Abstract
Intraperitoneal bleeding after radiofrequency ablation (RFA) is the most common major vascular complication due to direct needle injury to a vessel or liver capsule. However, intraperitoneal bleeding as a result of a delayed hepatic rupture after RFA for liver tumors is an extremely rare complication. The present report describes a case of intraperitoneal hemorrhage caused by delayed hepatic rupture resulting from arterioportal fistula after RFA for hepatic metastasis from colorectal cancer and successful management using transcatheter embolization.
The liver is the most common site of distant metastasis in colorectal cancer and 50% of all patients with colon cancer ultimately develop liver involvement [1]. Surgical resection is the most effective treatment for colorectal metastases confined to the liver. However, only up to 20% of patients are candidates for hepatic resection [2]. Radiofrequency ablation (RFA) is a well established minimally invasive treatment option for patients with inoperable hepatic metastasis from colon cancer [3] and can be performed safely using percutaneous or intraoperative techniques. However, various complications including hemorrhage, abscess, and collateral thermal damage have been reported [4]. Among these, intraperitoneal bleeding is the most common complication after RFA and most bleeding stops spontaneously [4]. As far as we know, this is the first report presented of delayed hepatic rupture caused by arterioportal (AP) fistula after RFA. We report a case of intraperitoneal bleeding due to delayed hepatic rupture after RFA for hepatic metastasis from colorectal carcinoma and successful management for the perihepatic hemorrhage and AP fistula using transcatheter embolization.
A 57-year-old man was referred to Department of Radiology for intraoperative RFA of a 2.6-cm-sized hepatic metastasis from colorectal cancer. Contrast enhanced abdominal CT showed a peripheral rim enhanced hypodense mass in segment VII of the liver (Fig. 1A). Percutaneous liver biopsy was performed before surgical procedure and the liver mass was confirmed as a metastatic adenocarcinoma. His aspartate aminotransferase level in the morning of operation day was 457 IU/L (normal, <38 IU/L), alanine aminotransferase, 182 IU/L (normal, <43 IU/L), alkaline phosphatase, 93 IU/L (normal, <129 IU/L), total bilirubin, 0.8 mg/dL (normal <1.2 mg/dL), albumin, 3.0 g/dL (3.3 g/dL<normal<5.3 g/dL). He underwent low anterior resection for rectal cancer and intraoperative RFA for hepatic metastasis, because of abnormal liver function. A clustered internally cooled electrode with a 2.5-cm active tip (Cool-tip, Valleylab, Boulder, CO, USA) was used for the hepatic tumor ablation. To achieve adequate ablated margin, two overlapping ablations were applied for 10 minutes and 8 minutes, respectively. At the end of the procedure, tract ablation was performed to prevent bleeding and tumor seeding. Abdominal follow-up CT the next day showed complete ablation with adequate ablated margin, yet a 2.3-cm-sized liver laceration and intrahepatic hematoma was suspected (Fig. 1B). At 6 days after intraoperative RFA, he complained of mild abdominal pain and severe watery diarrhea. Additional abdominal follow-up CT showed more extensive liver laceration and pseudoaneurysm abutting the 1st order branch of the portal vein in segment V (Fig. 1C). The next morning, the patient developed a sudden abdominal right upper quadrant pain. Blood pressure was 109/72 mmHg and the pulse rate, 88 beats/min. Hemoglobin levels dropped from 11.9 to 8.9 g/dL for three hours. Contrast enhanced abdominal CT revealed more extensive liver laceration, hepatic rupture and perihepatic hemorrhage (Fig. 1D). While the patient received 4 units of packed red blood cells and 2 units of fresh frozen plasma, we decided to perform embolization to prevent further intraperitoneal hemorrhage. For local anesthesia, right common femoral artery access was obtained using a micropuncture set and a 5-French introducer sheath (Radiofocus Introducer II, Terumo, Tokyo, Japan) was placed. Celiac trunk angiography was undertaken using a 5-French Rösch hepatic catheter (Cook, Bloomington, IN, USA) and showed massive AP fistula with contrast extravasation (Fig. 2A). Superselective catheterization of the hepatic artery in liver segment VI was performed using a 2.0-French microcatheter (Progreat, Terumo). Superselective angiography revealed massive AP fistula. Massive AP fistula was embolized with three platinum coils with synthetic fiber (Tornado, Cook) and absorbable gelatin sponge particles (1-2 mm in diameter; Gelfoam, Upjohn, Kalamazoo, MI, USA). Completion angiography showed occluded AP fistula without contrast extravasation (Fig. 2B). After the procedure, no more active bleeding signs were observed. The patient did not have clinical symptoms during 1-year follow-up without radiological evidence of tumor recurrence.
RFA has been mainly used in patients with nonresectable colorectal hepatic metastasis because of survival benefits, safety, and low complication rate [3]. Even though satisfactory results can be obtained with RFA, it can also be associated with adverse events. One of the most common complications of RFA is intraperitoneal hemorrhage resulting from direct needle injury to a vessel. Although most hemorrhage from the RFA needle tract tends to be self-limiting, transarterial embolization or surgical interruption may be required in case of arterial bleeding or AP fistula [4,5]. In most cases, vascular complications including arterial bleeding, pseudoaneurysm, and arteriovenous fistula occurs immediately after procedure and can be prevented by cauterization of the needle tract at the end of the ablation session [6]. Conservative management may be appropriate if the patient's condition is stable and liver capsule is intact.
However, delayed hepatic rupture after RFA is an extremely rare complication causing fatal consequences. Kaplan et al. [7] explained the mechanism of late hepatic rupture, which is attributed to the clot breakdown into hyperosmolar fluid, with more fluid absorbed, increasing the size and pressure within the injured liver parenchyma until a breaking point is reached, tearing the tissue and causing bleeding. Additional possible mechanisms can be explained in our case by gradual progression of intrahepatic laceration with hematoma from direct penetrating arteriovenous injury. Although most of the blood from injured hepatic artery passes through the portal vein, some might burrow into the hepatic parenchyma, causing intrahepatic laceration and delayed hepatic rupture.
Iatrogenic AP fistula can be managed by surgical treatment or hepatic arterial embolization. Curley et al. [5] reported that an AP fistula and pseudoaneurysm were noted on a CT scan 6 weeks and 3 months after RFA, respectively, and treated successfully with a transarterial coil embolization to prevent bleeding into RFA cavity.
Our report showed a delayed hepatic rupture combined with AP fistula one week after RFA for hepatic metastasis from colorectal carcinoma and successful endovascular treatment. Since iatrogenic AP fistula after RFA or needle biopsy is considered a minor complication, the patient is discharged a few days later if there is no symptom. However, if hepatic vascular and parenchymal injuries are suspected on follow-up CT after RFA, the patient should be closely monitored by radiologic examination to allow early detection of changes indicating the development of possible delayed complications. Patient should not be discharged before the radiologic imaging findings of damaged structures are stabilized. If the patient shows progressive hepatic laceration or severe vessel damages, transcatheter hepatic arterial embolization can be an appropriate treatment option.
Figures and Tables
Fig. 1
Serial changes of intrahepatic laceration and hematoma after radiofrequency ablation (RFA). (A) Abdominal computed tomography (CT) axial image before surgery shows 2.6-cm-sized peripherally rim enhanced hypodense mass in segment VII of liver (arrow). (B) Abdominal CT axial image one day after intraoperative RFA shows 2.3-cm-sized intrahepatic laceration and hematoma (arrow) in Couinaud segment V. (C) Abdominal CT coronal image seven days after intraoperative RFA shows pseudoaneurysm (arrow) abutting 1st order branch of portal vein in segment V. (D) Abdominal CT axial image eight days after intraoperative RFA shows hepatic rupture and intraperitoneal hemorrhage (arrow).
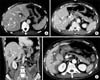
Fig. 2
Arterioportal fistula due to radiofrequency ablation, closed with coils and gelfoam. (A) Celiac arteriogram demonstrates early opacification of portal vein in segment V (arrowheads) and contrast extravasation (arrow). (B) Celiac arteriogram after embolization with coils (arrow) demonstrates no further arterioportal fistula and contrast extravasation.

References
1. Wu YZ, Li B, Wang T, Wang SJ, Zhou YM. Radiofrequency ablation vs hepatic resection for solitary colorectal liver metastasis: a meta-analysis. World J Gastroenterol. 2011; 17:4143–4148.
2. Bismuth H, Adam R, Levi F, Farabos C, Waechter F, Castaing D, et al. Resection of nonresectable liver metastases from colorectal cancer after neoadjuvant chemotherapy. Ann Surg. 1996; 224:509–520.
3. Gillams AR, Lees WR. Radiofrequency ablation of colorectal liver metastases. Abdom Imaging. 2005; 30:419–426.
4. Rhim H. Complications of radiofrequency ablation in hepatocellular carcinoma. Abdom Imaging. 2005; 30:409–418.
5. Curley SA, Marra P, Beaty K, Ellis LM, Vauthey JN, Abdalla EK, et al. Early and late complications after radiofrequency ablation of malignant liver tumors in 608 patients. Ann Surg. 2004; 239:450–458.
6. Rhim H, Dodd GD 3rd, Chintapalli KN, Wood BJ, Dupuy DE, Hvizda JL, et al. Radiofrequency thermal ablation of abdominal tumors: lessons learned from complications. Radiographics. 2004; 24:41–52.
7. Kaplan U, Hatoum OA, Chulsky A, Menzal H, Kopelman D. Two weeks delayed bleeding in blunt liver injury: case report and review of the literature. World J Emerg Surg. 2011; 6:14.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download