (A) Graft survival rates of the PRA ≥30% group were lower than the PRA 10%-30% group (P = 0.038) according to the sum of PRA percentage. No significant differences in graft survival rates were found among the PRA percentage groups according to the PRA classes I and II (B and C). However, class II showed more intervals among the groups.

Table 1
Clinical characteristics and outcomes according to the presence of donor-specific antibodies

ACKNOWLEDGEMENTS
This work was supported by a research grant from the Research Institute for Transplantation, Yonsei University College of Medicine (2012-2013).
References
1. Hori T, Uemoto S, Takada Y, Oike F, Ogura Y, Ogawa K, et al. Does a positive lymphocyte cross-match contraindicate living-donor liver transplantation? Surgery. 2010; 147:840–844.
2. Suehiro T, Shimada M, Kishikawa K, Shimura T, Soejima Y, Yoshizumi T, et al. Influence of HLA compatibility and lymphocyte cross-matching on acute cellular rejection following living donor adult liver transplantation. Liver Int. 2005; 25:1182–1188.
3. Ratner LE, Hadley GA, Hanto DW, Mohanakumar T. Immunology of renal allograft rejection. Arch Pathol Lab Med. 1991; 115:283–287.
4. Abu-Elmagd KM, Wu G, Costa G, Lunz J, Martin L, Koritsky DA, et al. Preformed and de novo donor specific antibodies in visceral transplantation: long-term outcome with special reference to the liver. Am J Transplant. 2012; 12:3047–3060.
5. Pons JA, Revilla-Nuin B, Ramirez P, Baroja-Mazo A, Parrilla P. Development of immune tolerance in liver transplantation. Gastroenterol Hepatol. 2011; 34:155–169.
6. Taner T, Gandhi MJ, Sanderson SO, Poterucha CR, De Goey SR, Stegall MD, et al. Prevalence, course and impact of HLA donor-specific antibodies in liver transplantation in the first year. Am J Transplant. 2012; 12:1504–1510.
7. Sugawara Y, Makuuchi M, Kaneko J, Kishi Y, Hata S, Kokudo N. Positive T lymphocytotoxic cross-match in living donor liver transplantation. Liver Transpl. 2003; 9:1062–1066.
8. Suh KS, Kim SB, Chang SH, Kim SH, Minn KW, Park MH, et al. Significance of positive cytotoxic cross-match in adult-to-adult living donor liver transplantation using small graft volume. Liver Transpl. 2002; 8:1109–1113.
9. Joo DJ, Ju MK, Huh KH, Kim MS, Choi GH, Choi JS, et al. Does lymphocyte cross-matching predict acute rejection and graft survival in liver transplantation? Transplant Proc. 2012; 44:418–420.
10. Matinlauri IH, Hockerstedt KA, Isoniemi HM. Equal overall rejection rate in pretransplant flow-cytometric cross-match negative and positive adult recipients in liver transplantation. Clin Transplant. 2005; 19:626–631.
11. Heeger PS, Dinavahi R. Transplant immunology for non-immunologist. Mt Sinai J Med. 2012; 79:376–387.
12. Wiesner RH, Demetris AJ, Belle SH, Seaberg EC, Lake JR, Zetterman RK, et al. Acute hepatic allograft rejection: incidence, risk factors, and impact on outcome. Hepatology. 1998; 28:638–645.
13. Lan X, Zhang MM, Pu CL, Guo CB, Kang Q, Li YC, et al. Impact of human leukocyte antigen mismatching on outcomes of liver transplantation: a meta-analysis. World J Gastroenterol. 2010; 16:3457–3464.
14. Everly MJ. Donor-specific anti-HLA antibody monitoring and removal in solid organ transplant recipients. Clin Transpl. 2011; 319–325.
15. O'Leary JG, Klintmalm GB. Impact of donor-specific antibodies on results of liver transplantation. Curr Opin Organ Transplant. 2013; 18:279–284.
16. O'Leary JG, Kaneku H, Jennings LW, Bañuelos N, Susskind BM, Terasaki PI, et al. Preformed class II donor-specific antibodies are associated with an increased risk of early rejection after liver transplantation. Liver Transpl. 2013; 19:973–980.
17. Kaneku H, O'Leary JG, Banuelos N, Jennings LW, Susskind BM, Klintmalm GB, et al. De novo donor-specific HLA antibodies decrease patient and graft survival in liver transplant recipients. Am J Transplant. 2013; 13:1541–1548.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download